The Elbow
Roger L. McCoy II
C. Edward Clark III
Anatomy/Biomechanics
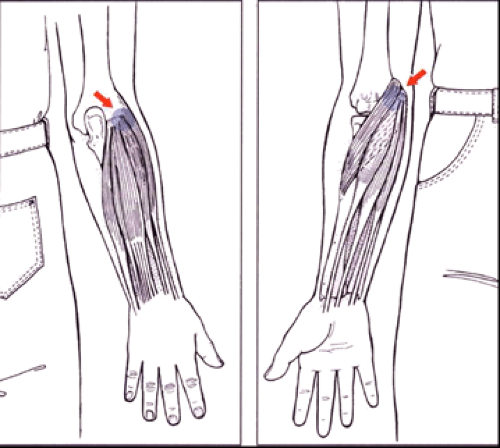
The bony anatomy consists of the distal humerus, which has the trochlea medially and the capitellum laterally. The radial head articulates with the capitellum and the proximal ulna articulates with the trochlea. The humeroradial joint is a uniaxial diarthrodial joint that functions as a hinge for flexion and extension and as a pivot in the longitudinal axis to allow rotational motion. The medial humeral epicondyle serves as the origin of the flexor–pronator muscle (FPM) group and the medial ulnar collateral ligament (UCL) (see Figure 26.1, Table 26.1). The lateral epicondyle serves as the origin of the extensor–supinator muscle group and the radial and lateral UCL (see Figure 26.1, Table 26.2) (1,2).
The elbow joint comprises three articulations: the ulnohumeral, the radiocapitellar, and the proximal radioulnar joint. These allow the elbow two degrees of freedom: flexion–extension and pronation–supination. The normal elbow moves from 0 degree to 135–150 degrees of flexion and possesses approximately 70 to 90 degrees of pronation and 80 to 90 degrees of supination. The normal carrying angle of the extended elbow is approximately 15 degrees of valgus in relation to the humeral shaft (11–14 degrees in men, 13–16 degrees in women) (see Figure 26.2) (3,4).
The medial and radial collateral ligaments, the closely matching bony surfaces, the joint capsule, and the surrounding muscles provide stability to the elbow. The primary structure providing valgus stability is the medial collateral ligament complex, which consists of three portions: the anterior oblique, posterior oblique, and a transverse intervening portion. The anterior oblique portion of the medial collateral ligament is the primary valgus stabilizer of the elbow (see Figures 26.3 and 26.4) (1,4).
Elbow Injuries
Obtaining a thorough history is essential in arriving at the correct diagnosis in the athlete who presents with elbow pain. Determining the onset of pain, whether acute or chronic, the mechanism of injury, the exact location, exacerbating factors, and quality, intensity, and radiation of the patient’s pain is important in establishing an accurate differential diagnosis. Associated symptoms, such as muscle weakness, numbness, clicking, catching, and locking of the joint, as well as neck, shoulder, wrist, and hand complaints, are also important in the history acquisition. The level and magnitude of competition of the athlete is also important to note; because this may direct modes and aggressiveness of treatment in the use of diagnostic studies. Earlier injuries and treatment protocols may also help in determining diagnostic and treatment strategies (2).
It may also help to organize the symptoms to coincide with a particular area of the elbow anatomy. Certain diagnoses are unique not only in their symptomatology, but also in their location. Not all conditions listed will be specifically addressed in this chapter as they may be readily found in many other texts (see Table 26.3) (5).
General Physical Examination
The physical examination of any joint is best done in the order of inspection, palpation, range of motion (ROM), and then stability/provocative maneuvers. This order minimizes patient discomfort early in the examination, which can minimize guarding. Inspection should preferably start with the patient standing, and any clothing covering the shoulder and arm should be removed. The examiner should observe the carrying angle (see section “Anatomy/Biomechanics”), color, size, and note
any swelling, ecchymosis, or obvious signs of trauma. General size differences could be from normal muscle hypertrophy expected in certain athletes (pitchers, racquet sports), while atrophy should be considered abnormal. Posterior swelling could represent olecranon bursitis or joint effusion (2).
any swelling, ecchymosis, or obvious signs of trauma. General size differences could be from normal muscle hypertrophy expected in certain athletes (pitchers, racquet sports), while atrophy should be considered abnormal. Posterior swelling could represent olecranon bursitis or joint effusion (2).
The examiner begins palpation away from the patient’s reported point of maximal tenderness when possible, noting any pain, crepitus, or other deformity. Palpation should begin posteriorly over the distal humerus and move towards the olecranon, while addressing any tenderness of the supracondylar region and the triceps tendon. Olecranon palpation can be assisted by placing the joint in slight flexion to free it from the olecranon fossa. A chronically enlarged olecranon bursa is not usually tender, but may be tender if infected or acutely inflamed from an injury. Proceeding laterally from the olecranon one finds the lateral epicondyle, and 1 to 2 cm more distally is the radial head. The radial head articulation can be easily found by pronating and supinating the forearm while palpating just distal to the lateral epicondyle. An effusion can be palpated in an imaginary triangle defined by the olecranon tip, lateral epicondyle, and radial head while the elbow is flexed to 90 degrees. Next palpate the medial epicondyle. The ulnar nerve sits posterior to the medial epicondyle, between it and the olecranon in the groove for the ulnar nerve (2,6,7).
TABLE 26.1 Flexor-Pronator Muscle Group | |||||
|---|---|---|---|---|---|
|
TABLE 26.2 Mobile Wad Extensors (Extensor-Supinator Group) | |||||
|---|---|---|---|---|---|
|
ROM should be first evaluated passively then actively, including flexion, extension, pronation and supination (see section “Anatomy/Biomechanics” for normal ranges). While checking the ROM one should note any ulnar nerve subluxation by flexing the elbow to 50 to 60 degrees, while placing the shoulder in slight external rotation and palpating over the ulnar nerve. During subluxation the nerve may “roll up” onto the epicondyle (2).
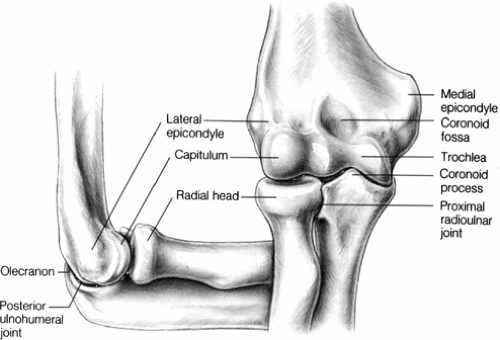 Figure 26.3 Bony anatomy of the elbow. (Source: Adapted from Chumbley E, O’Connor FG, Nirschl RP. Evaluation of overuse elbow injuries. Am Fam Physician 2000; 61:691–700. ) |
Stability of the medial or UCL is assessed by placing a valgus stress to the elbow and is explained in detail later in this chapter (see Figure 26.5). Radial collateral ligament stability is assessed in a similar manner with varus stressing. These and other specific maneuvers is discussed later in the chapter (5).
General Radiographic Principles
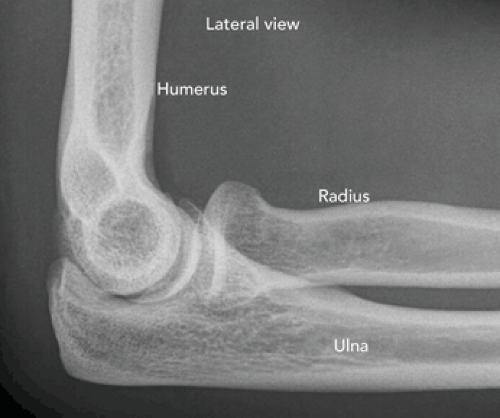
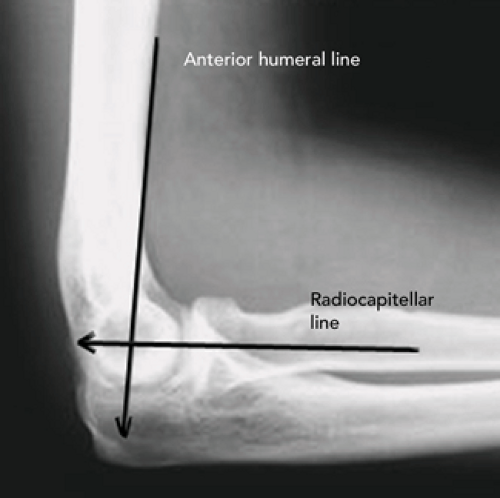
A standard elbow series includes an anteroposterior (AP) view in full extension (see Figure 26.6) and lateral view at 90 degrees (see Figure 26.7) of flexion. Two lines should be drawn in cases of trauma or when fracture is suspected. The anterior humeral line is drawn on the lateral view, parallel and along the anterior surface of the humeral cortex (see Figure 26.8). If the line does not transect the middle third of the mid capitellum, then a supracondylar fracture should be suspected. The radiocapitellar line can also be helpful in detecting pathology. It is drawn through the center of the radial head and neck and extended proximally (see Figure 26.8). Normally it extends in all views through the midcapitellum. Dislocation of the radial head is suspected if the line does not transect this region, or if there is relative movement of the capitellum from a supracondylar fracture (7,8).
The presence of two fat pads in the elbow are also helpful in detecting pathology. The anterior fat pad is located just anterior to the distal humeral diaphysis and can be seen in a normal elbow series as a small line or triangular radiolucency. The posterior fat pad is usually not visible because it lies in the olecranon fossa. Effusion from intra-articular bleeding or inflammation can elevate
these fat pads away from the cortex and either make them larger or visible. The anterior fat pad makes a “sail sign” when elevated (see Figure 26.9). Any presence of a posterior fat pad is abnormal and suggests fracture (see Figure 26.9) (7,8,9).
these fat pads away from the cortex and either make them larger or visible. The anterior fat pad makes a “sail sign” when elevated (see Figure 26.9). Any presence of a posterior fat pad is abnormal and suggests fracture (see Figure 26.9) (7,8,9).
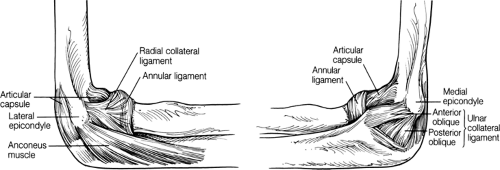 Figure 26.4 Ligamentous support of the elbow. (Source: Adapted from Chumbley E, O’Connor FG, Nirschl RP. Evaluation of overuse elbow injuries. Am Fam Physician 2000; 61:691–700. ) |
TABLE 26.3 Differential Diagnosis of Elbow Pain by Symptom Location | ||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||||||||||||||||||||||||
Acute Trauma
Any athlete presenting with significant pain around the elbow resulting from an acute event should be carefully evaluated to rule out a fracture or dislocation. The athlete should be removed from competition, and all equipment, tape, and padding from the shoulder to the hand should be removed so that an adequate examination can be performed. This is, of course, if it is safe and timely to do so. Tenderness, swelling, and ecchymosis should be noted. Any findings of bony crepitus or deformity warrants high suspicion of a fracture. The shoulder, forearm, wrist, and hand should be carefully and expediently examined. A thorough neurovascular examination of the median, ulnar, and radial nerves and pulses is essential. Sensory testing of peripheral nerves should include the first web space on the dorsum of the hand (radial nerve), volar tip of the index finger (median nerve), and volar tip of the small finger (ulnar nerve). Any deficiencies need to be noted and charted, as chronic sequelae may arise that may be directly related to the trauma as opposed to the physicians treatment (6,9,10).
Motor examination includes testing the extensor pollicis longus for interphalangeal joint extension of the thumb (radial nerve), the index flexor digitorum profundus for flexion at the distal interphalangeal joint (median nerve), and the dorsal interossei and abductor digiti quinti muscles
of the index and small fingers for abduction strength (ulnar nerve). The vascular examination is also essential in any trauma. Brachial, radial, and ulnar pulses need be checked immediately and any question of compromise considered an emergency situation. ROM at the elbow, including pronation and supination, should be carefully checked and recorded (6,7).
of the index and small fingers for abduction strength (ulnar nerve). The vascular examination is also essential in any trauma. Brachial, radial, and ulnar pulses need be checked immediately and any question of compromise considered an emergency situation. ROM at the elbow, including pronation and supination, should be carefully checked and recorded (6,7).
With an elbow trauma that is accompanied by any abnormal findings on physical examination, plain radiographs are warranted. Good quality AP and lateral radiographs are necessary to rule out occult fractures, especially those involving the radial head. A positive “fat pad” sign or “sail” sign (see Figure 26.9) on the posterior aspect of the humerus indicates an effusion within the joint and may be associated with a fracture. Any fracture should be appropriately immobilized with a well-padded posterior splint (6,7,11).
Fractures and Dislocations of the Elbow
Fractures or dislocations of the elbow do occur during athletic competition, especially in contact sports, and knowledge of the initial evaluation and management of these injuries is essential for the team physician. Elbow trauma includes fractures of the distal humerus, radial head and neck fractures, olecranon fractures, simple elbow dislocations, and fracture-dislocations of the elbow. Generally, most fracture patients can start rehabilitation at 6 to 8 weeks postinjury if good callous formation is present, and can expect return to play at 12 weeks. Simple elbow dislocations need physical therapy early in the healing process to prevent loss of extension, and these patients can usually return to play in 1 to 3 months depending upon stability and ROM.
Distal Humeral Fractures
These fractures include supracondylar, transcondylar, intercondylar, T-condylar and medial/lateral condylar fractures.
Supracondylar fractures of the distal humerus commonly occur between 5 and 10 years of age, and they usually occur from a severe fall on an outstretched hand (see Figure 26.10). If displaced, supracondylar fractures need to be treated operatively, whereas nondisplaced fractures can be treated with a long-arm cast for 3 to 4 weeks (90 degrees
flexion, neutral forearm rotation). If callous formation is confirmed at that time immobilization can be discontinued and active ROM exercises can be initiated. Supracondylar fractures in adults are best managed by an orthopedic surgeon unless nondisplaced or minimally displaced without neurovascular compromise. Nondisplaced fractures are placed in a long arm posterior splint at 90 degrees flexion with frequent re-examinations for neurovascular status in the early stages. At 2 weeks, gentle ROM exercises can begin, but splinting should continue for a total of 6 weeks, or until callus formation occurs. More vigorous rehabilitation can then be started to regain ROM and is usually best with the assistance of a physical therapist (6,7,8).
flexion, neutral forearm rotation). If callous formation is confirmed at that time immobilization can be discontinued and active ROM exercises can be initiated. Supracondylar fractures in adults are best managed by an orthopedic surgeon unless nondisplaced or minimally displaced without neurovascular compromise. Nondisplaced fractures are placed in a long arm posterior splint at 90 degrees flexion with frequent re-examinations for neurovascular status in the early stages. At 2 weeks, gentle ROM exercises can begin, but splinting should continue for a total of 6 weeks, or until callus formation occurs. More vigorous rehabilitation can then be started to regain ROM and is usually best with the assistance of a physical therapist (6,7,8).
 Figure 26.10 Supracondylar fracture. Note that the anterior humeral line does not cross the midportion of the capitellum, signifying supracondylar pathology (fracture). |
Fracture of the lateral condyle is the second most common pediatric elbow fracture and may also be caused by falling on an outstretched hand. These fractures are intra-articular, and open reduction is essential to avoid nonunion and malunion in displaced fractures. If nondisplaced, these fractures are initially placed in a posterior long arm splint, and if they remain nondisplaced over the first 10 to 14 days a long arm cast can be applied for 3 to 4 weeks, or until radiographic evidence of healing is seen. These fractures are also best managed by orthopedic surgeons due to the incidence of nonunion and growth arrest, which can cause cubitus varus or valgus deformity. Lateral condyle fractures in adults should also be evaluated by a surgeon (6,8,12).