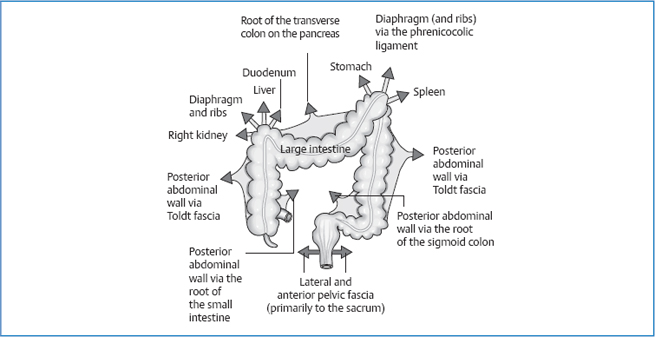
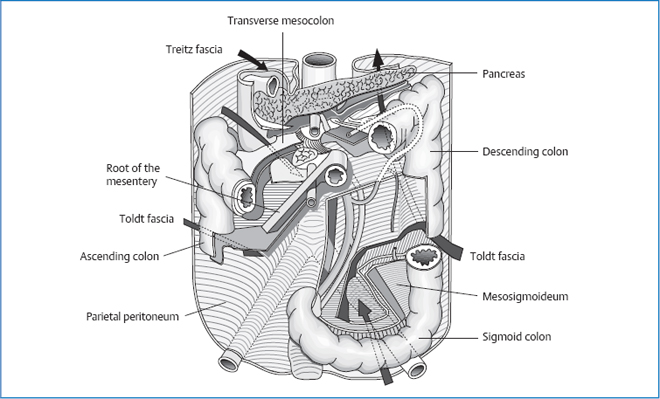
13 The Colon Length: approximately 1.5 m Diameter: Significant angles: Special characteristics: Fig. 13.1 Location of the colon. Retroperitoneal. Extraperitoneal. Phrenicocolic ligament. Toldt fascia. Sigmoid mesocolon. Portal vein. Fig. 13.2 Attachments of the colon, schematic. Fig. 13.3 Mesenteric attachments of the colon. Sacral parasympathetic innervation from S2 to S4 via: Maximal time: 5–7a.m. Minimal time: 5–7p.m. For basic information, see page 34. The greatest movement takes place in the flexures and in the transverse colon. The diaphragm is the propelling force for the movement of the colic flexures: in the frontal plane, the diaphragmatic movement is greater on the side than in the center—the flexures move inferiorly and medially (approximately 3 cm in normal inhalations, up to 10cm in maximum inhalation). In the sagittal plane, the flexures move anteroinferiorly. The transverse colon also moves inferiorly in the frontal plane, whereby the following applies: the fuller it is, the higher it lies. Each part of the colon completes a transversal motion on its parietal attachment (Toldt fascia, mesocolon). This results in a mediolateral or superoinferior (for the transverse colon) concave distortion in the frontal plane. In the same way, a rotation takes place around the longitudinal axis of the colon. In the colon, water and electrolytes are extracted from the chyme; the stool becomes thickened. In addition, the feces can be stored in the sigmoid and rectum for several days.
Anatomy
General Facts
 ascending colon 7–8cm
ascending colon 7–8cm
 transverse colon 5 cm
transverse colon 5 cm
 descending colon 3–5cm
descending colon 3–5cm
 sigmoid colon 3–5cm
sigmoid colon 3–5cm
 hepatic flexure (right colic flexure)
hepatic flexure (right colic flexure)
 splenic flexure (left colic flexure)
splenic flexure (left colic flexure)
 ileocecal valve
ileocecal valve
 sigmoid angle
sigmoid angle
 no villi and mucous membrane folds, only crypts
no villi and mucous membrane folds, only crypts
 semilunar folds (contracted ring muscles, not constant)
semilunar folds (contracted ring muscles, not constant)
 haustra (noncontracted sections of the intestine)
haustra (noncontracted sections of the intestine)
 taeniae coli (strong bands of longitudinal muscle, run together into a continuous muscle layer at the appendix and sigmoid)
taeniae coli (strong bands of longitudinal muscle, run together into a continuous muscle layer at the appendix and sigmoid)
 epiploic appendices (small pouches of serosa filled with fat)
epiploic appendices (small pouches of serosa filled with fat)
Location
Cecum
 intraperitoneal
intraperitoneal
 Runs diagonally in a caudal–medial–anterior direction and ends at the right iliac fossa.
Runs diagonally in a caudal–medial–anterior direction and ends at the right iliac fossa.
 approximately 7 cm long
approximately 7 cm long
 The ileocecal valve is found on the left side (superior and slightly posterior).
The ileocecal valve is found on the left side (superior and slightly posterior).
Vermiform Appendix
 5–10cm long
5–10cm long
 variability in diverse locations
variability in diverse locations
 projection onto the wall of the torso: approximately 2 cm superior to McBurney point
projection onto the wall of the torso: approximately 2 cm superior to McBurney point
Ascending Colon
 retroperitoneal
retroperitoneal
 pathway: on the right side in the lateral region superiorly and slightly posteriorly
pathway: on the right side in the lateral region superiorly and slightly posteriorly
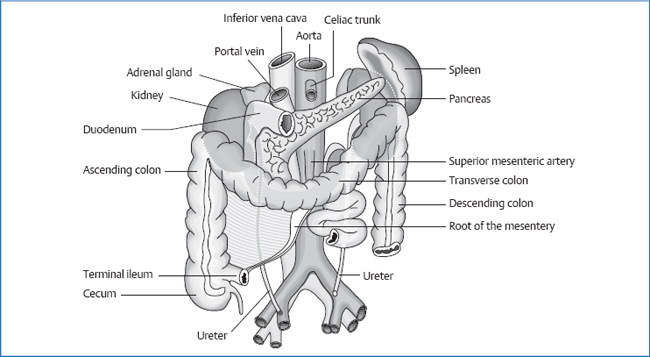
Right Colic Flexure
 angle of 70–80°
angle of 70–80°
 oriented sagittally with the opening in an anterior-caudal-medial direction
oriented sagittally with the opening in an anterior-caudal-medial direction
 projection onto the wall of the torso: rib 10 anterior to the right
projection onto the wall of the torso: rib 10 anterior to the right
Transverse Colon
 intraperitoneal
intraperitoneal
 The left end lies higher than the right end.
The left end lies higher than the right end.
 Has a concave shape posteriorly.
Has a concave shape posteriorly.
 Location is variable. We usually find it between two horizontal lines—one going through the ninth costal cartilage and the other through the navel—but it also extends to the lesser pelvis.
Location is variable. We usually find it between two horizontal lines—one going through the ninth costal cartilage and the other through the navel—but it also extends to the lesser pelvis.
Left Colic Flexure
 greater mobility than the right flexure
greater mobility than the right flexure
 angle of 50°
angle of 50°
 frontosagittal orientation with the opening in an anteromedial direction
frontosagittal orientation with the opening in an anteromedial direction
 projection: eighth rib anterior to the left
projection: eighth rib anterior to the left
Descending Colon
 retroperitoneal
retroperitoneal
 lies further posteriorly than the ascending colon in the lateral area on the left
lies further posteriorly than the ascending colon in the lateral area on the left
Sigmoid Colon
 intraperitoneal
intraperitoneal
 Runs from the posterosuperior part of the iliac fossa along the outer edge of the left psoas, crosses it 3–4 cm in front of the inguinal ligament, enters the lesser pelvis, and ends at the height of S3 in the rectum.
Runs from the posterosuperior part of the iliac fossa along the outer edge of the left psoas, crosses it 3–4 cm in front of the inguinal ligament, enters the lesser pelvis, and ends at the height of S3 in the rectum.
 Middle section can have a diameter of 15 cm.
Middle section can have a diameter of 15 cm.
 Pelvic section of the sigmoid can be displaced upward by a full bladder, the rectum, its own state of fullness, or the uterus.
Pelvic section of the sigmoid can be displaced upward by a full bladder, the rectum, its own state of fullness, or the uterus.
Proximal Rectum
Distal Rectum
Topograhic Relationships
Cecum
 abdominal wall
abdominal wall
 posterior peritoneum
posterior peritoneum
 iliac fascia
iliac fascia
 iliacus
iliacus
 envelope of the external iliac artery and vein
envelope of the external iliac artery and vein
 inguinal ligament
inguinal ligament
 psoas major
psoas major
 lateral cutaneous nerve of the thigh
lateral cutaneous nerve of the thigh
 femoral nerve
femoral nerve
 genitofemoral nerve
genitofemoral nerve
 small intestinal loops
small intestinal loops
Vermiform Appendix
 right ovary
right ovary
 possible contact with the bladder, rectum, and uterus
possible contact with the bladder, rectum, and uterus
Ascending Colon
 iliac fossa
iliac fossa
 covered by peritoneum
covered by peritoneum
 right kidney
right kidney
 Toldt fascia
Toldt fascia
 subcostal nerve
subcostal nerve
 iliohypogastric nerve
iliohypogastric nerve
 ilioinguinal nerve
ilioinguinal nerve
 aponeurosis of quadratus lumborum, kidney fascia, iliac fascia
aponeurosis of quadratus lumborum, kidney fascia, iliac fascia
 lateral and anterior abdominal wall
lateral and anterior abdominal wall
 diaphragm
diaphragm
 small intestinal loops
small intestinal loops
 duodenum (descending part)
duodenum (descending part)
 liver
liver
 rib 11
rib 11
Right Colic Flexure
 liver
liver
 duodenum (descending part)
duodenum (descending part)
 diaphragm
diaphragm
 right kidney
right kidney
 phrenicocolic ligament on the right
phrenicocolic ligament on the right
Transverse Colon
 liver
liver
 gallbladder
gallbladder
 abdominal wall indirectly via the greater omentum
abdominal wall indirectly via the greater omentum
 greater curvature of the stomach
greater curvature of the stomach
Transverse Mesocolon
 pancreas
pancreas
 duodenum
duodenum
 jejunum
jejunum
 left kidney
left kidney
 spleen
spleen
Left Colic Flexure
 greater curvature of the stomach
greater curvature of the stomach
 spleen
spleen
 phrenicocolic ligament on the left
phrenicocolic ligament on the left
 diaphragm
diaphragm
 lateral abdominal wall
lateral abdominal wall
 rib 8/9
rib 8/9
Descending Colon
 covered by peritoneum
covered by peritoneum
 left kidney
left kidney
 small intestinal loops
small intestinal loops
 Toldt fascia
Toldt fascia
 posterior abdominal wall
posterior abdominal wall
 subcostal nerve
subcostal nerve
 iliohypogastric nerve
iliohypogastric nerve
 ilioinguinal nerve
ilioinguinal nerve
 rib 10/11
rib 10/11
Sigmoid Colon
 iliac fascia
iliac fascia
 Toldt fascia
Toldt fascia
 iliacus
iliacus
 small intestinal loops
small intestinal loops
 lateral cutaneous nerve of the thigh
lateral cutaneous nerve of the thigh
 rectum
rectum
 uterus
uterus
 left ovary and fallopian tube
left ovary and fallopian tube
Sigmoid Mesocolon
 left ureter
left ureter
 testicular/ovarian vessels on the left
testicular/ovarian vessels on the left
 external iliac vein
external iliac vein
Attachments/Suspensions
 turgor
turgor
 organ pressure
organ pressure
Cecum
 posterior peritoneum (superior part)
posterior peritoneum (superior part)
 mesentery (inferior part)
mesentery (inferior part)
Ascending Colon
 peritoneum
peritoneum
 Toldt fascia
Toldt fascia
Right Colic Flexure
 peritoneum
peritoneum
 phrenicocolic ligament
phrenicocolic ligament
 hepatocolic ligament (from the liver via the flexure to the right kidney)
hepatocolic ligament (from the liver via the flexure to the right kidney)
 cystoduodenal ligament (extension of the hepatoduodenal ligament)
cystoduodenal ligament (extension of the hepatoduodenal ligament)
Transverse Colon
 transverse mesocolon
transverse mesocolon
 greater omentum (ends at the phrenicocolic ligaments)
greater omentum (ends at the phrenicocolic ligaments)
 gastrocolic ligament (part of the greater omentum): as a result of this ligament, the right part of the transverse colon has greater mobility
gastrocolic ligament (part of the greater omentum): as a result of this ligament, the right part of the transverse colon has greater mobility
Left Colic Flexure
Descending Colon
Sigmoid Colon
Circulation
Arterial
 superior mesenteric artery
superior mesenteric artery
 inferior mesenteric artery
inferior mesenteric artery
Venous
Lymph Drainage
 superior mesenteric lymph nodes
superior mesenteric lymph nodes
 celiac lymph nodes
celiac lymph nodes
 lumbar lymph nodes
lumbar lymph nodes
 inferior mesenteric lymph nodes
inferior mesenteric lymph nodes
 left lumbar lymphatic trunk
left lumbar lymphatic trunk
Innervation
 sympathetic nervous system from T10 to L2 via the greater and lesser splanchnic nerves
sympathetic nervous system from T10 to L2 via the greater and lesser splanchnic nerves
 T10–T11 via the superior mesenteric ganglion
T10–T11 via the superior mesenteric ganglion
 T12–L2 via the inferior mesenteric ganglion
T12–L2 via the inferior mesenteric ganglion
 parasympathetic nervous system
parasympathetic nervous system
 vagus nerve (ends at the superior mesenteric ganglion)
vagus nerve (ends at the superior mesenteric ganglion)
 pelvic splanchnic nerves-inferior hypogastric plexushypogastric nerves
pelvic splanchnic nerves-inferior hypogastric plexushypogastric nerves
 superior hypogastric plexus-inferior mesenteric plexus
superior hypogastric plexus-inferior mesenteric plexus
Organ Clock
Organ-Tooth Interrelationship
Movement Physiology according to Barral
Mobility
Motility
Physiology
Pathologies
Symptoms that Require Medical Clarification
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




