Chapter 4 The Cervicobrachial Region
Affections of the brachial plexus are usually the result of either compression or injury. The resultant symptoms and signs are often confusing, but these disorders should always be considered in the differential diagnosis of neuropathies of the upper extremity.
Anatomy
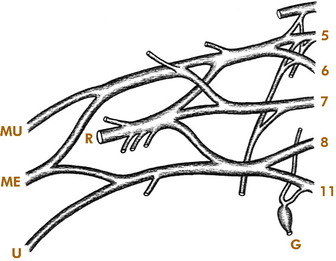
The brachial plexus is formed by the anterior rami of the last four cervical and first thoracic nerves (Fig. 4-1). In general, the upper portion of the plexus innervates the shoulder abductors, external rotators, and the elbow flexors. It also provides sensation to the shoulder and radial side of the arm. The lower portion of the plexus primarily innervates the forearm and hand muscles and provides sensation to the ulnar side of the arm, forearm, and hand. The first thoracic ramus also communicates with the first thoracic ganglion, through which sympathetic fibers are carried to the face from the spinal cord. Thus, involvement of the lower portion of the plexus by disease or injury may produce Horner’s syndrome (ptosis, miosis, enophthalmos, and anhidrosis).
The plexus passes distally between the middle and anterior scalene muscles, which attach to the first rib (Fig. 4-2). Beneath the clavicle, it is joined by the subclavian artery. The subclavian vein passes anterior to the scalenus anticus muscle. Artery, vein, and plexus then enter the axilla beneath the pectoralis minor muscle, with the lower trunk of the plexus (C8, T1) lying on the first rib.
Thoracic Outlet Syndromes
CERVICAL RIB SYNDROME
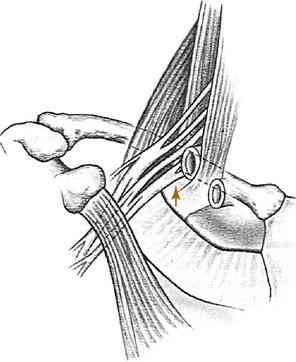
The cervical rib usually arises from the seventh cervical vertebra and is the most common cause of neurovascular compression at the base of the neck (Fig. 4-3). The condition may be bilateral. The rib or its fibrous extension narrows the interval between the anterior and middle scalene muscles and produces a higher barrier over which the neurovascular structures must arch on their way into the arm. In older patients or those with muscular weakness, the shoulder may also sag more than normal, which further increases the tension on the neurovascular structures. The compression may also be increased by carrying a heavy object.
In the absence of a cervical rib, compression can occur between the middle and anterior scalene muscles because of abnormal insertions or the presence of additional muscle slips in the interscalene interval (scalenus anticus syndrome).
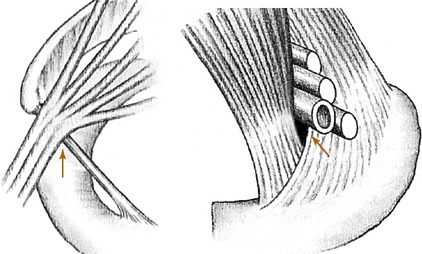
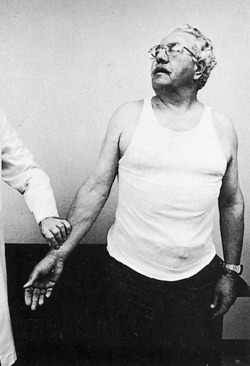
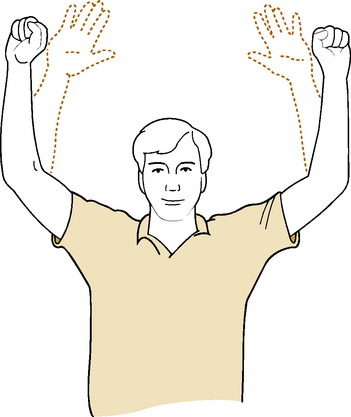
Provocative positioning tests are often described in the assessment of thoracic outlet syndromes. Adson’s test may be positive in cervical rib and scalenus anticus syndromes (Fig. 4-4). This test takes advantage of the fact that by tensing the scalene muscles the interval between them is decreased, and any existing compression of the subclavian artery is increased. The test is performed by having the patient breathe deeply, extend the neck, and turn the chin toward the affected side. When the test is positive, a decrease in the radial pulse is noted, and pain is reproduced. If the test is negative, it is repeated with the chin turned to the opposite side. Although a positive test result is suggestive of compression in the interscalene region, it is often positive in the normal population and is not necessarily diagnostic of cervical rib or scalenus anticus syndrome. Symptoms can also be reproduced occasionally by exercising the fingers with the arms elevated (Fig 4-5).
Roentgenographic examination may reveal an extra rib extending from the transverse process of the seventh cervical vertebra (Fig. 4-6). The rib may be fully developed or rudimentary, and it is often bilateral. Its presence does not necessarily imply that it is symptomatic, however, because cervical ribs are often present in asymptomatic individuals.