CHAPTER 6
Techniques and Scales for Measuring Spastic Paresis
Marjolaine Baude and Jean-Michel Gracies
This chapter focuses on technical, analytical measurement tools in patients with spastic paresis and their potential use in clinical trials. When considering the main factors of movement limitation in spastic paresis, one comes to recognize that: (a) most of the movement-limiting factors are antagonist resistances (soft tissue contracture, spastic dystonia, spastic cocontraction, spasticity) and that (b) at least three of the more important factors—paresis, spastic dystonia, spastic cocontraction—are not clinically measurable when taken individually (1–3).
DEFINITION OF SPASTICITY
In 1954, Tardieu proposed to define spasticity as an increase in stretch reflexes that could be characterized by the speed required to elicit the reflexes (4). Conceptually, this definition of spasticity was largely followed in the version proposed by Lance and colleagues in their 1979 consensus meeting, as a velocity-dependent increase in stretch reflexes (5). One error in that definition was that there has never been a demonstration that stretch reflex enhancement in spastic paresis is velocity dependent (6); on the contrary, the reflex enhancement seems conversely related to speed, as the enhancement compared to normal is in fact more prominent at slow stretch speed (7,8). On the other hand, the reflexes that are enhanced in spasticity are velocity dependent, both in healthy subjects (9) and in patients with spastic paresis (10–12). Therefore, a more correct definition of spasticity, as the characteristic phenomenon we may observe in all patients with spastic paresis, is an increase in the velocity-dependent stretch reflexes (2,3).
MEASURE OF SPASTICITY: THE ASHWORTH AND TARDIEU SCALES
After a first period in which he focused on measuring the speed required to elicit stretch reflexes, Tardieu later moved to a measurement of the angle of the muscle reaction to fast stretch (1). At the same time, Ashworth created an ordinal 5-point scale (Table 6.1), as a simple clinical tool to rate resistance to passive movement, that is, tone, and thus evaluate an “anti-spastic” drug in patients with multiple sclerosis (13). A couple of decades later, as botulinum toxin use became popular, the Ashworth Scale was gradually equated to a tool rating spasticity (instead of tone) and its use markedly increased (14).
The Ashworth Scale was later modified (Table 6.2) to a 6-point scale, with the aim of increasing the sensitivity of its grades at the lower end of the scale for those patients who demonstrate tone levels at that end (15).
However, there has since been considerable evidence that the amount of resistance to passive movement is not an exclusive measure of spasticity (16). In fact, when examining the scale carefully one can realize that only the grades 1 and 1+ correspond to true spasticity reactions, as they contain a “catch and release,” which is a key clinical characteristic of stretch reflexes. The problem lies in the higher grades 2, 3, and 4 that attempt to rate “spasticity” by an increasing resistance to passive movement, which could be a result of viscoelastic components, innadvertant voluntary contractions, dystonic activity, and so on. All the previous forms of resistances to passive movement will not lead to a sense of “catch-and-release” by the clinician. Therefore, it can be proposed that the Ashworth and Modified Ashworth Scales stop measuring spasticity, specifically from Grade 2 on. Unfortunately, most patients recruited in clinical studies are Grade 2 and above (17,18).
In addition, it is long known from torque–angle relationships that overall (passive and active) resistance to muscle stretch is exponentially related to the stretch itself (19). Unfortunately, the Ashworth and the Modified Ashworth Scales do not specify the part of the range of available movement over which resistance should be rated. This may lead to considerable interrater variations as some raters may assess a low grade because they assess resistance on the first part of the available range while others may decide on a high grade because of rating the resistance mostly over the end of the range (20). Finally, the Ashworth and the Modified Ashworth Scales do not specify the speed at which the muscle should be stretched, which, as seen earlier, may have remarkable impact on the active part of the resistance (10–12) (specifically the reflex active part).
TABLE 6.1
THE ASHWORTH SCALE | |
Grade | Description |
0 | No increase in tone |
1 | Slight increase in tone giving a catch when the limb is moved in flexion or extension |
2 | More marked increase in tone but limb easily flexed |
3 | Considerable increase in tone – passive movement is difficult |
4 | Limb rigid in flexion or extension |
Source: Adapted from Ref. (13). Ashworth B. Preliminary trial of carisoprodol in multiple sclerosis. Practitioner. 1964;192:540–542.
TABLE 6.2
THE MODIFIED ASHWORTH SCALE | |
Grade | Description |
0 | No increase in muscle tone |
1 | Slight increase in muscle tone, manifested by a catch and release or by minimal resistance at the end of the ROM when the affected part(s) is moved in flexion or in extension |
1+ | Slight increase in muscle tone, manifested by a catch, followed by minimal resistance throughout the reminder (less than half) of the ROM |
2 | More marked increase in muscle tone throughout most of the ROM, but affected part(s) easily moved |
3 | Considerable increase in muscle tone, passive movement is difficult |
4 | Affected part(s) rigid in flexion or extension |
ROM, range of motion.
Source: Adapted from Ref. (15). Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther. 1987;67(2):206–207.
Beyond reliability issues, a number of experimental works also shed doubt on the validity of the Ashworth Scale, as Ashworth ratings were found not to be comparable to laboratory measures of spasticity or clinical tendon taps in a number of paretic populations (21–23,48) (multiple sclerosis, spinal cord injury, stroke, etc.). Specifically, the Ashworth Scale grades the resistance to movement—spasticity included—but it appears unable to differentiate whether the cause of the abnormal resistance is neural or tissular (22–25) and in particular to distinguish spasticity from soft tissue retraction or spastic dystonia (14).
As Tardieu never translated his methods of clinical examination (1) into a scale, the scale today known as the Tardieu Scale was historically elaborated in the late 1990s, then named after Tardieu to pay tribute to his key idea of angular measurement, and finally published in 2000 (26,27). This development had followed Held and Pierrot-Deseilligny’s first attempts at standardizing Tardieu’s historical method of clinical examination into a complex scale that was deriving 12 numbers per muscle (28) (an early scale that became temporarily known as the Held scale). The Tardieu Scale reliability was first demonstrated in children with infant paresis (29,30) and then in adults with spastic paresis as far as the determination of angles (not the spasticity grade) was concerned (31). The scale entails two clinical maneuvers, consisting both in measuring an angle from zero being the position of minimal stretch of the tested muscle group (as opposed to the standard anatomical zero of the joint; see Figure 6.1).
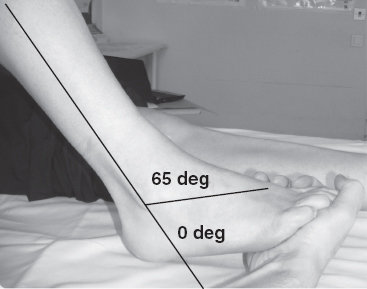
FIGURE 6.1 Measurement of XV1 and XV3 (Tardieu Scale) of the soleus muscle.
The first maneuver aims to assess passive soft tissue extensibility. The test is thus only completed after ensuring that the patient optimally rests the tested muscles immediately prior to the test (26,27). One visually (without goniometer) measures the functional muscle length (or maximal passive range of motion) for each tested muscle group. This is done by exerting the slowest and strongest possible stretch on the muscle group and associated soft tissue (fascia, tendons, ligaments, capsules, skin, nerves, and vessels) to move the limb segment as far as possible without causing pain or jeopardizing soft tissue integrity. The rationale behind using extreme slowness is to minimize recruitment of stretch reflex afferents, which might create a spastic reaction that would impact on the measured amplitude (10–12). The rationale behind using strong stretching force (maximal force for the examiner, compatible with preserving soft tissue integrity) is to optimally overcome the spastic dystonia present in the assessed muscle group, such that this type of overactivity is minimally involved in explaining the angle of arrest (19). The measured angle has been termed XV1 (V1, slowest velocity) (26,27,29). In effect, XV1 (which we like to call functional muscle length) represents the amplitude that active movement against the tested antagonist should reach in theory, if the disorder were limited to muscle tissue and not to neural command. Obviously, various nonmuscular underlying joint alterations may impact on XV1, such as arthritis, capsulitis, or immobilization-induced joint retractions (32). However, pure joint limitations should not in general be responsible for the major part of XV1 reductions (32). In addition, XV1 may not represent pure muscle or joint contractures as it might also reflect extensibility losses in fascia, aponeuroses, skin, vessels, and so on (33,34). The proposed term functional
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree






