Fig. 9.1
Show the MRI appearance of a mediopatellar synovial plica
Ultrasonography is another well-accepted investigation method of the knee. It has several advantages over MRI, such as cost, reproducibility and investigation time. Dynamic sonography allows for the examination of the internal structures of the knee in movement relying not only on different tissue echogenicity but also on tissue adhesion in the dynamic state. Coupled with sonopalpation (tissue recognition under transducer pressure and pain perception when passing a transducer over the affected part), allows more accurate diagnosis. The main disadvantage of this technique consists in the need of specially trained personnel in performing and interpreting musculo-skeletal ultrasonography [11].
Arthroscopy still remains the most accurate mean of identifying synovial plicas of the knee [12], but there is no definitive indication to perform a diagnostic arthroscopy in order to confirm the presence of a synovial plica [13].
There is a syndrome that is caused by the irritation and resultant inflammatory reaction of the relic of the synovial plica of the knee that is known as “pathological synovial plica syndrome” (PSPS). It is characterized by supra- and mid-patellar pain with knee extension as well as the presence of audible cracking noises with knee flexion and extension. Contraction of the quadriceps associated with compression of the supra-patellar pouch also causes pain. In addition, patients often experience a sensation of instability when they are walking up or down stairs or slopes. These symptoms have been correlated with recent changes in the intensity or quality of patients’ athletic activities. It appears especially in individuals who practice sports infrequently and subject higher stresses on untrained, unfit joints. Clinically a young active patient will present with dull, aching pain usually situated in the proximal medial aspect of the knee or in the infrapatellar aspect [13, 14].
The diagnosis of PSPS is mainly a clinical one, and in most patients conservative treatment will yield very good results. The classical clinical test used for the detection of a symptomatic medial plica is the Hughson plica test To perform this test the patient has to be lying in dorsal decubitus with the affected knee flexed at 90° while the examiner is internally rotating the tibia while passively moving the patella from lateral to medial all the while they are extending the affected leg to a straight position and then flexing it back to 90°. A positive Hughson test produces a sharp pain as the inflamed plica is caught between the articulate surfaces of the femur and the patella during knee flexion and/or a palpable clicking. A symptomatic plica will usually have a combination of these signs, as the clicking sensation caused by the interaction between the plica and the articular surfaces will usually produce pain or at least a sensation of local discomfort.
Plica pain is usually exacerbated by active quadriceps contraction. Other symptoms such as acute lateral pain or a giving away sensation can also be present at physical examination. MRI’s are routinely performed in patients complaining of knee pain or instability, but they don’t always show a clear image of synovial plicae, presumably because its static nature. The synovial plica syndrome is thus, despite advances in MRI imaging technique and advanced image interpretation, mostly an intraoperative diagnosis as it takes into account the clinically painful knee and the lack of other intraarticular pathology.
If diagnosed preoperatively, unassociated with other lesions, the routine treatment is conservative. Nonsurgical therapeutic modalities include rest from strenuous activities (such as prolonged running, sports, squatting), NSAID’s. Anti-inflammatory medication can be administered orally, with limited efficacy, locally via topical applications or a local subsynovial, extraarticular, corticosteroid infiltration in the mediopatellar region [4] that can be guided ultrasonographically as well and intraarticular corticosteroid infiltration [6]. A physical rehabilitation program should be prescribed and it should include closed chain kinetic quadriceps exercises and hamstring stretching. Improved outcomes are obtained if the hamstring-stretching program is performed several times a day [15].
Open chain kinetic exercises such as knee extensions especially those that are done under added weights add stress to an already painful plica, can often cause a further increase in the symptoms. The duration of the rehabilitation program should vary depending on patient specific response. About half of the patients have a positive response to 6 weeks of physical therapy noticing the resolution of or a significant improvement in their symptoms. A further 6 weeks of physical therapy provide relief of symptoms in the majority of the patients [16].
If the conservative treatment fails or a medial synovial plica is detected during knee arthroscopy that is performed for an unrelated pathology (such as a suspected meniscal tear), if the pathology that was suspected based on the clinical examination and preoperative imaging investigations is confirmed by arthroscopic visualization, it is recommended that it should be left in place by most authors. This treatment indication of plicae surgery is still controversial and some authors still advocate the resection of an asymptomatic medial plica even in conjunction with other associated intraarticular pathology in order to prevent the development of a subsequent plica syndrome [17]. But if after thorough examination of the knee no pathology is found and the presence of a synovial plica is detected we have found that the arthroscopic resection of the plica provides full relief of the symptoms in most cases [2].
There is a discussion in literature regarding the best way to treat a PSPS, either by totally resecting the involved mediopatellar plica to the capsular junction, a partial resection of the plica or just a incision, detensioning the synovial fold and allowing it to slide over the medial condyle into the recess during knee flexion. While some immediate relief of the painful symptoms may exist, just by arthroscopic incision and detensioning of the synovial plica there are no studies to demonstrate a long-term benefit and therefore this procedure is not considered to be advisable in treating a pathological mediopatellar synovial plica in the authors opinion, the risk of recurrence being significant. As the main complication of surgical treatment of a synovial plica is the persistence of symptoms we can conclude by saying that a complete arthroscopic resection of the plica should be performed if the decision to address the plica is made, either pre- or intraoperative. The resection should be extensive, up to the junction with the synovial membrane but care must be taken to avoid over resecting the plica because that could lead to iatrogenic injury to the capsular structures, rendering the medial retinaculum insufficient with subsequent patellar instability or it could cause iatrogenic vascular injury to the medial geniculate artery with subsequent hemarthrosis. Plica resection should therefore be performed with the arthroscope looking from the anterolateral portal and the working tool (this must include a shaver and preferably a radiofrequency probe apart from the regular arthroscopic punch) in the anteromedial portal. More so, as this is a technically difficult procedure because of the position of the plica and the viewing angles that are involved a medial suprapatellar portal can be used to facilitate access in the mediopatellar region of the joint [4, 18].
Postoperative management should begin with a period of relative rest. No knee immobilization is necessary in our experience and full weightbearing can be resumed as tolerated. However there should be a delay in initiating postoperative rehabilitation of around 2 weeks to minimize the risk of symptom recurrence due to the scarring of the synovial membrane in the area of the resected plica and to prevent secondary synovitis.
Arthroscopic resection proves a successful therapeutic tool for symptomatic synovial plicae in cases where conservative treatment has failed. Recurrence of symptoms is usually associated with residual intraarticular pathology that was left untreated during surgery [6, 13, 15, 19] (Fig. 9.2).
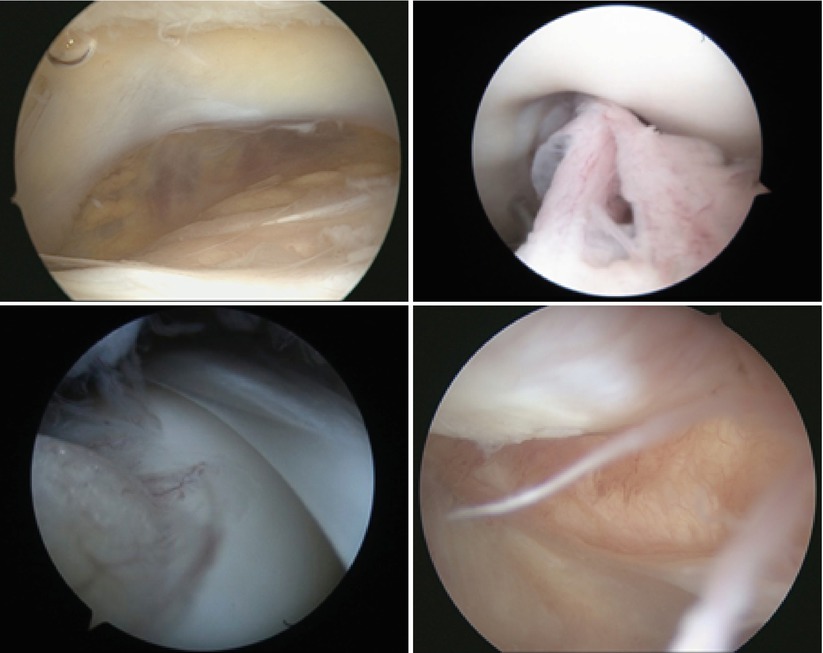
Fig. 9.2
Examples of supra, infra and mediopatellar plicae
9.2 Synovitis
The term “synovitis” depicts the inflammation of the synovial membrane that either acute or chronic. This can be caused by different underlying pathology such as rheumatoid arthritis (RA) or spondylarthropathy, lupus, gout or osteoarthritis being the most common causes of chronic synovitis, while acute synovitis follows a knee trauma or it can occur after a neglected meniscal injury. Pigmented villonodular synovitis (PVNS) of the knee is a proliferative disorder of the synovial membrane. It forms benign villi and nodules with large amounts of intracellular haemosiderin. The highest prevalence is in young adults between their twenties and their forties and although it affects other joints, the knee is the most frequently involved [20]. Two forms exist, localized PVNS and diffuse PVNS. Diagnosing PVNS is initially done with articular aspiration and confirmed with the help of MRI studies [20, 21], arthroscopic views confirm the disease but the positive diagnosis is made by histological exploration that makes the differential diagnosis with other synovial disorders such as chronic synovitis or RA. Increasing evidence supports the role of chronic synovial inflammation in the pathogenesis and structural progression of osteoarthritis (OA) a reciprocity has been created between the severity of synovial inflammation and the chondral joint degeneration and the number and size of osteophytes [1–3]. The hemophiliacs represent another group of patients prone to synovial inflammation and recurrent spontaneous hemarthrosis even during gentle manouvers. Arthroscopic synovectomy can be performed if the conservative treatment fails. It is usually performed as a two portal technique [22, 23] (Fig. 9.3).


Fig. 9.3




Open synovectomy and the removed synovial membrane
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








