Synovectomy for Pigmented Villonodular Synovitis
Edward Y. Cheng
Vineet Sharma
Pigmented villonodular synovitis (PVNS) is a unique condition affecting synovial tissues in joints, tendon sheaths, and bursa. The disease is classified into three categories: (a) extra-articular PVNS (also known as giant cell tumor of the tendon sheath), (b) localized intra-articular PVNS, and (c) diffuse intra-articular PVNS. It is unknown whether or not this disease is a true neoplasm or reactive in origin (24), but recent evidence of monoclonality suggests a neoplastic etiology (3,18). The disease may occur in either young adults or the elderly and commonly presents with symptoms related to the intra-articular nature of the mass. The knee is the most common joint involved but any synovial joint including the hip (Fig. 35-1) (33), ankle (Fig. 35-2) (13), shoulder (Fig. 35-3) (22), or elbow (30) may be affected. Polyarticular disease in children has also been reported (12,34). Pain and intermittent effusions, either traumatic or nontraumatic in origin, are caused by the inflammatory synovitis and recurrent hemarthroses that are typical. In the knee, locking may occur or the disease may be misdiagnosed as a popliteal cyst.
INDICATIONS/CONTRAINDICATIONS
The mainstay of treatment of PVNS is surgical excision by either open or arthroscopic means. No medical therapy is known to be effective at eradicating the disease. Untreated, some patients may develop stable disease but most patients will require treatment for symptomatic reasons or to prevent the eventual progression to periarticular erosive cyst formation and subsequent destruction of the cartilaginous joint surface. In about one third of cases, an aggressive course may ensue with multiple recurrences despite surgical resection (9). In these cases, radiation may be considered, administered by either external beam (26) or via intra-articular radiation synovectomy (11,16). Once joint destruction has occurred, total knee arthroplasty is the only means of addressing the disabling symptoms; however, a synovectomy must still be performed as recurrences after knee arthroplasty have been documented (1,14).
Indications
Symptomatic PVNS
Asymptomatic PVNS
Locally recurrent PVNS
PREOPERATIVE PLANNING
Examination and Evaluation
Patients with PVNS demonstrate evidence of an effusion or a hemarthrosis when minor trauma results in a hemorrhage. In the localized type, locking due to the presence of an intra-articular mass is common, and in both the diffuse and localized from, there may be limited joint arc of motion. A palpable mass is not usually appreciated unless there are extra-articular disease manifestations. Most commonly, the extra-articular disease occurs in the popliteal fossa or intercondylar notch (Fig. 35-4). In advanced cases, findings consistent with degenerative arthrosis are evident.
Imaging Studies
Plain radiographic findings in the early stage of disease are either normal or may show a displaced suprapatellar fat plane due to presence of an effusion. A capsular-based noncalcified soft tissue mass may be present (7). In later stages, periarticular cysts are present and cartilage thinning is seen (4). The findings on magnetic resonance imaging (MRI) are more dramatic and in many cases diagnostic. A soft tissue mass with alternating areas of bright signal and dark signal void on both T1 and T2 sequence represents the fluid (bright on T2) and fat (bright on T1) accumulation as well as hemosiderin deposits within the soft tissue (dark on both T1 and T2), respectively (Fig. 35-5). In the appropriate clinical setting, these findings are nearly diagnostic of PVNS, although rheumatoid arthritis may have a similar appearance (23,31). The nodular form may not always be localized to one location and instead may occur in multiple compartments within the joint. It is essential to precisely
determine the extent of the disease on MRI as this will directly affect the surgical approach to the disease. In doubtful cases, the diagnosis can be established with a biopsy.
determine the extent of the disease on MRI as this will directly affect the surgical approach to the disease. In doubtful cases, the diagnosis can be established with a biopsy.
 FIGURE 35-2 A: Sagittal T2 MRI image of PVNS of the tibio talar and subtalar joint. B: Sagittal T1 MRI image of PVNS of the tibio talar and subtalar joint. |
 FIGURE 35-4 Sagittal T2 MRI image of PVNS in an extra-articular location extruding outward from the intercondylar notch. |
Gross and Histologic Appearance
The intraoperative gross appearance of disease is characteristic. In the diffuse form, multiple fronds of reddish-brown pigment-stained synovial tissue represent villous projections floating in synovial fluid. In the nodular form, a thickened reddish-brown and yellow stained xanthomatous soft tissue mass with cavitary areas of fluid accumulation is seen and the mass may spread dramatically in the suprapatellar pouch (Fig. 35-6) or intercondylar notch.
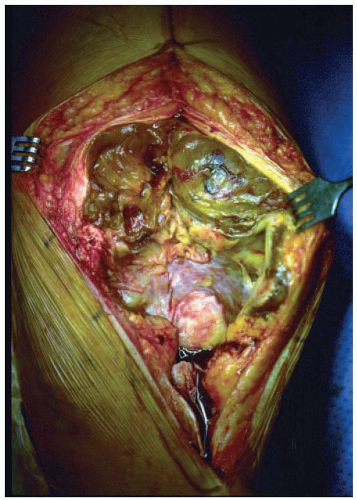 FIGURE 35-6 Clinical intraoperative photo of markedly thickened PVNS with reddish-brown pigmentation and xanthomatous appearance in the suprapatellar pouch. |
Histologically, PVNS is indistinguishable from a giant cell tumor of tendon sheath (nodular tenosynovitis). A proliferation of round synovial-like cells is present with occasional multinucleated osteoclast-type giant cells, xanthomatous cells, and inflammatory cells interspersed throughout the lesion (Fig. 35-7) (5,15).
Specific Approaches
The controversy regarding open versus arthroscopic synovectomy is difficult to resolve. With either technique, in the diffuse form, the recurrence rate ranges from 8% to 50% (10,25,32). The only factor which is conclusively known to prevent local recurrence is complete and aggressive resection of the affected tissues. The benefits of arthroscopic synovectomy are a quicker rehabilitation and avoidance of arthrotomy and postoperative knee stiffness. The disadvantages are related to performing an intralesional excision or debridement, potential for intra-articular spread of disease converting a localized form to diffuse disease, seeding of portal sites (Fig. 35-8), difficulty accessing posterior and extra-articular locations of disease, and difficulty in removal of markedly thickened
synovial tissue. Advantages of an open synovectomy over the arthroscopic technique are the ability to do a marginal or en bloc excision of the mass, complete a total synovectomy as opposed to a only a debridement, and the expeditious nature of an arthrotomy. Excellent results using cryosurgery in addition to open synovectomy have been reported (20). However, the open procedure can be technically challenging to perform adequately through a popliteal exposure and may result in postoperative adhesions if a normal arc of knee motion is not regained promptly after surgery. No prospective trials directly comparing these techniques have been performed, and they would be considerably difficult to power adequately due to the rarity of the disease.
synovial tissue. Advantages of an open synovectomy over the arthroscopic technique are the ability to do a marginal or en bloc excision of the mass, complete a total synovectomy as opposed to a only a debridement, and the expeditious nature of an arthrotomy. Excellent results using cryosurgery in addition to open synovectomy have been reported (20). However, the open procedure can be technically challenging to perform adequately through a popliteal exposure and may result in postoperative adhesions if a normal arc of knee motion is not regained promptly after surgery. No prospective trials directly comparing these techniques have been performed, and they would be considerably difficult to power adequately due to the rarity of the disease.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree













