Surgical Treatment of Traumatic Quadriceps and Patellar Tendon Injuries of the Knee
Introduction
Background
Ruptures of the extensor mechanism are debilitating injuries that typically require surgery and prolonged physical therapy
Knee extension plays a central role in activities of daily living
Epidemiology
Quad tendon ruptures typically occur in patients older than 40 years; patella tendon ruptures typically occur in patients younger than 40 years
Patella fractures are the most common cause of extensor mechanism failure
Indirect injury accounts for twice as many quad tendon injuries and three times as many patella tendon injuries as direct injury
Males are more likely to have quad or patella tendon rupture
Biomechanics and Pathology
The relatively low frequency of tendinous rupture is partly due to the relative strength of tendons
Biomechanical studies have shown that a force 17.5 times body weight is required for rupture of extensor mechanism
Nondirect traumatic tendinous rupture is likely to occur through a region of pathologic change
End-stage renal disease, diabetes mellitus, rheumatoid arthritis, gout, obesity, hyperparathyroidism, systemic lupus erythematosus, systemic steroid use, infection, and repetitive microtrauma predispose to rupture
Incidence of systemic conditions is 70% in bilateral quadriceps ruptures and 20% in unilateral ruptures
One study showed poor blood supply in the quadriceps tendon in a zone 1 to 2 cm from insertion site of the quadriceps tendon into the patella; this finding coincides with the observation that most tears occur within 2 cm of the superior pole of the patella
Patient Selection
Symptoms—Pain, inability to perform a straight-leg raise due to lack of active knee extension, a palpable suprapatellar or infrapatellar tendinous defect, large knee effusion, ecchymosis
Timing—Surgical repair done more than 2 weeks post injury is associated with increased surgical complexity and more unsatisfactory results
Chronic tears are more likely to need graft augmentation
Relative contraindications
Nonambulatory patients
Significant medical comorbidities
Compromised soft tissues around the knee from infection, trauma, radiation
Known noncompliance with rehabilitation
Chronic irreparable tears
Incomplete tear of the extensor mechanism can be treated nonsurgically
Incomplete tears—Evident when patients retain active knee extension against gravity while supine but have compromised extension against resistance while seated
Such patients lack a large palpable tendinous defect and radiographic findings of patella baja or alta
Preoperative Imaging
Radiography
AP and lateral views
Quadriceps tendon tear—Characteristic findings are patella baja, interruption of quadriceps tendon soft-tissue shadow, and suprapatellar soft-tissue mass
Patellar tendon tear—Characteristic finding is patella alta
Ultrasonography
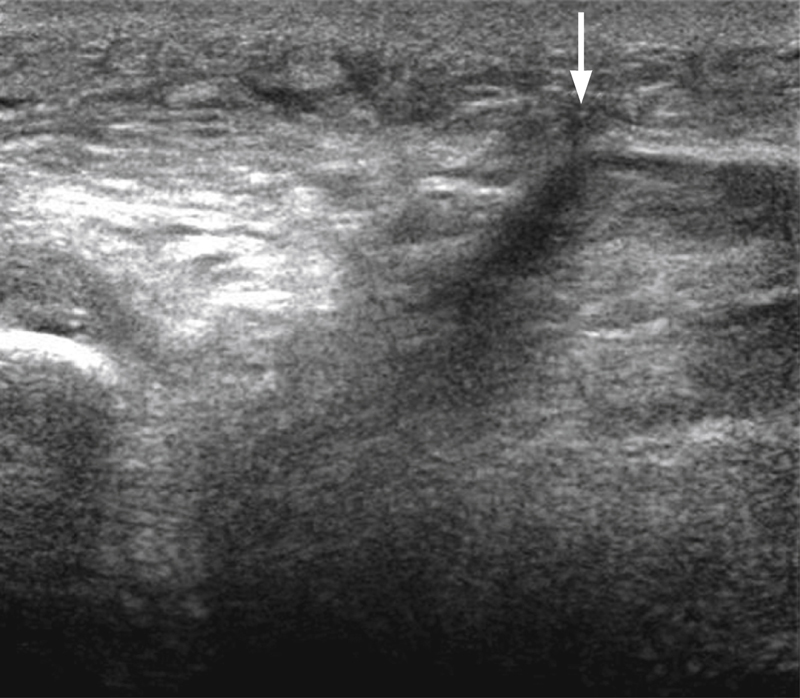
Figure 1Sagittal ultrasonographic image shows a ruptured quadriceps tendon. The anechoic shadow within the substance of the tendon (arrow) represents the rupture.
Operator dependent
Expeditious and inexpensive way to determine location and completeness of the tear (Figure 1)
Magnetic Resonance Imaging
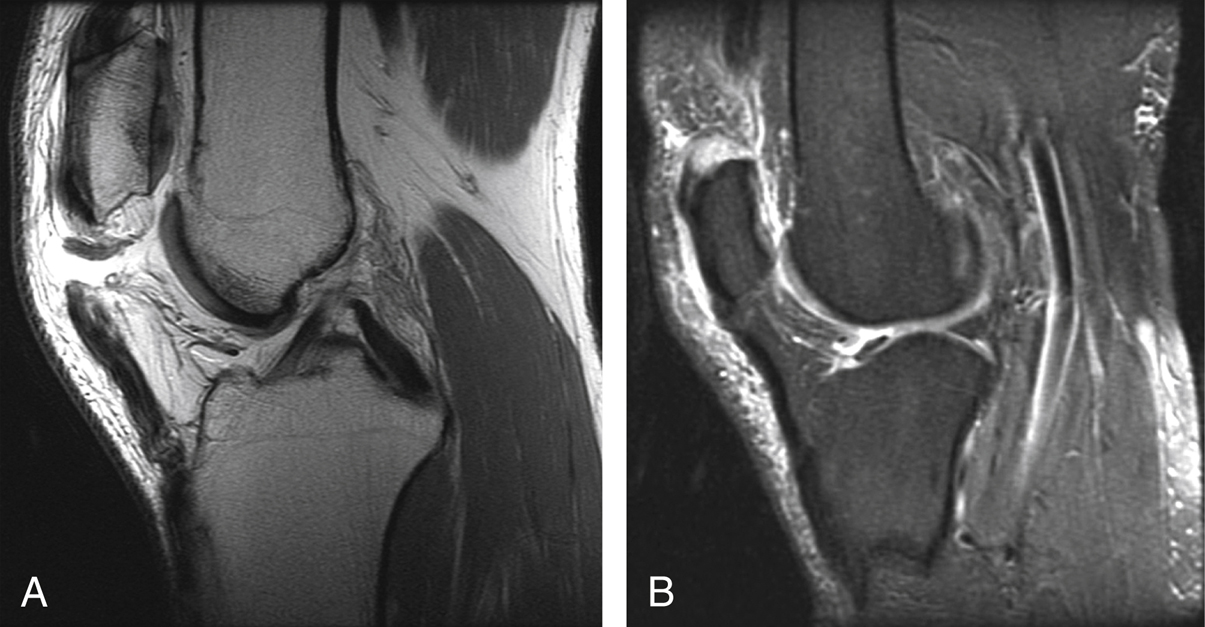
Figure 2Extensor mechanism injuries of the knee. A, Sagittal T1-weighted MRI demonstrates an acute patellar tendon rupture. B, Sagittal fluid-sensitive, fat-suppressed MRI demonstrates an acute quadriceps tendon tear.
Can accurately diagnose difficult cases (Figure 2)
Can identify concomitant injuries; 30% of patellar tendon tears and 10% of quadriceps tendon tears are associated with concomitant injuries, usually anterior cruciate ligament and medial meniscus tears
Procedure
Positioning and Preparation
Regional anesthesia
Supine position with bump under ipsilateral hip
Tourniquet
Examination under anesthesia to evaluate for soft-tissue injuries or confirm presence and extent of injuries identified on preoperative imaging
Quadriceps Tendon Repair
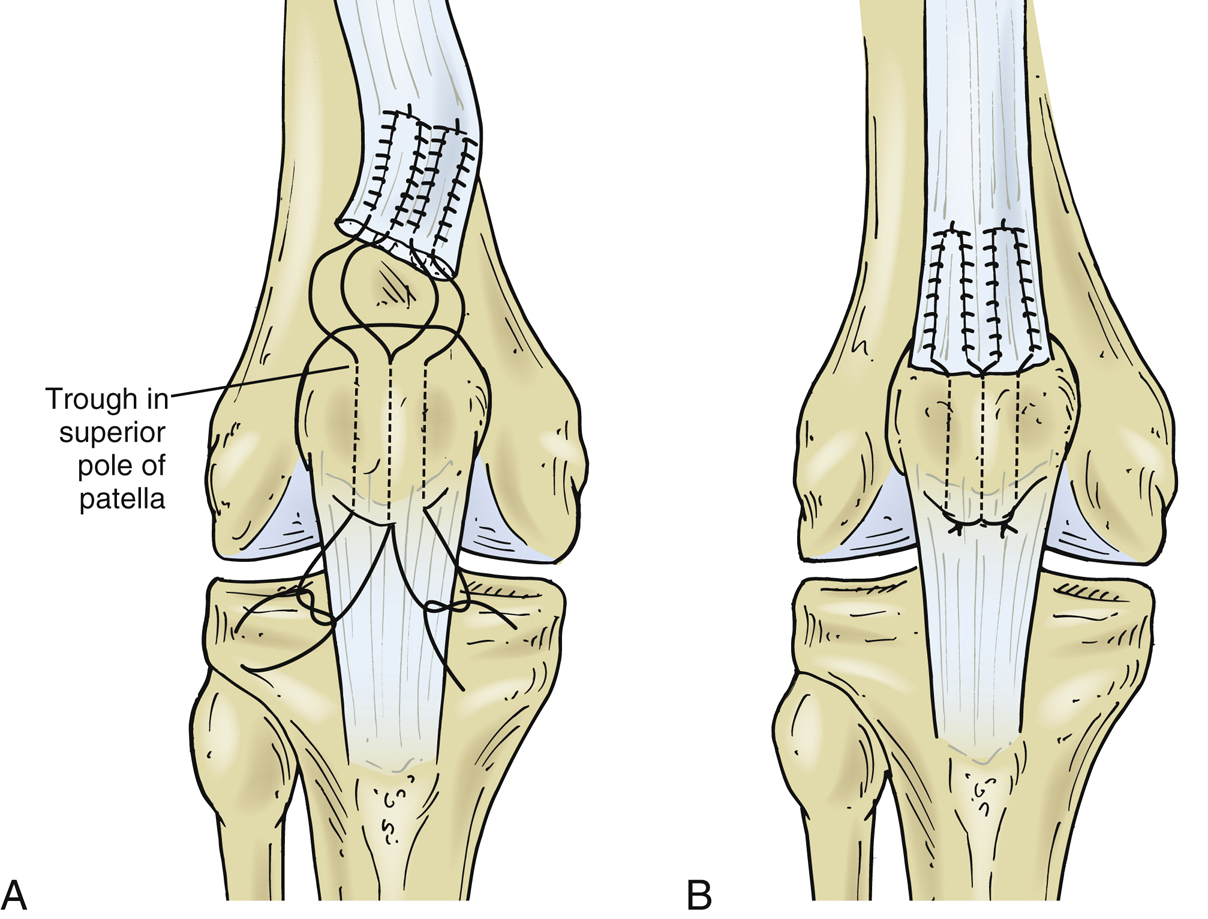
Figure 3Illustrations show acute quadriceps tendon repair. A, The four suture limbs of the Krackow stitch are passed through the three transosseous drill holes. B, The suture limbs are tied together over the patellar bone bridge.
For osteotendinous junction tear repair (Figure 3)
Most common repair is transosseous tunnel technique, which involves interlocking sutures through proximal tendon
Pass sutures through longitudinal transosseous patellar drill holes
Tie sutures over patellar bony bridge
On rare occasions you can do a quadriceps turndown technique or augmentated with an Achilles allograft
Use of suture anchors—recent biomechanical studies have demonstrated that suture anchors are equally as strong or superior to transosseous tunnels
Authors’ preferred technique for repair is using transosseous tunnels
Surgical Technique
Make midline longitudinal incision 5 cm proximal to superior border of patella extending to inferior pole of patella distally
Create full-thickness flaps down to extensor mechanism
Débride and irrigate scar tissue/hematoma
Deflate tourniquet to allow full mobilization of the tendon; hemostasis is achieved using electrocautery
Quadriceps Tendon Repair Using Transosseous Tunnels
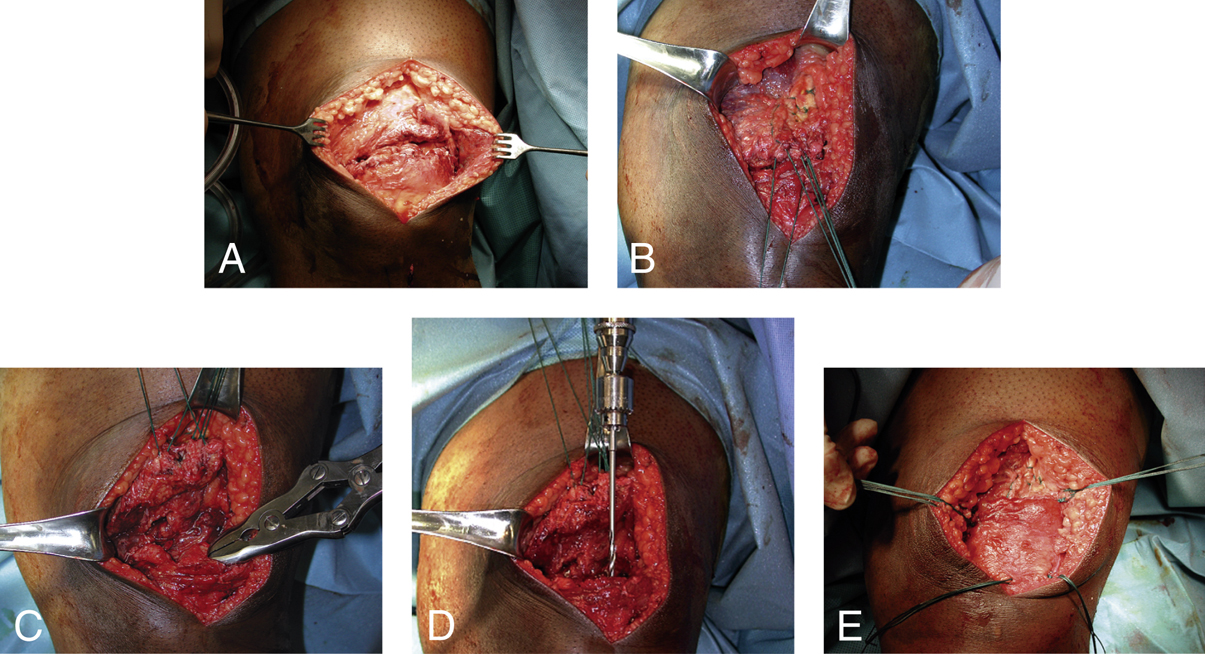
Figure 4Intraoperative photographs demonstrate the surgical repair of an acute quadriceps tendon rupture. A, Exposure of the tear. B, The quadriceps tendon is mobilized after two sutures are placed in the tendon using a Krackow stitch. C, Débridement of the superior patellar pole. D, Creation of the transosseous patellar tunnels using a 2.5-mm drill. Careful attention is paid to drill orientation to avoid iatrogenically violating the articular cartilage. E, Medial and lateral retinaculum repair.

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


