Surgical Treatment of Osteochondritis Dissecans Lesions
Introduction
Osteochondritis dissecans (OCD) is a pathologic joint disorder that affects the subchondral bone and the overlying articular cartilage.
Results in subchondral bone loss and destabilization of articular cartilage
End result is fragmentation of cartilage and bone that can progress to early degenerative changes and loss of function in the affected compartment.
Site of lesions
80% affect the medial femoral condyle (MFC), usually the lateral aspect of the MFC intersecting the intercondylar notch near the femoral footprint of the posterior cruciate ligament.
15% in lateral femoral condyle
5% in patellofemoral region
Course of treatment dependent on stability, which is most accurately determined arthroscopically. MRI only has 53% accuracy in determining stability.
Nonsurgical options
Can be successful in the case of a stable lesion and short duration of symptoms
Consists of hiatus from sports and high-impact activities for 6 to 8 weeks; normal weight bearing is allowed in the compliant patient.
“Relative rest program” can maintain joint health without compromising healing potential of a symptomatic OCD lesion; length of rest is highly variable and is a factor to consider when deciding whether to intervene surgically.
Surgical options
Fragment removal
Drilling (antegrade or retrograde)
Internal fixation
Marrow stimulation
Autologous chondrocyte implantation (ACI)
Osteochondral autograft/allograft transplantation
Joint arthroplasty—last resort in advanced cases.
Decision-making debate—Treat lesions early with cartilage restoration versus initial fragment excision, which leaves many patients clinically normal.
Patient Selection
Thorough history mandatory
Inciting events
Underlying metabolic or systemic conditions
Duration of symptoms
Previous treatments
Risk factors for OCD include:
Male sex
African-American race
Presence of discoid lateral meniscus
Family history of OCD
Active sports participation
Typical presentation
Pain and swelling related to activity
Mechanical symptoms such as catching or locking if fragment has destabilized or completely detached
Physical examination findings
Localized tenderness, antalgic gait, leg externally rotated while walking (Wilson sign)
Joint effusion, loose-body symptoms, reduced range of motion (ROM), and quadriceps atrophy are variably present
Indications
Failed nonsurgical management
Unstable fragment in an active, symptomatic patient
Can comply with postoperative weight bearing and activity restrictions
Classic location in MFC; this site has a resolution rate of less than 30%, but nonclassic lesions more likely to heal in adolescent population, with 88% to 100% healing rates with nonsurgical management.
Contraindications to Surgical Management
Physeal status stratifies OCD into juvenile OCD (JOCD) or adult OCD (AOCD).
Nonsurgical management recommended for stable lesion in JOCD
Activity modification has good outcomes in juveniles because of increased regenerative capacity from chondrocytes and mesenchymal cells.
Primary surgical fixation not recommended if lesion is free-floating loose body and underlying subchondral bone is compromised
Preoperative Imaging

Figure 1Magnetic resonance images show the appearance of an osteochondritis dissecans (OCD) lesion. A, T1-weighted sagittal view. B, T2-weighted sagittal view. C, T2-weighted coronal view of an OCD lesion presenting concomitantly with compromised subchondral bone. An area of high signal intensity between the OCD lesion and the subchondral bone suggests instability.
Crucial to diagnosis
Radiography
AP weight-bearing knee, weight-bearing 45° flexion PA, lateral, Merchant views
Open physes are a positive predictor for healing of an OCD lesion.
MRI (Figure 1)
Evaluate for bone edema, subchondral separation, cartilage breakdown, lesion size, lesion location.
Meeting one of the following four criteria offers up to 97% sensitivity and 100% specificity in predicting lesion stability.
A thin, ill-defined, or well-demarcated line of high signal intensity, measuring 5 mm or more in length at the interface between the lesion and underlying subchondral bone
A discrete, rounded area of homogeneous high signal intensity
A focal defect with a width of 5 mm or more in the articular surface of the lesion
A high signal intensity line traversing the articular cartilage and subchondral bone plate into the lesion
Procedure
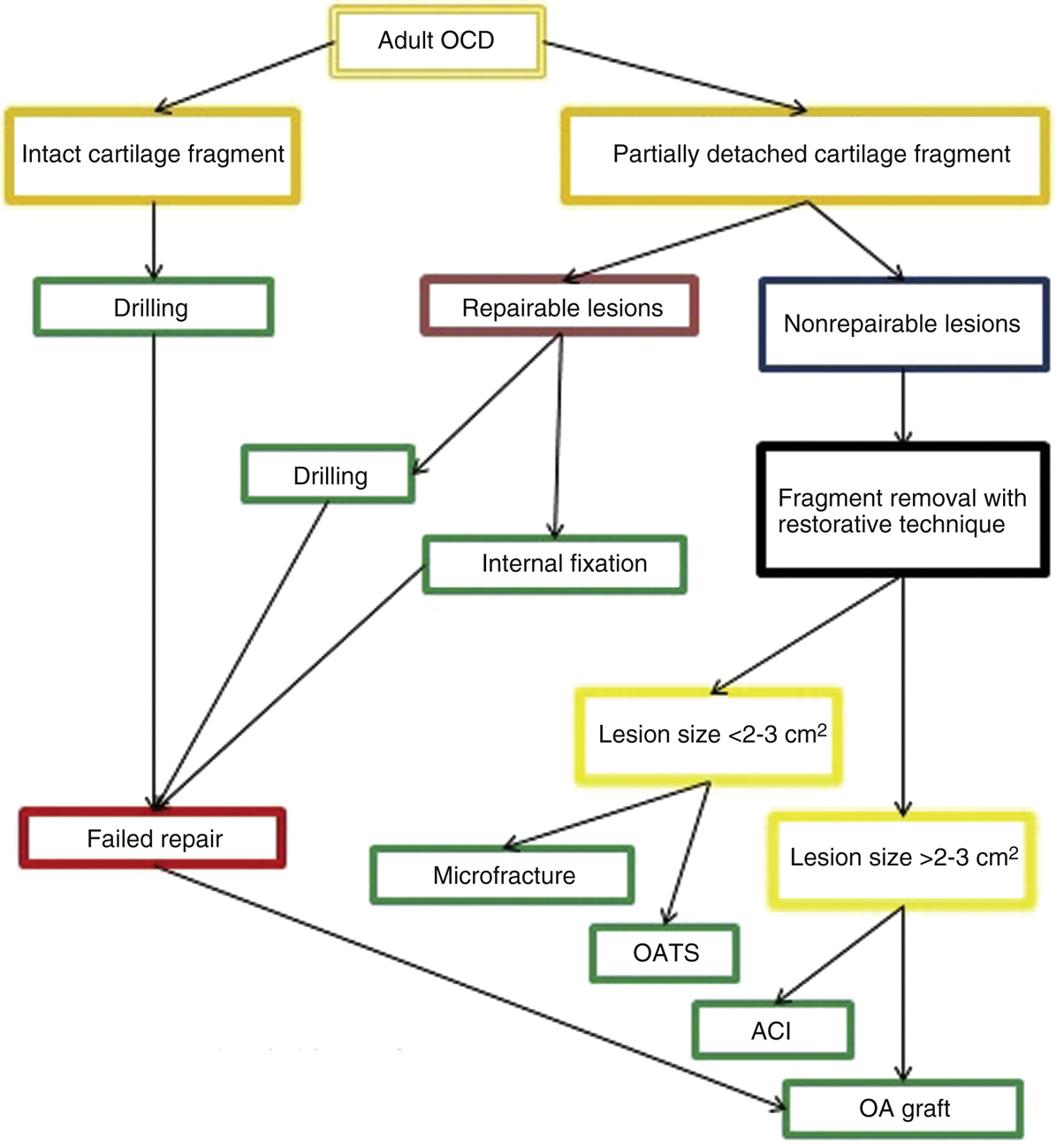
Figure 2Diagram depicts the surgical treatment algorithm for osteochondritis dissecans (OCD). The surgical goals should always incorporate an attempt to reestablish the joint surface using the least invasive procedure first. ACI = autologous chondrocyte implantation, OA graft = osteochondral allograft, OATS = osteochondral autograft transfer system
Goal—To enhance the healing potential of the subchondral bone, fix the unstable fragment, or replace the abnormal cartilage and bone with implantable tissue.
Surgical treatment algorithm determines the type and extent of surgery needed (Figure 2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


