Surgical Treatment of Navicular Stress Fractures
Patient Selection
Most common in patients who participate in high-impact or explosive athletics (sprinting, jumping) or long-distance running
Frequently missed; suspect if patient does not respond to treatments for other diagnosis; can be confused with posterior/anterior tibial tendinitis, midfoot sprain, ankle sprain
Classified as complete versus incomplete, displaced versus nondisplaced
Nonsurgical care is mainstay for complete nondisplaced and incomplete fractures; minimum of 6 weeks non–weight-bearing (NWB) immobilization
Noncompliance with NWB, immobilization leads to treatment failure
Preoperative Imaging
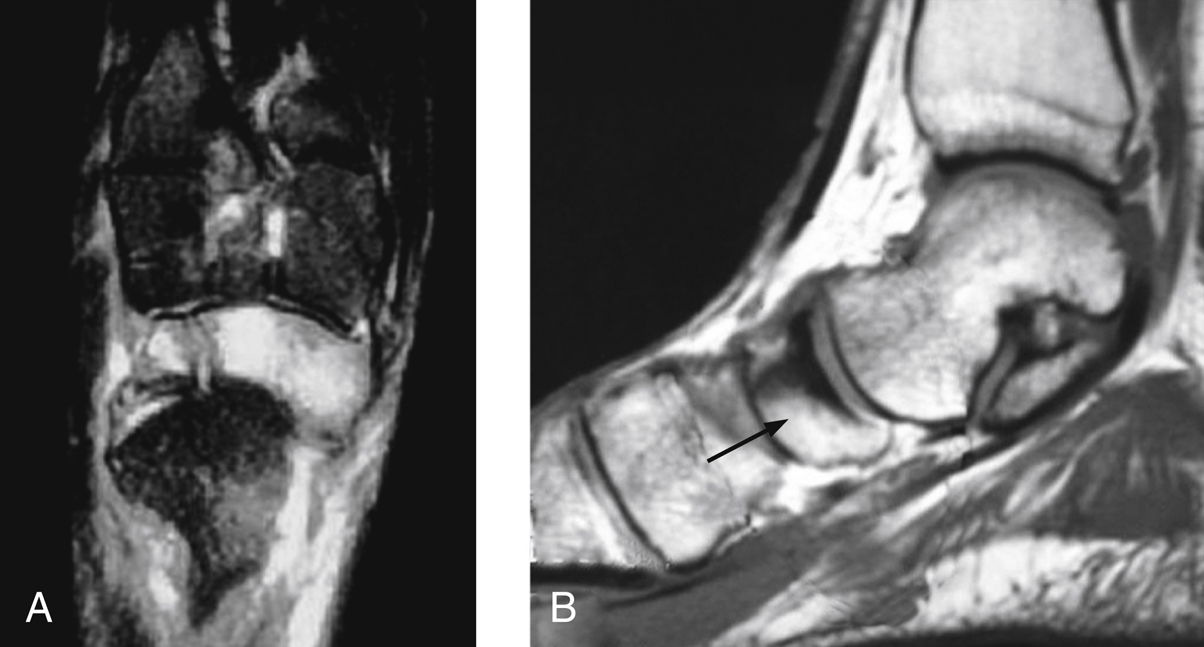
Figure 1Axial (A) and sagittal (B) magnetic resonance images show a navicular stress fracture (arrow) with associated bone edema and fracture line.
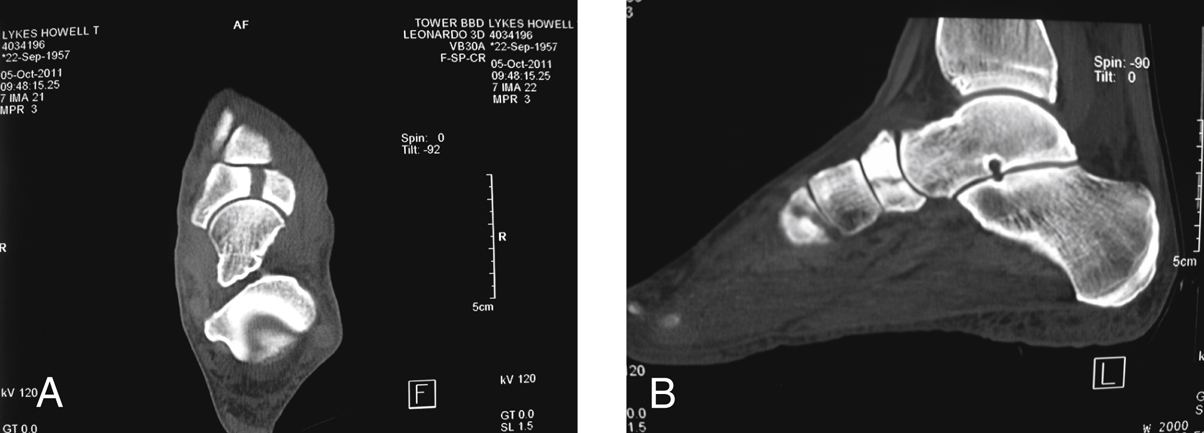
Figure 2Axial (A) and sagittal (B) CT scan cuts show a complete navicular stress fracture pattern.
Standard weight-bearing AP, oblique, and lateral radiographs of foot; often miss stress fracture, however
If radiograph negative but clinically suspicious, MRI is next examination (Figure 1); MRI may not identify fracture, requiring CT
If radiograph identifies fracture or sclerosis, CT is next examination (Figure 2)
Bone scans are sensitive but nonspecific for pathology
Most common fracture is incomplete and in central third of bone traversing from dorsal-medial to plantar-lateral
Procedure
Patient Positioning
Supine position with bump under ipsilateral hip
Tourniquet on thigh
Drape to allow for possible proximal tibial bone harvest
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


