Residual hip dysplasia, a well-known cause for early osteoarthritis (OA), is a relatively common disorder in children and adolescents. Three-dimensional imaging assessment has enhanced diagnosis and treatment by allowing clear identification of important pathomorphologic anatomy and cartilage degeneration. Treatment requires surgery with a goal of normalizing joint loading by increasing the contact area and improving the level arm of the hip to forestall the development of OA. Methods for correcting dysplasia in children and adolescents are described in this article.
- •
Residual hip dysplasia, a well-known cause for early osteoarthritis (OA), is a relatively common disorder in children and adolescents.
- •
Three-dimensional imaging, including CT and MRI assessment has enhanced the diagnosis and treatment of patients with dysplasia by allowing clear identification of important pathomorphologic anatomy and cartilage degeneration.
- •
Treatment of residual hip dysplasia requires surgery with a goal of normalizing joint loading by increasing the contact area and improving the level arm of the hip to forestall the development of OA.
- •
Proper selection and performance of a corrective acetabular osteotomy and adjunctive procedures to provide a well-covered femoral head are prerequisites for a good clinical outcome and high survivorship of the hip.
Introduction
The human hip develops in utero and evolves to a large polyaxial stable joint that under ideal circumstances can last a lifetime. Unfortunately, both genetic and acquired factors can prevent this ideal circumstance, leading to hip dysplasia and early secondary degenerative arthritis.
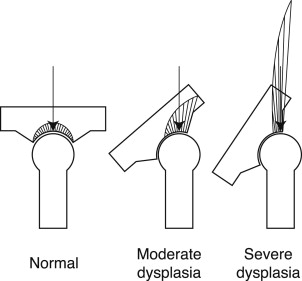
Modern neonatal diagnostic methods have minimized the late diagnosis of hip dysplasia, with ultrasound, allowing treatment in the first months of life. Despite this progress, however, some patients end up with residual hip dysplasia, which requires surgical treatment in childhood or adolescence. The goal of surgery is to convert shear forces to compression forces (for which the articular cartilage is well-designed to withstand) ( Figs. 1 and 2 ). Obviously, the earlier correction is provided, the greater the chance for normal development of the acetabulum and hip joint.

The goal of this article is to briefly describe the nature of residual hip dysplasia in childhood and adolescence and to present indications and methods for performing commonly used surgical procedures to correct hip dysplasia.
History and physical examination
Initial assessment should focus on the patient history, symptomatology, activity level, and functional limitations, if any.
The history should include any pertinent risk factors, such as breech-presentation, high birth weight for gestational age, or oligohydraminios. A family history of hip pathology should identify heredity factors, including a history of acetabular dysplasia and joint laxity in the family. Parents of children with hip dysplasia/hip dislocation may have observed a variety of features in their child, such as limping, walking on tiptoe, difficulty in crawling, and asymmetry of thigh creases, hip abduction, or leg length. Many children and adolescents are incidentally diagnosed following radiographs for other reasons and are asymptomatic.
Patients with residual dysplasia may be asymptomatic or experience slight discomfort with weight-bearing activities. Adolescents who additionally have a labral tear may experience catching or locking symptoms with occasional popping sensations in their hip joint. In older teenager and young adults, symptoms of continued pain should make the clinician suspect and evaluate for osteoarthritic (OA) changes. Finally, because dysplasia is often asymptomatic in the child and adolescent, many of the patients were treated or evaluated for hip dysplasia as infants and toddlers. Therefore, a detailed surgical history is often required.
History and physical examination
Initial assessment should focus on the patient history, symptomatology, activity level, and functional limitations, if any.
The history should include any pertinent risk factors, such as breech-presentation, high birth weight for gestational age, or oligohydraminios. A family history of hip pathology should identify heredity factors, including a history of acetabular dysplasia and joint laxity in the family. Parents of children with hip dysplasia/hip dislocation may have observed a variety of features in their child, such as limping, walking on tiptoe, difficulty in crawling, and asymmetry of thigh creases, hip abduction, or leg length. Many children and adolescents are incidentally diagnosed following radiographs for other reasons and are asymptomatic.
Patients with residual dysplasia may be asymptomatic or experience slight discomfort with weight-bearing activities. Adolescents who additionally have a labral tear may experience catching or locking symptoms with occasional popping sensations in their hip joint. In older teenager and young adults, symptoms of continued pain should make the clinician suspect and evaluate for osteoarthritic (OA) changes. Finally, because dysplasia is often asymptomatic in the child and adolescent, many of the patients were treated or evaluated for hip dysplasia as infants and toddlers. Therefore, a detailed surgical history is often required.
Examination
Physical examination should include inspection of the extremities for limb-length discrepancy, angular or torsional malalignment of the limb, provocative testing for hip instability, and evaluation of hip motion, including assessment of difference in abduction. Gait analysis may reveal a very subtle limp in early childhood or Trendelenburg gait in an older child. Timed Trendelenburg test (10–20 seconds) allows for the assessment of relative abductor muscle weakness. Pelvic obliquity and spinal alignment for scoliosis should be tested. Pain elicited by hip flexion, adduction, and internal rotation (positive impingement test) can be potentially caused by a torn labrum or an acetabular rim syndrome, which is associated with a limbus or bone fragment that has detached from the rim of the acetabulum. Of note, children with untreated hip dysplasia often have normal hip motion and no pain.
Imaging
Standard Radiography
Plain radiographic evaluation of hips aids in the comprehensive assessment of hip dysplasia, helps monitor hip development, may guide treatment, and also assists in assessment of treatment outcomes. This includes an anteroposterior (AP) pelvis and a lateral radiograph at a minimum. A false- (faux-) profile image may be helpful in certain patients depending on their age and severity of dysplasia. Pelvic rotation and pelvic tilt should be considered for appropriate assessment of morphology.
Several radiographic parametric indices are helpful in evaluating the skeletally immature hip, including the Hilgenreiner line, the Perkins-Ombrédanne line (drawn at the lateral margin of the acetabulum perpendicular to the Hilgenreiner line), and the Shenton arc (line).
Further measurements can be performed to stratify or grade the severity of hip dysplasia, including the acetabular index, Tonnis angle, lateral center-edge angle (LCA) of Wiberg, and, after fusion of the triradiate cartilage (in adults) the acetabular angle of Sharp. The presence of a crossover sign and a prominent ischial spine are indicators for acetabular retroversion, which although rare, may be associated with hip dysplasia.
The false-(faux-) profile view as described by Lequesne and de Sèze in 1961 allows for the assessment of the ventral center-edge angle (angle formed between a vertical line through the center of the femoral head and a line extending through the center of the femoral head to the anterior sourcil) as a potential determinant of the anterior acetabular coverage.
The appearance of the acetabular sourcil is a sensitive radiographic feature of symmetric or asymmetric loading of the hip joint. This dense subchondral bone normally appears as a smooth curve with uniform thickness, forming the base of the so-called “Gothic Arch” with craniomedially and craniolaterally extending groups of trabeculae that meet above the sourcil to complete the arch. In the dysplastic hip, the sourcil appears tilted rather than level, and lateral sourcil thickening occurs, which represents increased focal loading related to the underlying malalignment of the joint.
Femoral torsion may be evaluated using a Dunn-Rippstein radiograph ; however, precise torsion profile assessment is feasible only by means of computed tomography (CT) or magnetic resonance (MR) imaging.
In older patients, radiographic examination of the hip joint in various positions can be valuable to evaluate the effect of a proposed osteotomy. For example, an abduction internal rotation radiograph reveals whether the femoral head can be concentrically reduced into the acetabulum. This view neutralizes femoral anteversion and allows accurate calculation of the femoral neck-shaft angle.
Acetabular dysplasia can be either associated with stable articulation or with articular instability including hip subluxation and hip dislocation. A patient with hip dysplasia has morphologic abnormalities of the acetabulum and/or femoral head with an intact Shenton line, whereas a patient with subluxation has anatomic abnormalities of the femoral head and/or acetabulum and a disruption of the Shenton line.
The long-term outcome after corrective hip osteotomy correlates with preexisting joint degeneration with less predictable findings in patients with preexisting OA changes. The degree of OA of the hip can be graded according to the Tönnis criteria ; however, detection of early cartilage changes, which is important for treatment and prognostication, remains a challenge and, as such, hip joint degeneration may be advanced by the time the diagnosis of OA is made based on plain radiography.
Advanced Imaging
Advanced imaging studies, such as MRI, MR arthrography, or CT examination with 3-dimensional (3D) reconstruction may be indicated in patients with severe hip dysplasia and/or patients who present late to (1) determine the exact location and character of the deformity, and (2) to reliably assess the status of hip joint structures (ie, cartilage and labrum), which is essential for surgical decision making, treatment planning, and prognostication. The 3D evaluation provides superior information about the fit of the femoral head inside the acetabulum, as well as the size, shape, and orientation of both the acetabulum and femur ( Fig. 3 ). Furthermore, CT or MRI examination, including torsional profile assessment may be indicated to define the exact degree of femoral and acetabular anteversion.
With advances in hip preservation surgery, accurate assessment of joint cartilage status that includes detection of biochemical changes is becoming increasingly important (discussed in the article by Y.J. Kim, elsewhere in this issue).
Surgical treatment—basic principles
In hip dysplasia, joint overloading occurs at the rim of a short and shallow acetabulum. Two main components account for joint overloading: (1) increased muscle forces about the hip, and (2) decreased load-transferring weight-bearing surface area related to the shortness and obliquity of the dysplastic hip. Shear forces originating from the oblique acetabulum further contribute to lateralization of the hip joint center. Eventually, progressive cartilage degeneration associated with soft-tissue impairment, such as labral damage and degeneration, may develop.
The goal of surgical treatment is to reduce the joint loading by increasing the contact area, relaxing the capsule and muscles about the hip, and improving the lever arm of the hip to restore hip biomechanics, provide joint stability, and potentially forestall the development of OA. In infants and younger children, the restoration of hip-joint concentricity may set the stage for subsequent remodeling, whereas relieving symptoms, maintaining or improving activity and quality of life, and delaying the total hip arthroplasty may be the more limited goal in patients with more severe hip dysplasia.
Many hip osteotomies and soft tissue procedures to accomplish these goals have been reported that vary depending on the patient’s age, severity of dysplasia, morphology of the hip joint, coexisting soft tissue pathology, preexisting OA, and surgeon comfort. These procedures include femoral procedures, such as derotation, varization, and shortening femoral osteotomies, and pelvic osteotomies, such as Salter innominate osteotomy, juxta-articular double osteotomy, triple pelvis osteotomies, periacetabular osteotomies (PAOs), Pemberton pericapsular osteotomy, and Dega transiliac osteotomy.
Spherical osteotomies described by Wagner, Eppright, and others may be used to cover severely dysplastic hips; however, these procedures are technically difficult and are prone to complications, such as inadvertent penetration of the acetabulum and/or avascular necrosis.
Age-Related Indications
Residual hip dysplasia can be a major cause of disability and is best corrected at an early age. Previous studies have demonstrated that early surgical correction of residual dysplasia will delay or prevent the onset of premature arthritis. Furthermore, in younger children, residual hip dysplasia or subluxation may be more predictably corrected, with better clinical and radiographic results, less morbidity, and fewer complications. However, the debate about the minimum age, at which a hip osteotomy should be performed remains controversial. On the assumption that the potential for acetabular remodeling is significantly reduced after the age of 18 months, Salter and coworkers proposed his procedure to be done after that age, whereas others believe that pelvic osteotomy has limited indications in children younger than 5 years.
Acetabular osteotomies are characterized as redirectional or reshaping procedures that are performed either as a reconstructive or a salvage procedure. Complete acetabular procedures, such as the Salter, triple pelvic (TPO), or Bernese PAO, improve the coverage of the femoral head by redirecting the acetabulum. The shape of the acetabulum itself remains unchanged. Reshaping osteotomies, such as the Pemberton or Dega osteotomy, change the shape of the acetabulum. Because redirectional procedures involve complete cuts through the innominate bone, fixation is required to maintain the new alignment until the osteotomy heals, whereas reshaping osteotomies in general do not require additional fixation.
The Salter single innominate osteotomy or reshaping procedures (ie, Pemberton or Dega osteotomy) may be used for dysplastic hips in younger children (younger than 8 or 9 years). In older children and adolescents, where the acetabulum may have to be displaced to a greater degree to provide sufficient coverage of the hip, procedures including the TPO and PAO are used. This article focuses on osteotomies (ie, Salter osteotomy, TPO) that do not cross the triradiate acetabular growth cartilage and can be used in the growing child. In contrast, the PAO (described in a later article in this issue) is performed in mature adolescents and young adults in whom the triradiate growth cartilage is closed.
Finally, the ability to concentrically reduce and maintain the femoral head within the acetabulum must be analyzed when surgical treatment is considered. In severe cases, a simultaneous femoral osteotomy may be needed.
Incongruent Hip Joint
Joints that are relatively incongruent and cannot be concentrically reduced, or those that reveal notable changes of degeneration, may benefit from “salvage” procedures, such as the Chiari osteotomy or Staheli shelf procedure. However, whereas reconstructive procedures have a relatively predictable outcome, the main expectation from any kind of salvage procedure is to help relieve pain, delay the inevitable hip arthroplasty, and possibly improve function in the meantime.
Proximal femoral osteotomy
A proximal femoral shortening osteotomy is commonly performed with primary hip dislocation to decrease the compressive forces on the femoral head after the reduction to potentially decrease the risk of avascular necrosis. When a child with hip dislocation is older than 2 years, a combined open reduction and acetabular procedure with a proximal femur osteotomy (varus derotation with/without shortening) may be performed. In the past, proximal varus derotation osteotomy (which was acclaimed as a technically easier procedure as compared with pelvic osteotomy) was used in younger children with hip dysplasia with the consideration that concentric reduction served as the primary stimulus for acetabular remodeling. Lalonde and colleagues noted that isolated varus osteotomy was unpredictable for correcting hip dysplasia, even in children as young as 4 years.
Spence and colleagues compared acetabular development in children of walking age managed for dislocation of the hip with open reduction combined with either a femoral varus derotation osteotomy or an innominate osteotomy, noting that acetabular remodeling after open hip reduction and innominate osteotomy was more effective for reversing acetabular dysplasia and maintaining hip stability than open reduction combined with a femoral varus derotation osteotomy.
In our current practice, we do not perform an isolated varus osteotomy to correct residual hip dysplasia in childhood. Femoral osteotomy is sometimes performed in combination with an acetabular procedure in cases of severe dysplasia with high subluxation.
Redirectional acetabular osteotomies
Salter Innominate Osteotomy
Described by Salter in 1961, the single innominate osteotomy was reported as a method to add immediate stability when reducing a completely dislocated hip in children older than 18 months (described in an earlier article in this issue). The Salter innominate osteotomy has also been commonly used to correct residual dysplasia in childhood up to about age 10 years. The procedure is widely used owing to its long track record and relative ease of performance (if the surgeon is properly trained).
The Salter procedure provides improved anterolateral coverage by redirecting the acetabulum without changing acetabular shape or volume ( Fig. 4 A). The primary indication for the Salter procedure is, therefore, deficiency in anterolateral coverage in an otherwise concentrically reduced hip in children between 2 and 10 years of age. The undersized acetabulum is redirected, avoiding the risk of an acetabular bending procedure that might decrease the size or volume of the acetabulum. Depending on age and acetabular fragment mobility through the pliable fulcrum of the pubic symphysis, adequate improvement in the LCA as well the acetabular index may be expected.
Children younger than 2 years may have inadequate iliac bone to support pin fixation, whereas in children older than 10 years, the decreased flexibility of the pubic symphysis prevents sufficient movement of the acetabular fragment. A steep, shallow elongated acetabulum is a relative contraindication and may be better treated with a reshaping procedure.
Procedure
The hip is approached through the anterolateral Smith-Peterson interval, which is, in the children’s orthopedic world, usually referred to as the Salter approach. The inner and outer tables of the iliac wing are exposed subperiosteally and a straight osteotomy is made with a Gigli saw from the sciatic notch to the anterior-inferior iliac spine. Adequate exposure and proper subperiosteal clearing of the sciatic notch is required to prevent injuries of neurovascular structures.
The Salter procedure mildly increases limb length and also increases tension on the muscles that cross the hip anteriorly. Therefore, an iliopsoas intramuscular lengthening at the pelvic brim is performed to decrease compression on the femoral head and enhance distal fragment mobility.
The acetabular portion is pulled forward and rotated slightly anterolateral by rotating through the flexible fulcrum of the pubic symphysis with the proximal fragment held in place, leaving the posterior site of the osteotomy closed. Inadvertent opening of the osteotomy posteriorly displaces the hip joint distally, resulting in leg lengthening and less acetabular coverage. A towel clamp placed in the iliac bone just above the acetabulum can be used as a handle to guide the displacement and rotation of the acetabulum.
If the capsule is intact, the displacement of the acetabular fragment may be further facilitated by placing the patient’s leg into a figure-of-4 position (hip flexion, abduction, and external rotation) while being careful to prevent retroversion. In his description of the procedure, Salter emphasized that when the acetabular fragment is rotated forward, the anterior superior and inferior iliac spines should be kept aligned. Although the concept was not described as such, he meant “avoid creating acetabular retroversion”—a concept now well appreciated, as excessive acetabular retroversion can be a risk factor for early hip arthritis.
A triangular bone graft, taken from the anterior-superior iliac spine area, is placed into the osteotomy and the osteotomy is fixed with threaded K-wires. One pin directed behind the acetabulum and one superior and medial to the acetabulum transfix the bone graft. Image intensifier views ensure proper correction and fixation.
Postoperative treatment includes 6 weeks in a single hip spica cast followed by 3 additional weeks of partial weight-bearing.
Salter variant
Salter emphasized that the iliac osteotomy should be complete to allow sufficient anterior and lateral movement of the acetabulum; however, this mobility increases the risks associated with the procedure (ie, posterior slippage and loss of fixation) (see Fig. 4 B).
Accordingly, when treating hip dysplasia alone (not in association with open reduction), we often use a power saw for the anterior two-thirds of the osteotomy cut and then an osteotome, cutting the bone to a point just anterior to the sciatic notch. The osteotomy is then hinged opened, leaving the posterior cortex intact. The bone graft and K-wire fixation are the same as in the traditional Salter procedure (see Fig. 4 C). The result is a safe, stable Salter procedure with little risk for inadvertent displacement and/or loss of fixation.
Triple Pelvic Osteotomy
In older children (>8 years), hinging and rotation on the triradiate cartilage or pubic symphysis becomes more difficult because of skeletal maturity and decreased ligamentous laxity. One can still perform a Salter innominate osteotomy in this age group but dysplasia correction may be insufficient, especially in severe grades of dysplasia. Furthermore, potential upward migration and/or rotation of the proximal segment through the sacroiliac joint can lead to a loss of correction over time. Therefore, residual hip dysplasia in older children is managed better with a TPO. After closure of the triradiate cartilage, the Bernese PAO can be considered an alternative to the triple innominate osteotomy.
The TPO was first described by Steel, but due to editorial dating errors by a journal, was attributed to Le Coeur. Briefly summarized, the approach includes a transverse osteotomy of the ilium through a Smith-Peterson approach just above the acetabular roof and cutting of the superior and inferior pubic rami. The acetabulum was then rotated laterally and anteriorly to improve coverage of the femoral head.
Since then, several modifications of the original TPO, including the Tönnis and the Carlioz procedures, have been described; however, the principle of the triple innominate osteotomy remains the same: it involves osteotomies of the ischium and pubis in addition to the iliac osteotomy to allow free mobility and rotation of the acetabular fragment ( Fig. 5 ).








