Surgical Treatment of Dupuytren Disease
Ghazi Rayan
DEFINITION
Dupuytren disease (DD) is a fibroproliferative disorder that affects primarily the palmar fascia of the hand, with occasional secondary involvement of other areas in the hand as well as remote tissues.
DD has a strong genetic origin that is suggested not only by population studies and family clustering but also by genomewide association study,15 which suggest that chromosomes 6, 11, and 16 may contain genes for the disease and that multiple other genes may be involved in its etiology.
It is a sui generis condition that clinically and pathophysiologically resembles no other known condition.
Although physiologically DD bears a resemblance to the processes associated with normal wound healing, the difference is the perpetual and progressive proliferation with abnormal collagen deposition and resultant tissue contracture.
Attempts to classify DD under other headings such as inflammatory and neoplastic disorders have not been born out.
ANATOMY
The radial; ulnar; and central aponeuroses, palmodigital fascia, and digital fascia are elements of the palmar fascia.17
The radial aponeurosis has four components:
Thenar fascia, which is an extension of the central aponeuroses
Thumb pretendinous band, which is small and ill defined
Distal and the proximal commissural ligaments
The ulnar aponeurosis has the following components:
Hypothenar muscle fascia, which is an extension of the central aponeurosis
Pretendinous band to the small finger, which is consistent and substantial
Abductor digiti minimi muscle confluence
Pisiform ligament complex
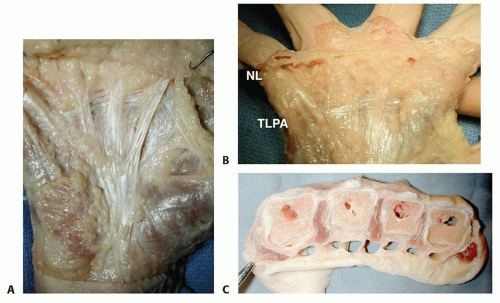
The central aponeurosis is the core of DD activity and has a triangular shape with a proximal apex (FIG 1A).
Its fibers are oriented longitudinal, transverse, and vertical.
The longitudinal fibers fan out as pretendinous bands to the three central digits (index, middle, and ring). Each pretendinous band bifurcates distally and each bifurcation has three layers. The superficial layer inserts into the dermis, the middle layer continues to the digit as the spiral band, and the deep layer passes almost vertically dorsally toward the flexor tendon digital sheath.
The transverse fibers make up the natatory ligament (NL) located in the distal palm and the transverse ligament of the palmar aponeurosis (TLPA). The TLPA is proximal and parallel to the NL (FIG 1B) and lies deep to the pretendinous bands. Its distal radial extent is the proximal commissural ligament. The TLPA gives origin to the septa of Legueu and Juvara, which protect the neurovascular structures and provide an additional proximal pulley to the flexor tendons.
The vertical fibers of the central aponeurosis are the minute but strong vertical bands of Grapow and the septa
of Legueu and Juvara (FIG 1C,D), which lie deep to the palmar fascia. There are eight of these septa that form seven fibro-osseous compartments3 of two types: four flexor septal canals that contain the flexor tendons and three web space canals that contain common digital nerves and arteries and lumbrical muscles. These septa insert in a soft tissue confluence that consists of five structures: A1 pulley, palmar plate, sagittal band, interpalmar plate ligament (IPPL; FIG 1D,E), and septum of Legueu and Juvara.
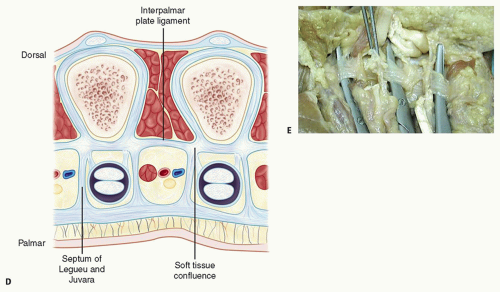
FIG 1 • (continued) D. IPPL and septum of Legueu and Juvara. E. There are three IPPLs: radial (to the left), central, and ulnar (to the right). These form the floor of the three web space canals.
The palmodigital fascia encompasses a number of fascial structures, including the terminal fibers of the pretendinous bands, the spiral bands, the beginning of the lateral digital sheet, and the NL. The middle layer of the bifurcated pretendinous band spirals about 90 degrees and the peripheral fibers run vertically adjacent to the metacarpophalangeal (MCP) joint. They continue distally deep to the neurovascular bundle and NL and emerge distal to this ligament and contribute to the formation of the lateral digital sheet. The proximal fibers of the NL run in a transverse plane, but the distal fibers form a “U” that continues longitudinally along both sides of the digit, forming the lateral digital sheet. The lateral digital sheet therefore has deep and superficial contributions from the spiral band and NL.
The digital fascia surrounds the neurovascular bundle in the digit and this includes the Grayson ligaments (palmar), the Cleland ligaments (dorsal), the Gosset lateral digital sheet laterally, and possibly fibers from the checkrein ligaments medially and dorsally, which were described previously as the Thomine retrovascular fascia.
PATHOGENESIS
In DD, normal bands become diseased cords,13 and Dupuytren nodules and cords are pathognomonic of the disease.14
A nodule usually appears first, followed by the cord.
The cords form in the palmar, palmodigital, or digital regions and progressively shorten, leading to joint and soft tissue contractures.
The Grapow vertical bands become microcords, leading to thickening of the skin, which is one of the earliest manifestations of DD.
Skin pits develop from the diseased first layer of the split pretendinous band.
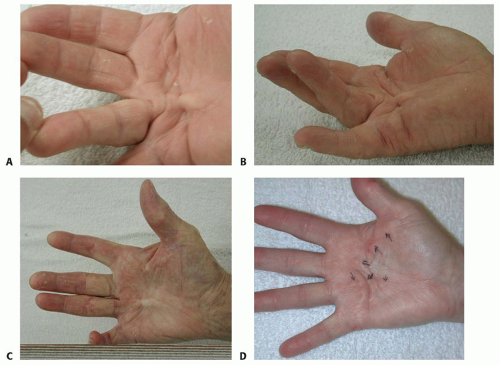
The pretendinous cord develops from the pretendinous band and is the most common cord in DD. It leads to MCP joint flexion deformity and often extends distally, contributing to the digital cords. The pretendinous cord may bifurcate distally with each branch extending into a different digit, forming a commissural Y cord (FIG 2).
The vertical cords, or diseased septa of Legueu and Juvara,2 are short and thick. They are connected to the pretendinous cord and extend deeply in between the neurovascular bundle and flexor tendon fibrous sheath.
Extensive palmar fascial disease is encountered in severe conditions and affects larger areas of the palm, leading to diffuse thickening of many components of the palmar fascial complex.
The spiral cord has four components: the pretendinous band, the spiral band, the lateral digital sheet, and the Grayson ligament. It is encountered most often in the small finger, but it may be present in the ring finger.
In the palm, this cord is located superficial to the neurovascular bundle. Distal to the MCP joint, it passes deep to the neurovascular bundle, and in the digit, it runs lateral to the neurovascular bundle as it involves the lateral digital sheet and again becomes superficial to the neurovascular bundle as it involves the Grayson ligament.
Initially, the cord spirals around the neurovascular bundle, but as it contracts, the cord straightens and the neurovascular bundle spirals around the cord.
The distorted anatomy of the neurovascular bundle, which is displaced medially and centrally, and later also proximally, is at risk for injury during surgery.23
The natatory cord develops from the NL, converting the U-shaped web space fibers into a V shape, resulting in contracture of the second to fourth web spaces.
This cord extends along the dorsal lateral aspect of the adjacent digits and is best detected by passively abducting the digits and at the same time flexing one digit and extending the other at the MCP joints.
The most commonly encountered digital cord is the lateral cord, followed by the central and spiral cords. These are responsible for proximal interphalangeal (PIP) joint flexion contractures.
The central cord is an extension of the pretendinous cord in the palm.
The lateral cord originates from the lateral digital sheet and attaches to the skin or to the flexor tendon sheath near the Grayson ligament. The lateral cord causes a contracture of the PIP joint but can also rarely cause a distal interphalangeal joint contracture.
The abductor digiti minimi cord, also known as the isolated digital cord, takes origin from the abductor digiti minimi tendon but may also arise from adjacent muscle fascia at the base of the proximal phalanx.
It courses superficial to the neurovascular bundle and infrequently entraps and displaces the bundle toward the midline.
It inserts on the ulnar side of the base of the middle phalanx but may attach on the radial side or have an additional insertion in the base of the distal phalanx, causing a distal interphalangeal joint contracture.
The distal commissural cord develops from the diseased distal commissural ligament, which is the radial extension of the NL. The proximal commissural cord originates from the proximal commissural ligament, which is the radial extension of the TLPA.
Both of these cords cause first web space contracture.
The thumb pretendinous cord originates from the thumb pretendinous band and causes thumb MCP joint flexion deformity, which is uncommon.
NATURAL HISTORY
DD has three clinical phases: early, intermediate, and late.16
Skin changes with loss of normal architecture and skin pitting characterize the early phase.
Nodules and cords form during the intermediate phase.
Contractures mark the late phase, with the MCP joint most frequently affected, followed by the PIP joint.
PATIENT HISTORY AND PHYSICAL FINDINGS
The classic DD patient is a Caucasian man with a positive family history. The condition is bilateral and progressive and may extend to the digits, leading to their contracture.
Palmar involvement usually precedes disease extension into the digits, but the disease may begin and remain in the digits.
The ring finger is the most commonly involved digit, followed in order of frequency by the small, middle, and index fingers, and last by the thumb.
DD may affect areas outside the palmar surface of the hand.
Ectopic disease can be either regional in the upper extremity or distant in other parts of the body.
Garrod nodes are different from knuckle pads, occur on the dorsum of the hand, and are almost always limited to the finger (FIG 3). We have shown that DD nodules are pathognomonic of DD, whereas knuckle pads demonstrate similar prevalence in normal and DD populations.18
Distant ectopic DD affects the plantar fascia and male genitals.
Patients said to express a Dupuytren diathesis or genetic predisposition typically have faster and more severe development of the condition.
Positive family history
Young age of onset
Ectopic sites of fibromatosis such as the dorsal digital area (Garrod nodes), plantar fascia (Ledderhose disease), and male genitals (Peyronie disease)
DIFFERENTIAL DIAGNOSIS
Non-DD19
Occurs in a diverse ethnic group, is unilateral and nonprogressive, usually involves a single digit, and frequently follows trauma or surgery
Patients with this disease rarely require surgical treatment. Confusing this with DD will produce contrasting epidemiologic data.
Epithelioid sarcoma
Occupational thickening and callus formation that mimic Dupuytren nodules
Palmar subcutaneous soft tissue lesions, such as localized pigmented villonodular synovitis, palmar ganglions, and inclusion cysts
Stenosing tenosynovitis without triggering can be associated with thickening and adherence of the skin to the underlying flexor tendon sheath.
Prominent flexor tendons can be confused with pretendinous cords because of attenuation of annular pulleys, as seen in rheumatoid arthritis.
NONOPERATIVE MANAGEMENT
No treatment is necessary for non-DD.
Observation is appropriate for nonprogressive DD with minimal contracture and without compromise of function.
Surgical treatment for minor disease or pitting can result in a disease flare and must be avoided.
Basic science research has shown the potential of certain local agents in the treatment of DD. These include calcium channel blockers, nifedipine, and verapamil,20 especially for early stages of the disease.
Steroid injection of nodules has been used to suppress the disease.
MINIMALLY INVASIVE TREATMENT METHODS
Percutaneous fasciotomy was used initially by the British surgeon Sir Astley Cooper in the early 19th century. The appeal for this procedure has recently reemerged in the pursuit of lower morbidity and fewer complications that may be encountered with conventional open surgical treatment.
Needle aponeurotomy and collagenase1,10 injection have recently been used for DD more broadly by treating surgeons and gained appeal among patients because of their “noninvasive” nature. These procedures, however, are mistakenly labeled as nonoperative treatment methods. In fact, these are minimally invasive procedures, which create distinct deep soft tissue wounds with the potential for accidental injury to neurovascular structures or infection.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree