Surgical Treatment of Cubital Tunnel Syndrome
The authors wish to recognize the work of John Dupaix, MD and Wayne Chen, MD for their contributions to this chapter.
Introduction
Occurs at elbow as a compressive neuropathy of the ulnar nerve
Second most common peripheral nerve compression syndrome after carpal tunnel syndrome
Patient Selection
Physical Examination
Inspect for muscle atrophy/weakness, sensory deficits, Tinel sign at the cubital tunnel, results of elbow flexion test and cubital tunnel compression test. The ulnar nerve is evaluated for any subluxation or instability
Examine ulnar innervated muscles, particularly FDP to the ipsilateral small finger. M4 motor strength indicates early compression of the ulnar nerve in the cubital tunnel
Finally, document the range of motion of the elbow joint and examine the ulnar nerve for subluxation
Electrodiagnostic Testing and Preoperative Imaging
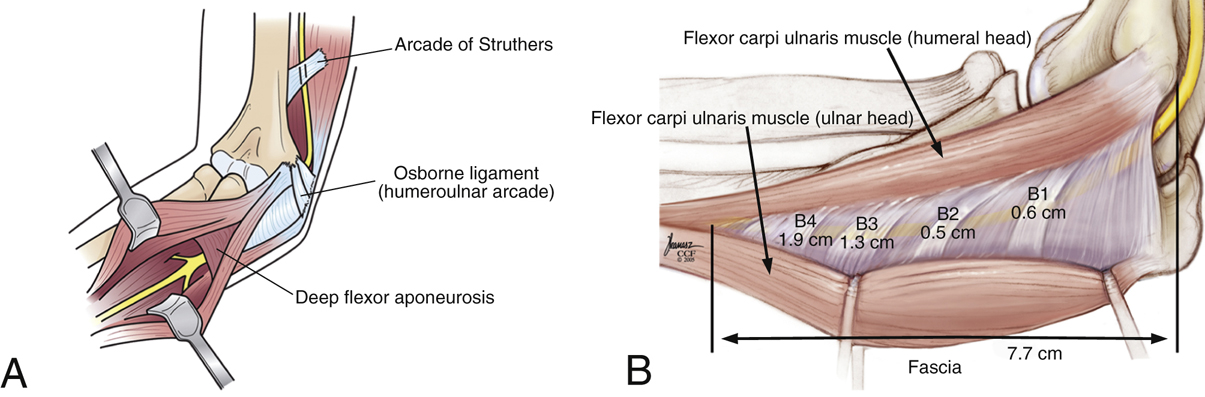
Figure 1Illustrations depict the anatomy of the cubital tunnel. A, The most common sites of ulnar nerve compression are labeled. B, Additional potential sites of compression of the ulnar nerve located in the submuscular membrane of the flexor-pronator muscle. (Panel B copyright Joe Kanasz, the Cleveland Clinic Foundation, Cleveland, OH.)
Electrodiagnostic testing (electromyography and nerve conduction velocity tests) is often obtained to support the diagnosis, exclude alternative diagnoses, or determine the extent of nerve changes; however, these studies are not always abnormal in early cases
Radiographs in at least two projections may be obtained in some cases
Ultrasonography and MRI are gaining importance in detecting morphologic changes in select cases, but are generally not necessary for most patients as cubital tunnel syndrome is a clinical diagnosis
CT is recommended only in the setting of skeletal deformity (Figure 1)
Indications and Contraindications
Regardless of technique, a few principles are important and common for each technique: complete decompression of compressive structures, assuring the nerve is in hospitable environment, avoiding iatrogenic injury to medial antebrachial cutaneous nerve, and assessing for nerve instability following end of procedure
Recent studies in the literature suggest that endoscopic cubital tunnel release procedures compare favorably to open in situ decompression
Cubital tunnel decompression may be indicated in patients with failure of nonsurgical treatment
In Situ Decompression
Room Setup/Patient Positioning
Outpatient setting
General anesthesia preferred
Supine position with shoulder abducted 90°, elbow flexed, forearm supinated
Apply well-padded tourniquet around upper arm
Special Instruments/Equipment/Implants
Karl Storz endoscopy set for endoscopic decompression; includes illuminated speculum, 30° endoscope, endoscopic bipolar forceps
Other commercial systems are also available
Open Decompression
Exsanguinate limb and elevate tourniquet
Make a longitudinal incision centered over the medial aspect of the elbow posterior to the medial epicondyle
Protect branches of medial and posterior cutaneous nerves
Expose the ulnar nerve and divide arcuate ligament (Osborne ligament)
Decompress the nerve through the two heads of the flexor carpi ulnaris (FCU) fascia
Divide the fascia proximally in similar fashion
Identify intermuscular septum; consider resection especially if anterior transposition of the ulnar nerve is planned or if impingement upon the nerve is noted
Obtain hemostasis and close skin in usual fashion
Apply well-padded bandage
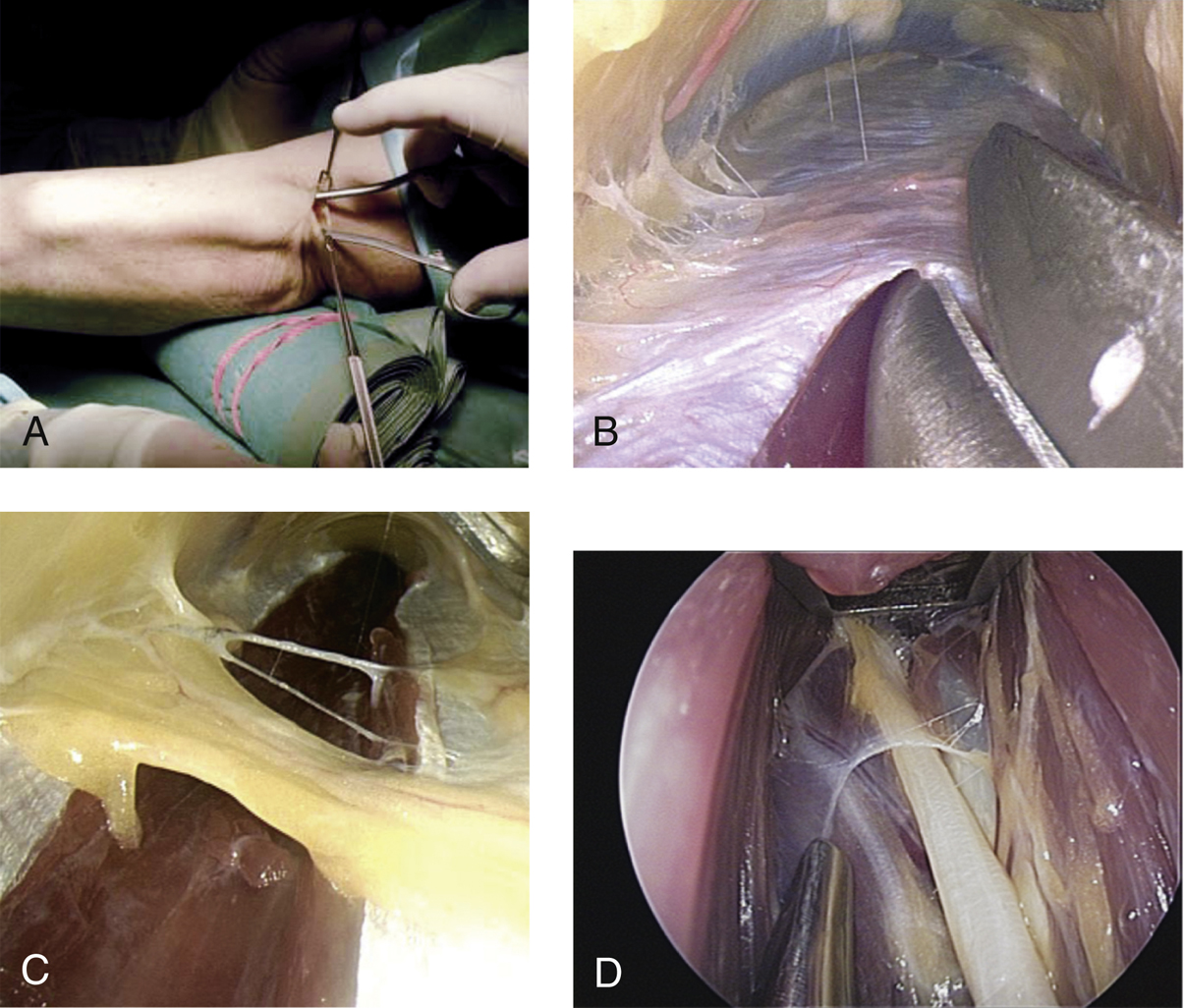
Endoscopic Decompression (Hoffmann Technique)
Raise hand table to nearly eye level of the seated surgeon
Palpate ulnar nerve
Make 1.5- to 2.5-cm longitudinal incision posterior to the medial epicondyle
Retractors facilitate exposure of the nerve; dissect adipose tissue or epitrochlear anconeus muscle as needed
Divide arcuate ligament under direct vision while keeping epifascial layer in view
Introduce tunneling forceps into space between subcutaneous tissue and fascia—not into the cubital tunnel, that is, not beneath the arcuate ligament adjacent to the nerve
Spread forceps distally, then proximally, to create workspace cavity; work gently
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree