Surgical Treatment of Ankle Fractures
Patient Selection
Ankle is most frequently injured weight-bearing joint
Injury usually results from indirect rotational forces, less commonly due to direct blow; can result in fracture and ligamentous and soft-tissue injury
Ankle stability depends on bony, ligamentous integrity; injury to both must be recognized, and treated
Classified based on anatomic site, mechanism of injury
Danis-Weber classification based on anatomic site; uses level of lateral malleolar fracture in relation to articular surface
Lauge-Hansen classification based on mechanism of injury; predicts position of foot, direction of primary deforming force based on displacement pattern, level, and morphology of fibula fracture
Individualize treatment decisions based on degree of bony, ligamentous stability, not classification system
Dislocation or subluxation of talus within ankle mortise is commonly present; even minimal mortise malalignment alters contact pressures, risks arthritis
Imperative to achieve stable, anatomically reduced mortise by restoring bony and ligamentous structures
Critical to assess the condition of the soft tissues
Marked swelling, fracture blisters, and other skin changes should delay definitive surgery until soft-tissue milieu resolves
Can wait up to 3 weeks for definitive management
Condition of soft tissues particularly important in elderly and in persons with diabetes
Most nondisplaced or minimally displaced (<2 mm) monomalleolar fractures, typically medial or lateral, are treated nonsurgically
Monomalleolar fractures displaced more than 2 mm, bimalleolar and trimalleolar fractures, fracture-dislocations, syndesmotic injuries, and open fractures require surgery
Preoperative Imaging
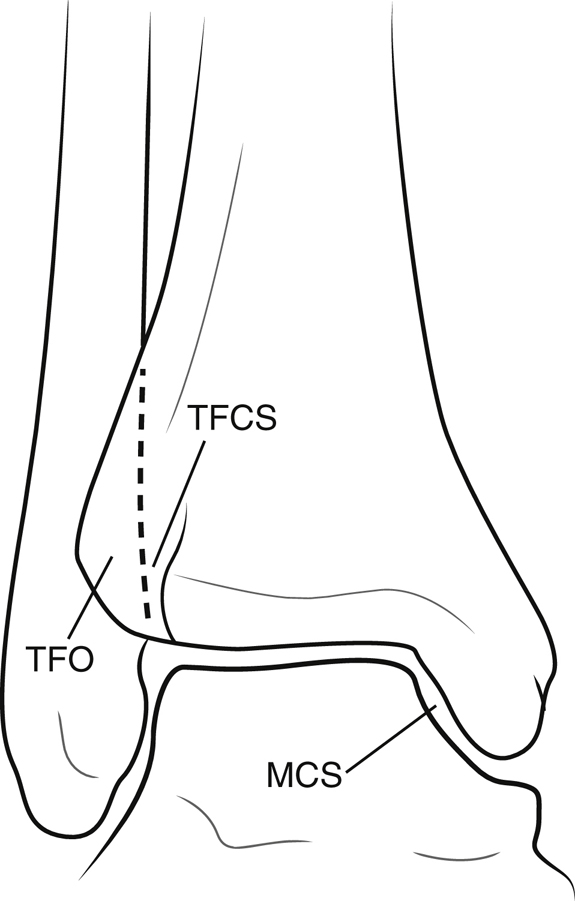
Figure 1Illustration depicts the parameters commonly measured when assessing ankle stability. The medial clear space (MCS) should be 4 mm or less on the AP and mortise views. The tibiofibular overlap (TFO) should be 6 mm or more on the AP view and 1 mm or more on the mortise view. The tibiofibular clear space (TFCS) should be 6 mm or less on AP and mortise views.
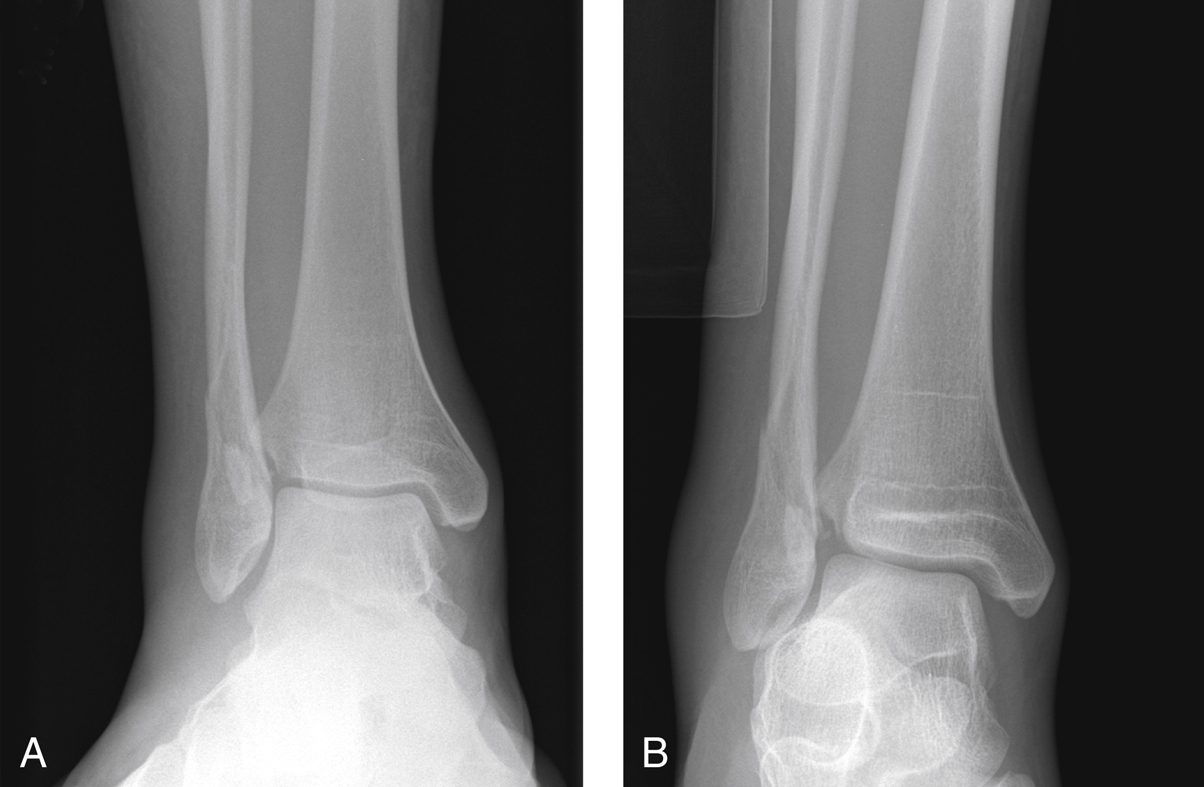
Figure 2AP radiographs show an isolated right distal fibula fracture. A, The medial clear space (MCS) appears normal on a static view. B, Note the increased MCS, suggestive of widening with gravity stress.

Figure 3AP (A) and lateral (B) radiographs show a trimalleolar ankle fracture-dislocation in a 76-year-old man. AP (C) and lateral (D) postreduction radiographs and sagittal reconstruction (E) show the posterior malleolar component. Note the now-reduced ankle mortise (C) and restoration of the tibiotalar relationship in the lateral plane (D). E, The size and displacement of the posterior malleolar fracture fragment are evident.
Ankle injuries require AP, lateral, and mortise radiographs
Three important radiographic measurements are medial clear space, tibiofibular overlap, and tibiofibular clear space (Figure 1)
Lateral shift of talus at least 2 mm (measured by medial clear space) or fracture displacement greater than 2 mm are surgical indications
Dynamic stress views can demonstrate talar shift that may be unappreciated on static radiographs (Figure 2)
Syndesmotic injury suggested by tibiofibular clear space >6 mm on AP or mortise radiographs or tibiofibular overlap <6 mm on AP and <1 mm on mortise
| Video 79.1 Trimalleolar Ankle Fracture Fixation. Eben Carroll, MD; Jason Halvorson, MD (14 min) |
Procedure
Room Setup/Patient Positioning
Surgeon, instrument table are on side of ankle injury, with C-arm on opposite side
For isolated monomalleolar and bimalleolar ankle injuries, supine position with bump under hip, nonsterile tourniquet
For trimalleolar injuries needing posterior fixation, lateral position on beanbag
Allows posterolateral approach to fibula and posterior malleolus
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


