Surgical Repair of Irreducible Congenital Dislocation of the Knee
Matthew B. Dobbs
DEFINITION
Congenital dislocation of the knee (CDK) is a rare deformity that presents at birth as recurvatum.
The incidence of CDK is estimated at 1 per 100,000 live births, which is approximately 1% of the incidence of congenital dislocation of the hip.7
It may be an isolated entity or occur with associated musculoskeletal anomalies such as dislocated hips, clubfoot, and congenital vertical talus. It can also occur with myelodysplasia, Larsen syndrome, and arthrogryposis.
ANATOMY
The fundamental pathologic feature in CDK involves the quadriceps muscle. The amount of quadriceps muscle is small, and the muscle as well as the lateral retinaculum adheres to the femur.
The quadriceps femoris tendon is shortened and fibrosed, which is thought to be secondary to the dislocation rather than its cause.3
The patella is often laterally displaced.
There is hypoplasia of the suprapatellar pouch.
The hamstrings are often deficient, subluxed anteriorly, or both.
The anterior knee articular capsule is tight.
The menisci are usually present and normal.
The pathology in the cruciate ligaments is variable, from absent to elongated.5
PATHOGENESIS
The exact cause of CDK remains unknown.
A genetic etiology is supported by the presence of familial occurrence in some cases as well as the association of CDK with developmental hip dysplasia, idiopathic clubfoot, and congenital vertical talus; all three of which have a known or presumed genetic basis.1, 11
Simple hyperextension of the knee in newborns may be caused by aberrations in intrauterine positions, such as frank breech presentation, which slowly stretches the hamstrings and posterior knee soft tissues.7, 13 Chronic knee hyperextension results in anterior subluxation of the hamstrings, allowing them to function as knee extensors.
NATURAL HISTORY
The natural history of CDK depends on the severity of the disorder on presentation. Simple hyperextension of the knee tends to resolve spontaneously or with splinting.2, 6
In cases of subluxation and dislocation, spontaneous resolution is not common, and most patients require surgical correction.
Left untreated, these patients have great difficulty with ambulation owing to the inability to flex the knees. These patients often have associated neuromuscular or genetic syndromes.3
PATIENT HISTORY AND PHYSICAL FINDINGS
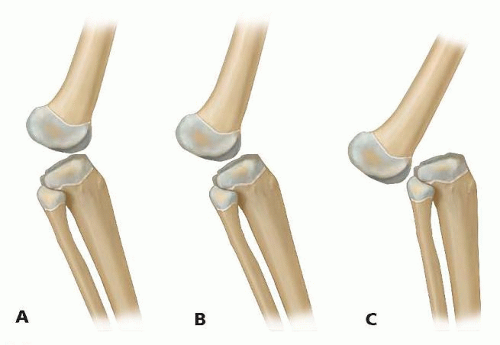
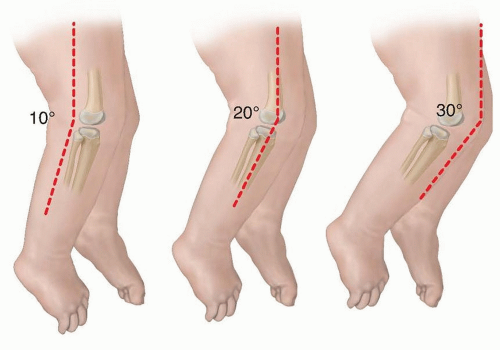
The physical findings of CDK are readily apparent at birth but of variable severity (FIG 2).

FIG 2 • This infant has a unilateral knee dislocation. Note, the deep skin creases across the front of the knee.
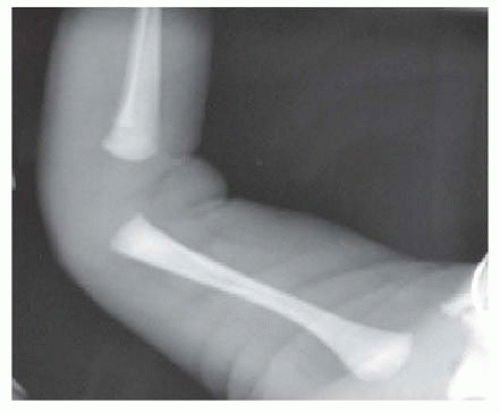
FIG 3 • A lateral radiograph of a newborn demonstrating complete dislocation of the tibia on the distal femur. The anterior aspect of the knee is on the right. Note, the deep skin creases anteriorly.
The knee is hyperextended, in severe cases to such a degree that the foot rests against the baby’s face.
In cases of simple hyperextension, the knee can be passively brought into flexion.
In the more common scenario of subluxation, passive flexion is limited but improves with splinting, casting, or both.
In cases of dislocation, the knee cannot be easily passively flexed with simple manipulation. The patella is often laterally displaced and difficult to palpate. A deep crease may be present over the anterior aspect of the knee.
The more severe cases are more likely to have associated musculoskeletal anomalies.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior and lateral radiographs of the knee help to differentiate the mild hyperextension deformity from the more severe type of subluxation or fixed anterior dislocation of the tibia on the distal femur (FIG 3).
The ossification centers of the distal femur and proximal tibia are usually present in the full-term infant.
The patella is not yet ossified in the infant.
Ultrasound can also be used to make the diagnosis.
NONOPERATIVE MANAGEMENT
Nonoperative treatment should be started as soon as possible.
Nonoperative treatment consists of serial manipulations and long-leg plaster castings.2, 4, 6, 10, 12

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree