CHAPTER 9 Surgical Pearls for Fixed-Bearing Medial Unicompartmental Knee Arthroplasty
Skin Incision
The ACL can be visualized at the time of the arthrotomy, but visualization of an intact ACL is not always required. Certainly more important appears to be the stability of the knee. An examination under anesthesia can be performed and stability of the ACL assessed. A nonfunctioning ACL with an unstable knee increases the sliding forces that can eventually lead to early polyethylene wear and joint failure. Engh and Ammeen reported on the results of unicompartmental knee arthroplasty without an intact ACL, and good results can be obtained if functional instability is not present.1 This differs from the classic article by Goodfellow and O’Connor that showed a higher failure rate without an intact ACL. Therefore, the emphasis is on knee stability, not ACL integrity.2 Visualization at the ACL does not answer completely the status of the ACL. Cushner et al. not only described significant loss of the ACL at the time of indicated total knee arthroplasty, but pathologic changes in the “viable” ACL were also noted.3 Mullaji et al. recently evaluated tibial cartilage wear in patients undergoing total knee arthroplasty and found that the articular wear pattern can provide clues to the functional status of the ACL.4 Posterior-half involvement of the medial plateau was more commonly seen when a functional ACL was not present. This is a helpful pearl since studies from Trompeter et al. showed that the clinical appearance of the ACL was not a good predictor of severity on microscopic examination.5
Certainly, the size of the incision should not compromise results. Hamilton et al. reviewed 221 unicompartmental arthroplasties performed using the MIS technique.6 This cohort was compared to a cohort of 514 standard-incision unicompartmental knee arthroplasty patients. In the MIS group, 9 of 221 were revised for loosening. Of the remaining 212 patients, 16 patients required 18 nonrevision reoperations. In other words, 25 of 221 required at least one reoperation (11.3%). This compared to 8.6% for the standard-incision group, with a higher aseptic loosening rate also noted in the MIS group (3.7% vs. 1%).
Decreasing Blood Loss
Once a skin incision is made, a surgical pearl to decrease blood loss is to inject the knee arthrotomy site with a lidocaine (Marcaine)/epinephrine solution. Thirty milliliters injected along the arthrotomy site did result in a significant decrease in blood loss in our total knee arthroplasty patients.7 While this procedure was initially described in a total knee arthroplasty patient, it could be also performed in unicompartmental arthroplasty patients. We have extended the use of lidocaine with epinephrine to all arthrotomy patients with the goal of not only less bleeding and fewer transfusions but overall less hematoma in the joint postoperatively. Our thoughts are that less blood in the joint improves the patient’s function. Periarticular steroid injections can also be used to improve outcomes following unicondylar knee replacement. Pang et al. recently performed a prospective randomized study comparing 90 knees over a 2-year period where injection with triamcinolone acetonide, bupivacaine, and epinephrine was compared to a control group in which only bupivacaine and epinephrine injections were performed. Improvement was noted in midterm and short-term results with no increase in infection or tendon failures reported.8
Solid Repair of the Arthrotomy
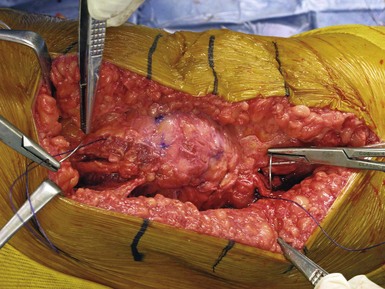
Another pearl utilized at our institution is a solid repair of the arthrotomy. If a solid repair is not performed, this can result in late patella instability and subluxation. We believe that a more watertight seal can not only improve knee appearance but also result in less wound drainage in the immediate postoperative period. We currently utilize a bidirectional barbed suture design to facilitate arthrotomy closure (Quill Suture; Angiotec, Vancouver, British Columbia). Our initial studies showed that not only did we achieve a shorter operating time secondary to a quicker closure of the arthrotomy, but a more watertight closure was also described in the laboratory setting9,10 (Fig. 9–1).
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree