Because the greater tuberosity is the insertion site of the posterior superior rotator cuff, fractures can have a substantial impact on functional outcome. Isolated fractures should not inadvertently be trivialized. Thorough patient evaluation is required to make an appropriate treatment decision. In most cases surgical management is considered when there is displacement of 5 mm or greater. Although reduction of displaced greater tuberosity fractures has traditionally been performed with open techniques, arthroscopic techniques are now available. The most reliable techniques of fixation of the greater tuberosity incorporate the rotator cuff tendon bone junction rather than direct bone-to-bone fixation.
Key points
- •
Because the greater tuberosity is the insertion site of the posterior superior rotator cuff, fractures can have a substantial impact on functional outcome.
- •
Although the greater tuberosity is commonly involved in proximal humerus fractures, isolated fractures are not and can be inadvertently trivialized.
- •
Thorough patient evaluation including adequate imaging is required to make an appropriate treatment decision.
- •
In most cases surgical management is considered when there is displacement of 5 mm or greater.
- •
Although reduction of displaced greater tuberosity fractures has traditionally been performed with open techniques, arthroscopic techniques are now available.
- •
The most reliable techniques of fixation of the greater tuberosity incorporate the rotator cuff tendon bone junction rather than direct bone-to-bone fixation.
Introduction
Although proximal humerus fractures account for approximately 5% of all fractures and many involve the tuberosities, isolated greater tuberosity fractures are less common and only account for about 2% of proximal humerus fractures. The intimate association of the rotator cuff with the tuberosities has a substantial impact on the management and outcome of these injuries. In addition, age-related factors such as activity level and bone quality play a role in the treatment of greater tuberosity fractures. The appropriate management of these fractures is predicated on having a clear understanding of the relevant anatomy, fracture characteristics, associated injuries, and patient factors. This article focuses on current principles of surgical management of isolated greater tuberosity fractures.
Anatomy
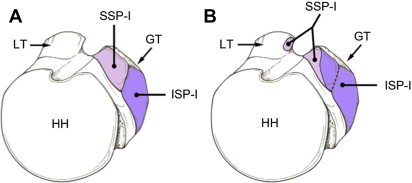
The greater tuberosity is an apophyseal structure of the proximal humerus. Ossification of the greater tuberosity occurs during the second and third years of life. On average, the superior aspect of the greater tuberosity is 6 to 8 mm inferior to the most superior aspect of the articular surface of the humeral head and is composed of 3 facets: superior, middle, and inferior. Recent anatomic studies show that the rotator cuff tendon insertions on the greater tuberosity are more complex than earlier descriptions ( Fig. 1 ). An earlier anatomic study found that the supraspinatus tendon inserts on the superior facet and the superior half of the middle facet, whereas the infraspinatus tendon inserts on the entire middle facet, covering a portion of the supraspinatus tendon. A more recent anatomic study by Mochizuki and colleagues describes a different relationship in which the supraspinatus insertion is localized to the anteromedial aspect of the highest impression of the superior facet and the infraspinatus insertion is localized to the anterolateral aspect of the highest impression of the superior facet and all of the middle facet. The soft tissue attachments of the rotator cuff affect the direction and amount of displacement of the fractured greater tuberosity. The force vectors of the supraspinatus and upper aspect of the infraspinatus result in superior displacement, whereas the lower infraspinatus and teres minor cause posterior displacement. Understanding this anatomy helps to guide both the evaluation of injuries and the operative management of displaced fractures.
The vascularity of the greater tuberosity, as well as the humeral head articular segment, derives from an anastomosis of vessels from the posterior humeral circumflex vessels and the ascending branch of the anterior humeral circumflex artery (arcuate artery), and to a lesser degree by the rotator cuff tendons and joint capsule. Hettrich and colleagues performed a quantitative assessment of the blood supply to the humeral head and found that, overall, the posterior humeral circumflex artery contributes more to the blood supply (64%) than the anterior humeral circumflex artery (36%), including the area containing the greater tuberosity. Isolated fractures of the greater tuberosity have not proved to compromise blood flow to the humeral head.
Proximal humerus fractures, including isolated greater tuberosity fractures, are commonly associated with neurologic injury. The axillary nerve, a branch of the posterior cord of the brachial plexus, passes inferior to the subscapularis muscle and through the quadrilateral space before dividing into anterior and posterior branches, which provide innervation to the deltoid and teres minor muscles respectively, as well as sensory innervation to the lateral aspect of the upper arm and shoulder. The axillary nerve is thus tethered anteriorly and posteriorly and subject to traction injury, especially with glenohumeral dislocation. The suprascapular nerve passing through suprascapular notch and around the scapular spine at the spinoglenoid notch provides innervation to the supraspinatus and infraspinatus muscles. Both of these important peripheral nerves, as well as the more proximal aspects of the brachial plexus, are susceptible to traumatic and iatrogenic injury.
Introduction
Although proximal humerus fractures account for approximately 5% of all fractures and many involve the tuberosities, isolated greater tuberosity fractures are less common and only account for about 2% of proximal humerus fractures. The intimate association of the rotator cuff with the tuberosities has a substantial impact on the management and outcome of these injuries. In addition, age-related factors such as activity level and bone quality play a role in the treatment of greater tuberosity fractures. The appropriate management of these fractures is predicated on having a clear understanding of the relevant anatomy, fracture characteristics, associated injuries, and patient factors. This article focuses on current principles of surgical management of isolated greater tuberosity fractures.
Anatomy
The greater tuberosity is an apophyseal structure of the proximal humerus. Ossification of the greater tuberosity occurs during the second and third years of life. On average, the superior aspect of the greater tuberosity is 6 to 8 mm inferior to the most superior aspect of the articular surface of the humeral head and is composed of 3 facets: superior, middle, and inferior. Recent anatomic studies show that the rotator cuff tendon insertions on the greater tuberosity are more complex than earlier descriptions ( Fig. 1 ). An earlier anatomic study found that the supraspinatus tendon inserts on the superior facet and the superior half of the middle facet, whereas the infraspinatus tendon inserts on the entire middle facet, covering a portion of the supraspinatus tendon. A more recent anatomic study by Mochizuki and colleagues describes a different relationship in which the supraspinatus insertion is localized to the anteromedial aspect of the highest impression of the superior facet and the infraspinatus insertion is localized to the anterolateral aspect of the highest impression of the superior facet and all of the middle facet. The soft tissue attachments of the rotator cuff affect the direction and amount of displacement of the fractured greater tuberosity. The force vectors of the supraspinatus and upper aspect of the infraspinatus result in superior displacement, whereas the lower infraspinatus and teres minor cause posterior displacement. Understanding this anatomy helps to guide both the evaluation of injuries and the operative management of displaced fractures.
The vascularity of the greater tuberosity, as well as the humeral head articular segment, derives from an anastomosis of vessels from the posterior humeral circumflex vessels and the ascending branch of the anterior humeral circumflex artery (arcuate artery), and to a lesser degree by the rotator cuff tendons and joint capsule. Hettrich and colleagues performed a quantitative assessment of the blood supply to the humeral head and found that, overall, the posterior humeral circumflex artery contributes more to the blood supply (64%) than the anterior humeral circumflex artery (36%), including the area containing the greater tuberosity. Isolated fractures of the greater tuberosity have not proved to compromise blood flow to the humeral head.
Proximal humerus fractures, including isolated greater tuberosity fractures, are commonly associated with neurologic injury. The axillary nerve, a branch of the posterior cord of the brachial plexus, passes inferior to the subscapularis muscle and through the quadrilateral space before dividing into anterior and posterior branches, which provide innervation to the deltoid and teres minor muscles respectively, as well as sensory innervation to the lateral aspect of the upper arm and shoulder. The axillary nerve is thus tethered anteriorly and posteriorly and subject to traction injury, especially with glenohumeral dislocation. The suprascapular nerve passing through suprascapular notch and around the scapular spine at the spinoglenoid notch provides innervation to the supraspinatus and infraspinatus muscles. Both of these important peripheral nerves, as well as the more proximal aspects of the brachial plexus, are susceptible to traumatic and iatrogenic injury.
Fracture classification
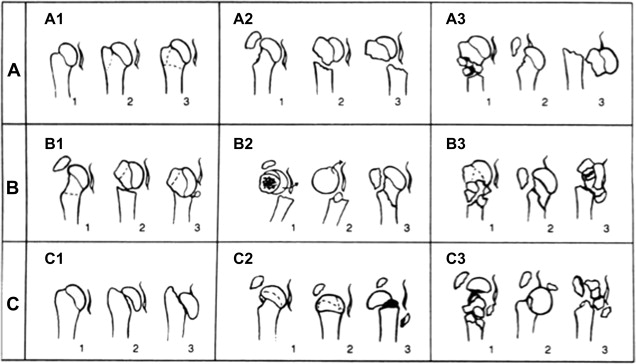
Codman’s early observation that fracture patterns involving the proximal humerus fractures often occurred along the physeal scars of the proximal humerus formed the basis for Neer’s 4-part classification system. The humeral shaft, articular segment, and the greater and lesser tuberosities comprise the 4 parts of the proximal humerus. In the original description, 1 cm of displacement of 45° of angulation were the criteria that defined a part ( Fig. 2 ). This classification system emphasized the relationship between displacement and the rotator cuff, as well as displacement and the vascularity of the humeral head articular segment, and continues to be commonly used for the description of proximal humerus fractures. The AO/ASIF/OTA classification of proximal humerus fractures is based on the relationship between fracture fragments and the humeral head articular segment ( Fig. 3 ). Type A fractures are unifocal and involve the greater tuberosity or surgical neck. Similar to many other fracture classification systems, limited interobserver reliability has been shown. Nevertheless, these classifications provide surgeons with useful information to define injuries and form the basis for treatment, with displacement as the primary indication for considering surgical intervention.
In considering displacement of greater tuberosity fractures, both degree and direction are important. Healing with superior displacement can cause subacromial impingement, whereas posterior displacement can block external rotation motion. More recent recommendations consider even a few millimeters of greater tuberosity displacement to be clinically relevant in some cases, and greater tuberosity displacement of more than 5 mm is an indication for operative treatment. Park and colleagues suggested that good results can be obtained with nonoperative treatment when the displacement is less than 5 mm. However, they also suggested that, if the displacement is more than 5 mm in young active patients, and more than 3 mm in athletes and heavy laborers with demand for overhead activity, the fracture should be repaired.
Mechanism of injury
Greater tuberosity fractures typically occur as the result of impaction, shearing, or avulsion mechanisms. Impaction fractures usually occur from a direct fall onto the shoulder or with hyperabduction and compression of the greater tuberosity against the acromion. In contrast, shearing and avulsion fractures can occur in association with glenohumeral dislocation as the tuberosity shears across the glenoid rim or with forceful contraction of the rotator cuff. In a retrospective review of 103 patients with greater tuberosity fractures, Bahrs and colleagues found that 47.6% had an impaction mechanism, 32% were associated with an indirect mechanism, and that 57% of all greater tuberosity fractures occurred as a result of glenohumeral fracture-dislocation. Previous studies showed that 15% to 30% of anterior glenohumeral dislocations are associated with greater tuberosity fractures.
Associated injuries
Rotator Cuff Tear
The status of the rotator cuff has an important impact on the functional outcome after proximal humerus facture. Although proximal humerus fractures are not usually associated with acute rotator cuff tears, preexisting rotator cuff tears and disorders are more common with advancing age. Associated acute rotator cuff tears can occur and should be considered when there is marked initial displacement, persistent displacement after reduction of an anterior glenohumeral dislocation, and when there is failure of progression of recovery after nondisplaced fracture. Although also uncommon, older patients can have preexisting chronic rotator cuff tearing. In the senior author’s experience associated acute rotator cuff tears are uncommon.
Nerve Injuries
The infraclavicular brachial plexus and peripheral nerve branches are subject to injury with proximal humerus fractures and fracture-dislocations. Nerve injuries associated with greater tuberosity fractures usually result from displacement and traction injury and can occur either from direct contact with the fracture fragments or from stretching. Isolated axillary nerve injury is the most common nerve injury associated with greater tuberosity fracture-dislocations.
Anterior dislocations are a common cause of isolated axillary nerve and posterior cord lesions. When diagnosed by electromyography, the prevalence of axillary and other nerve lesions associated with glenohumeral dislocations and humeral neck fractures is 20% to 30%. In patients older than 40 years, it can be as high as 50%.
Nerve injuries are often missed or overlooked in the acute setting because pain and immobilization can make examination difficult. Sensory deficit is especially difficult to assess and does not always accompany an axillary nerve lesion. However, recovery of nerve injuries associated with proximal humerus fractures is often incomplete. Alnot reported that 80% of isolated axillary nerve lesions were neurapraxias that recovered in 4 to 6 months. Although persistent complete deltoid palsy is rare, a long delay before reinnervation lessens the likelihood of complete functional recovery.
Vascular Injuries
Although vascular injuries are rarely associated with proximal humeral fractures, the consequences of a missed injury are severe, thus highlighting the importance of early evaluation of the vascular status of the upper extremity. Axillary artery injury has been reported in approximately 5% of 4-part proximal humeral fractures. Swelling and the collateral circulation may mask the extent of the vascular injury. Even in the presence of a complete axillary artery occlusion, the radial pulse may be palpable because of the extensive collateral circulation around the shoulder. The peripheral pulses, including the radial artery, should be palpated in addition to seeking other signs of vascular injury such as paresthesias, pallor or cyanosis, and an expanding hematoma. If a vascular injury is suspected, Doppler ultrasonography and arteriography should be performed and appropriate management emergently instituted in the case of significant arterial injury.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




