Surgical Management of Fractures of the Talus
Introduction
Anatomy
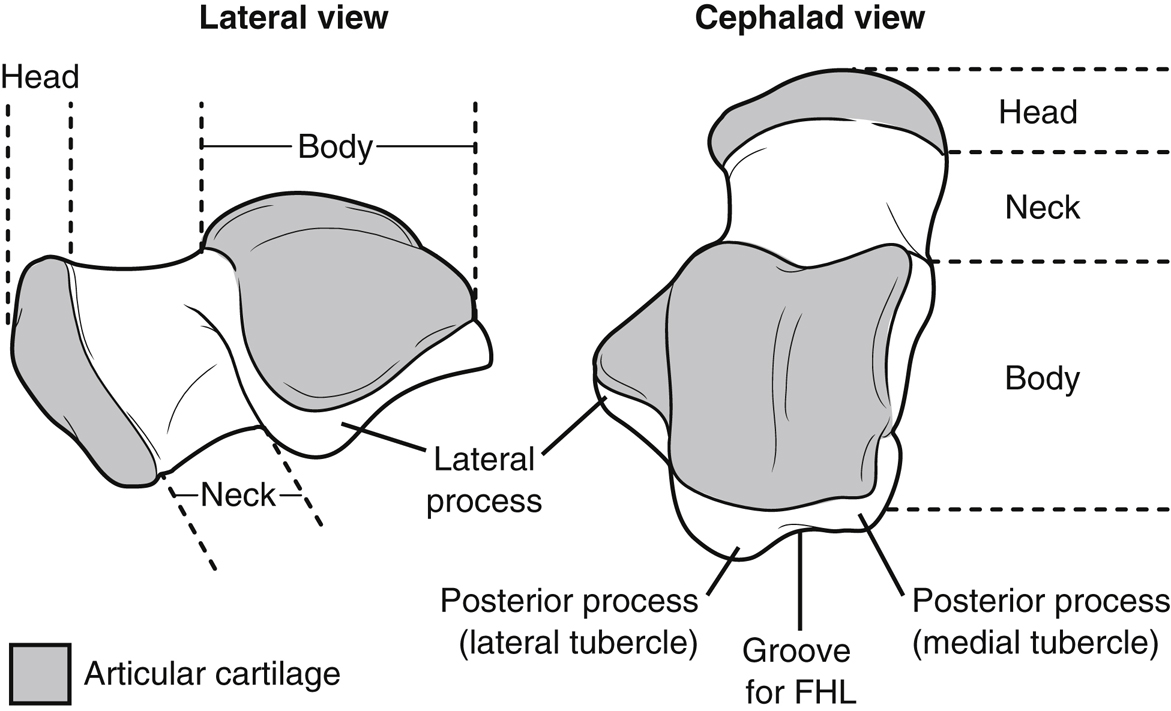
Figure 1Illustrations depict two views of the talus. FHL = flexor hallucis longus
(Adapted from Fortin P, Balazsy J : Talus fractures: Evaluation and treatment. J Am Acad Orthop Surg2001;9[6]:114-127.)
Talus consists of the head, neck, body, lateral process, and posterior process (Figure 1)
Flexor hallucis longus (FHL) tendon divides posterior process into medial and lateral tubercle
Cartilage covers 60% of talus
No muscles/tendons attach to talus, which plays critical role in midfoot, hindfoot, and ankle motion
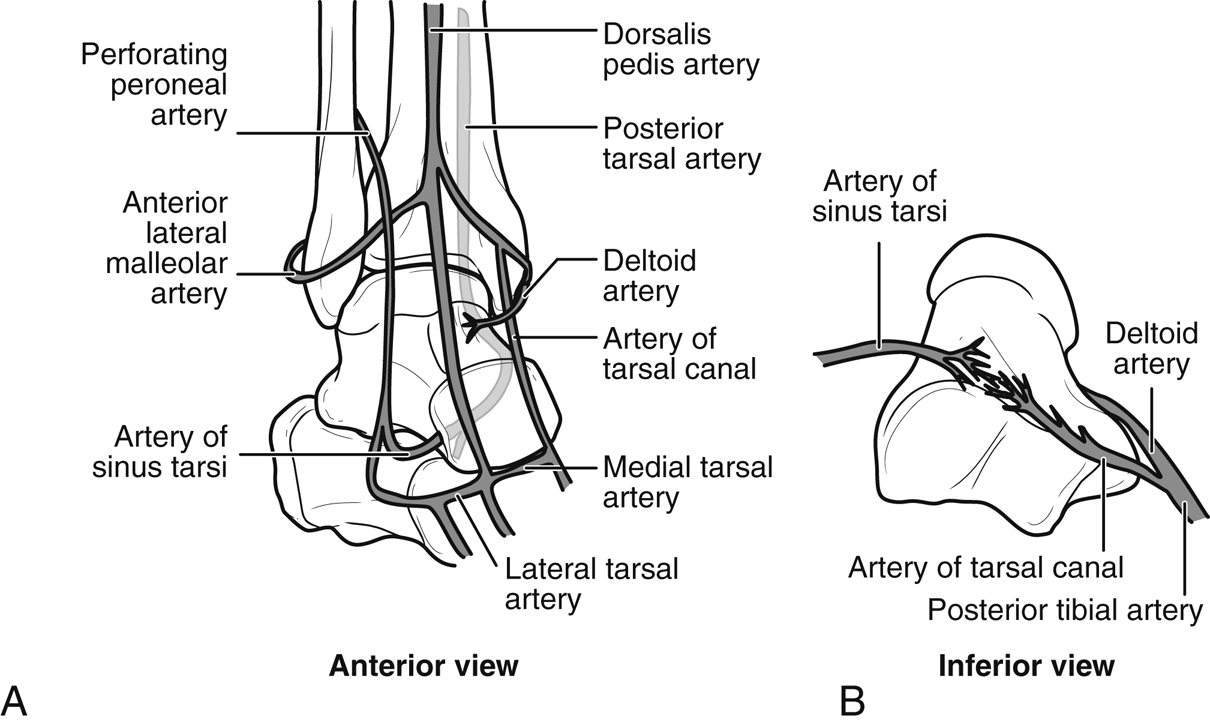
Talus receives blood supply from artery of tarsal canal, deltoid artery, and artery of sinus tarsi; all derive locally from peroneal, anterior tibial, and posterior tibial arteries (Figure 2)
Mechanism of Injury
Talar neck fractures commonly occur from hyperdorsiflexion force
Talar neck susceptible to fractures due to its low bone density and small cross-sectional area, as talus strikes denser anterior tibia
High-energy injuries with significant comminution and displacement; high incidence of associated fractures (64%) and soft-tissue injuries (21% open)
Classification
Hawkins classification widely used
Type I—Nondisplaced
Type II—Displaced with subluxation/dislocation of subtalar joint
Type III—Displaced with subluxation/dislocation of subtalar and tibiotalar joints
Type IV—Displaced with subluxation/dislocation of subtalar, tibiotalar, and talonavicular joints
Rate of talar body osteonecrosis correlates with Hawkins classification, increasing risk of vascular disruption with extent of displacement
Hawkins classification confined to talar neck; AO/Orthopaedic Trauma Association classification more broad but rarely used clinically
Patient Selection
Indications
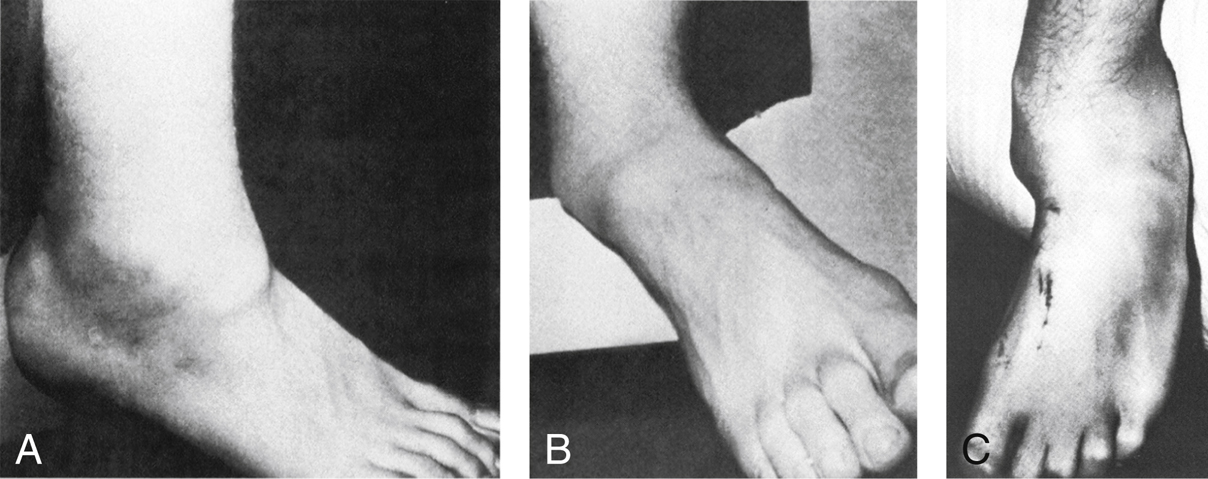
Figure 3Photographs depict deformity associated with the dislocation of the subtalar joint. In this medial subtalar dislocation, the head of the talus is palpable on the dorsum of the foot (A), and the heel is displaced medially (B). C, In this lateral subtalar dislocation, the head of the talus is prominent medially, whereas the rest of the foot is dislocated laterally.
(Reproduced with permission from Buckingham WW Jr, LeFlore I : Subtalar dislocation of the foot. J Trauma1973;13[9]:753-765.)
Truly nondisplaced fractures can be managed nonsurgically
Displaced fractures require surgical management (Figure 3)
Contraindications
Preexisting active or indolent bone infection, severe neuropathic foot, uncorrectable vascular impairment with likelihood of wound healing complications
Isolated nondisplaced lateral or posterior process fractures may be managed nonsurgically
Preoperative Imaging
Plain Radiography
AP, lateral, ankle mortise, and Canale views of ankle and foot
Lateral view shows talar neck and talonavicular, tibiotalar, talocalcaneal joint incongruencies
Canale view shows neck in profile; obtain with foot in maximal plantar flexion, 15° internal rotation, with beam angled 75° from horizontal
CT
Axial CT with sagittal and coronal reformats are recommended
Aids preoperative planning, characterizing extent of comminution and displacement
Procedure
Patient Positioning
Supine position with feet at end of radiolucent table for talar head, neck, and most body fractures
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


