Surgical Fixation of Fractures of the Distal Femur
Introduction
Fixation of distal femoral metaphyseal fractures is challenging; demands anatomic axial alignment, precise reduction of articular surface
Distal femur is defined by a square; sides same length as widest part of distal femoral epiphysis (metaphysis in adults)
A fracture whose center resides within this box is defined as a distal femoral fracture
Intra-articular fractures classified as partial or complete articular
Factors making treatment difficult
High-energy distal femur fractures have soft-tissue stripping; 50% of intra-articular fractures are open; tendinous structures at distal end lead to poor environment for bone healing due to lack of extraosseous vascularity
High-energy fracture patterns result in articular, metaphyseal fragmentation, making reduction difficult; risk of posttraumatic arthritis; metaphyseal fragmentation contributes to delayed union, nonunion
Increasing incidence of osteoporosis makes these fractures more prevalent; periprosthetic fractures make management difficult
Patient Selection
Indications
Any displaced intra-articular fracture in healthy, active, ambulatory patient
Most displaced extra-articular fractures need surgery because long-term knee function needs alignment of distal femur
Contraindications
Nondisplaced articular or metaphyseal fracture in healthy patient who mobilizes with cast
Individuals who are unfit for surgery, nonambulatory, significantly incapacitated
Consider total knee arthroplasty in elderly patients with multifragmented articular fracture
Preoperative Imaging
Radiography
AP, lateral of knee, femoral shaft; full-length femur
If fracture significantly displaced, gentle traction may improve radiographs
Must determine if fracture involves articular surface; rule out coronal plane fracture of medial/lateral condyle (Hoffa fracture) on lateral radiograph
Computed Tomography
Indicated to evaluate intra-articular fracture pattern if present
Procedure
Timing
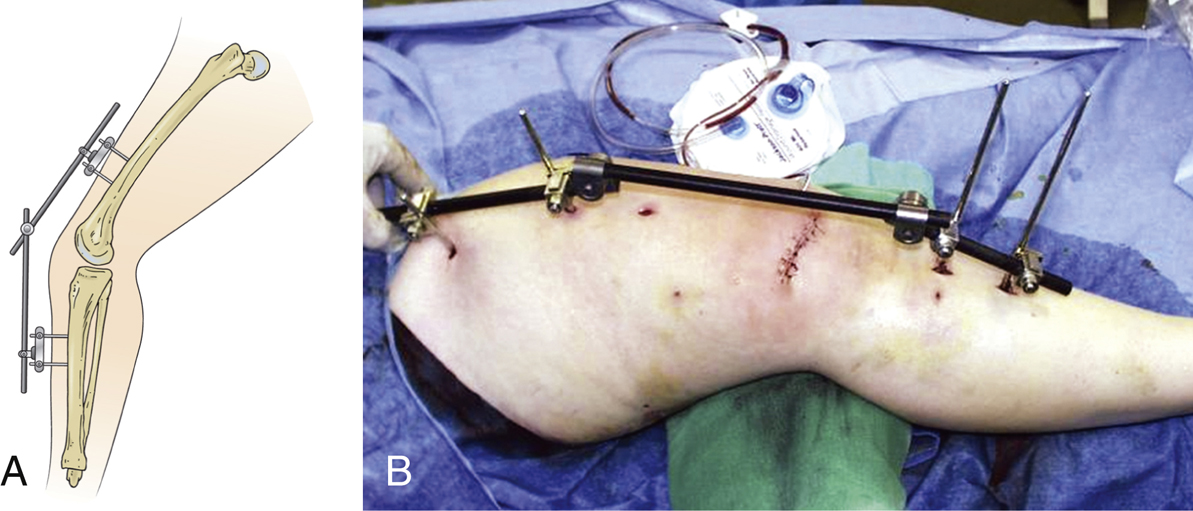
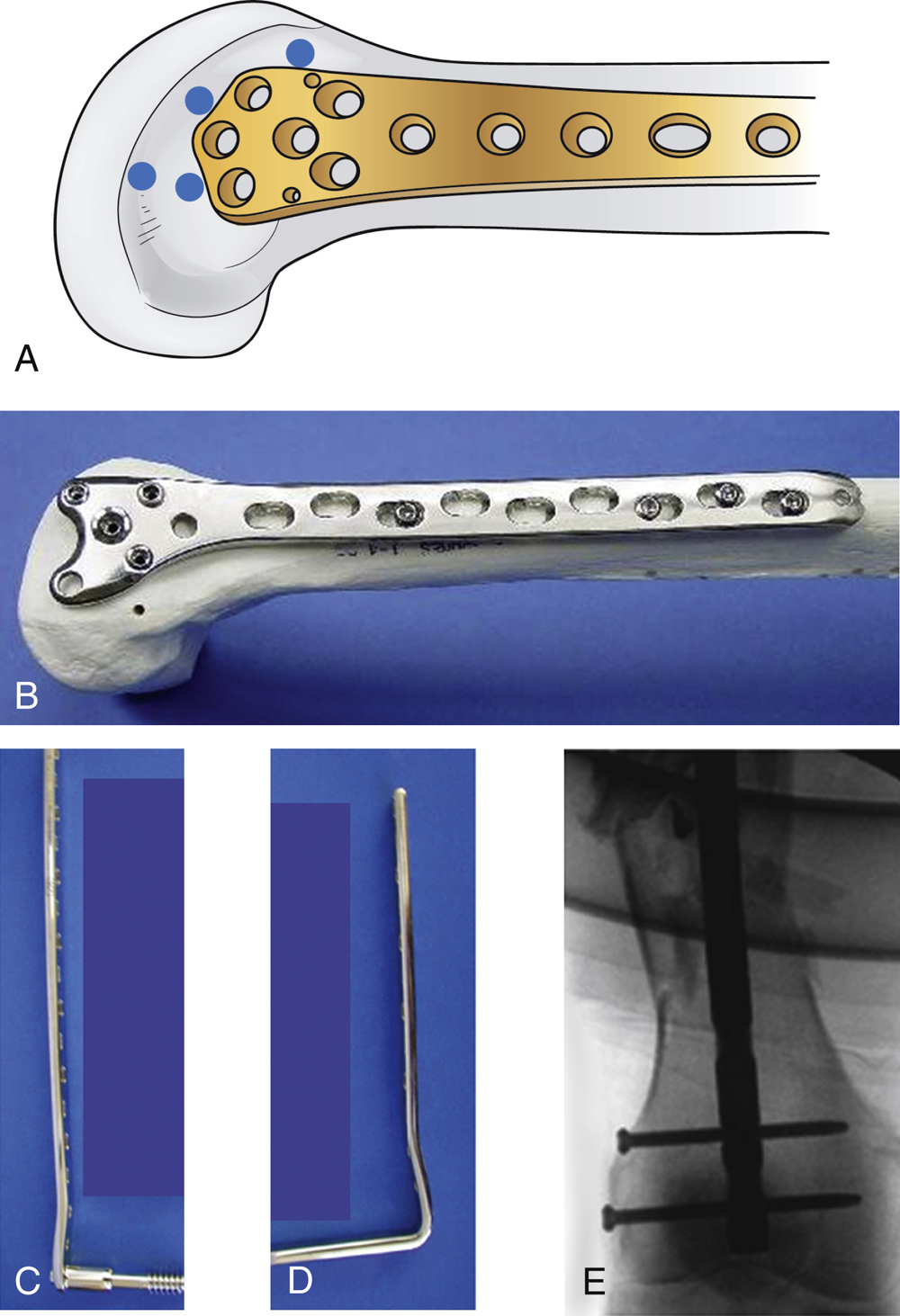
Figure 1 A, The illustration of the lateral aspect of the leg shows the joint-spanning external fixator. B, Intraoperative photograph demonstrates that it is imperative that the Schanz screws are placed outside of the proposed area for the surgical incisions for the fixation.
(Courtesy of AO Archives and AO Principles of Operative Management of Fractures.)
Authors recommend fixation as soon as possible when patient medically stable, appropriate staff available, and nature of injury understood
If staff unavailable and conditions not met, consider joint-bridging external fixation to align fracture and stabilize soft tissues
For open fractures, severe soft-tissue injury, consider joint-spanning external fixator so soft tissues can “declare” their intent (Figure 1)
Room Setup/Patient Positioning
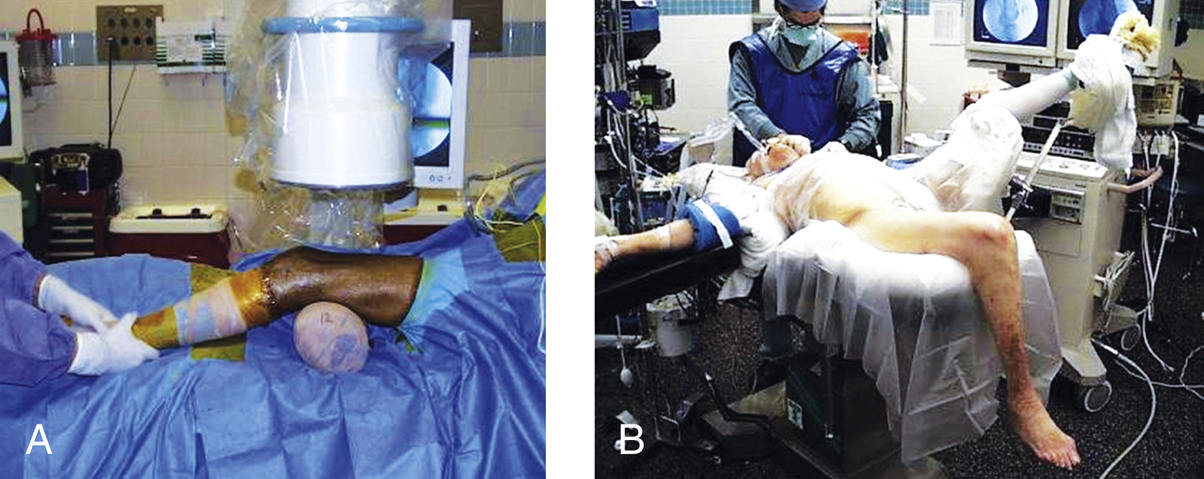
Figure 2 A, Intraoperative photograph of the lateral aspect of the leg shows the patient positioned on radiolucent table with C-arm from the side opposite the fractured limb. Note the roll under the thigh providing a force for indirect reduction along with manual traction. B, Intraoperative photograph of the AP aspect of the patient positioned on a regular operating table with the end flexed so as to allow access to the knee.
(A, Courtesy of Steve Sims, MD, Charlotte, NC. B, Courtesy of Eric Johnson, MD, Los Angeles, CA.)
Radiolucent table
Place fluoroscopy opposite the injured leg; surgical team on side of injury
Supine position; place sterile triangle or bump proximal to fracture to allow knee flexion up to 60° (Figure 2, A); also can place knee at table break to allow flexion as desired (Figure 2, B)
Placing knee at table break reduces pull of gastrocnemius and abductor magnus, preventing genu recurvatum, shortening
If using roll under buttock, take care to avoid malrotation of the fracture
Special Instruments/Equipment/Implants
Periarticular reduction clamps
Foot plates (for weak osteoporotic bone)
Wide-throated clamps
Kirschner wires (K-wires), used as joysticks
Cancellous or cortical screws, sizes 2.7 to 6.5 mm; trend toward 3.5-/4.0-mm screws, which increase space for distal plate screw placement, provide good fixation
Locking femoral condylar plate
Locking screws enhance angular stability of metaphyseal component
Shaft holes have locking or combination holes, enable axial compression with nonlocking cortical screws (Figure 3, A and B)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree