Introduction
Wrist surgery is characterized by the multiplicity of surgical approaches and the difficulty in exposing the carpal bones, which require the surgeon to determine the most appropriate technique. Schematically, the anatomical elements that prevent access to the carpus are: on the dorsal side, the extensor tendons of the wrist and fingers, sensory nerves, and dorsal veins; at the front, both median and ulnar nerves, each crossing a tunnel, the flexor tendons of the wrist and fingers through the carpal tunnel with the median nerve, and the radial and ulnar arteries.1,2
The patient is positioned supine; the upper limb rests on a table with a tourniquet just below the axilla, which for anterior approaches is in supination and for posterior approaches is in pronation, with the shoulder well relaxed.
The carpal bones (except the pisiform), the intracarpal ligaments, and the distal radioulnar joint will be exposed by posterior approaches; the distal radius and scaphoid, as appropriate, by anterior, posterior, or lateral approaches; and all tendons, vascular bundles, or nerves by direct approaches.
3.2 Principles
For better healing and better exposure, incisions parallel to the axis of the upper limb are favored because they respect more proximodistal vascularization. To avoid scar retraction, especially in anterior approaches, do not cross the flexor creases (e.g., discontinuity at the anterior flexion crease of the wrist); avoid skin detachment, especially on the dorsum of the wrist surface, to respect the vascularization of muscles and intermuscular septa,3 especially in patients with fragile skin (rheumatoid arthritis, corticosteroids). If detachment is necessary, make contact with the extensor retinaculum and lift the skin with the nerves (radial and/or ulnar). Respect the branches of the radial nerve radially (dorsoradial approach), and of the ulnar nerve ulnarly (dorsoulnar approach), which are vulnerable.
Until now, surgical approaches to the wrist joint have been focused on providing large exposure of the carpus. Recent investigations of the innervation and proprioception of the wrist joint show that one should also take care to preserve the innervation of the capsule and ligaments. Some authors propose surgical approaches to the dorsal and volar radiocarpal joint aiming to minimize damage to the innervation of the capsule while providing wide access to the wrist.4
3.2.1 Anterior Approaches
From the lateral to the medial side of the wrist, these approaches allow exposure of the scaphoid and trapezium (anterolateral approach), the lunate in the carpal tunnel (anterior approach), and the pisiform bone (anteromedial approach). These approaches may pose danger to the subcutaneous sensory branches: palmar cutaneous branches of the median and ulnar nerves at the wrist level, the superficial vascular arch to the distal edge of the flexor retinaculum.
Scaphoid and Trapezium Approaches: Anterolateral Approach
Scaphoid Approach
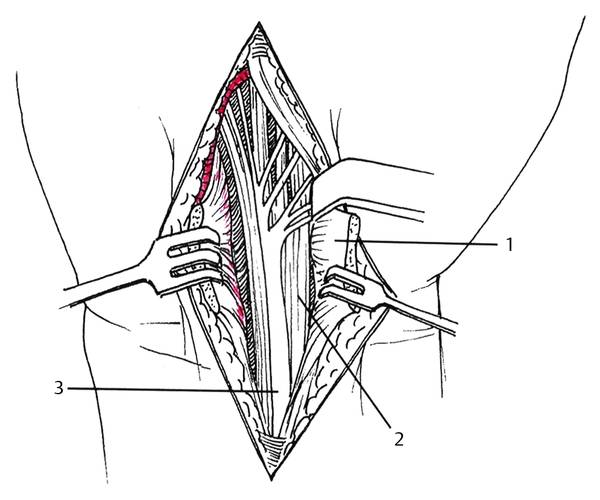
A longitudinal skin incision is made, starting 3 or 4 cm upstream from the distal anterior crease of the wrist, radially or over the flexor carpi radialis (FCR) tendon. Changing direction at the level of the distal flexion crease of the wrist, the incision continues over the relief of the thenar muscles about 1 to 2 cm (bayonet or zigzag approach) up to the distal tubercle of the scaphoid. The deep fascia is incised longitudinally at the radial edge of the FCR, which is then retracted ulnarward with the flexor tendons. Care is taken to avoid the palmar cutaneous branch of the median nerve, which is ulnar to the FCR. The radial artery and the sensory branches of the radial nerve are gently retracted radially (▶ Fig. 3.1). This exposes the flexor pollicis longus (FPL) tendon which is also retracted radially.
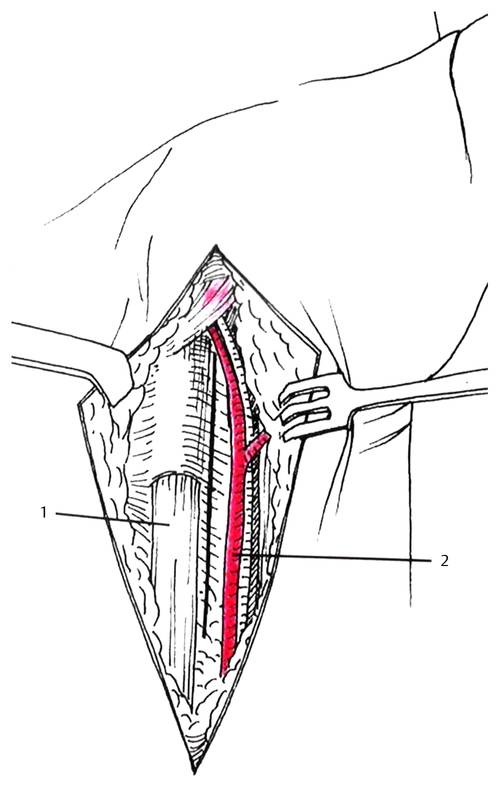
Fig. 3.1 Incision of the antebrachial fascia between (1) the flexor carpi radialis and (2) the radial artery. (With permission of Elsevier-Masson. Dubrana F, Le Nen D. Manuel des voies d’abord en chirurgie orthopédique et traumatologique. Ed Masson. Paris, 2003.)
Exposure of the distal radius The pronator quadratus muscle is elevated from its radial attachment. The FPL is also elevated from its radial attachment. This gives complete exposure of the distal radius. The brachioradialis muscle can also be elevated subperiostally to improve the exposition.
Exposure of the scaphoid The superficial branch of the radial artery is retracted (if large) or ligated. The capsule is exposed distally to the pronator quadratus and opened vertically in the plane of the skin incision (with the radioscaphocapitate ligament, which will be repaired after surgery) until contact is made with the bone (▶ Fig. 3.2). To preserve the innervation of the capsule and ligament, some authors recommend a nerve-sparing capsule approach4 in which two flaps are raised: laterally a flap based proximally and involving the radioscaphoid ligament; medially a flap based distally and involving the radioscaphocapitate ligament.
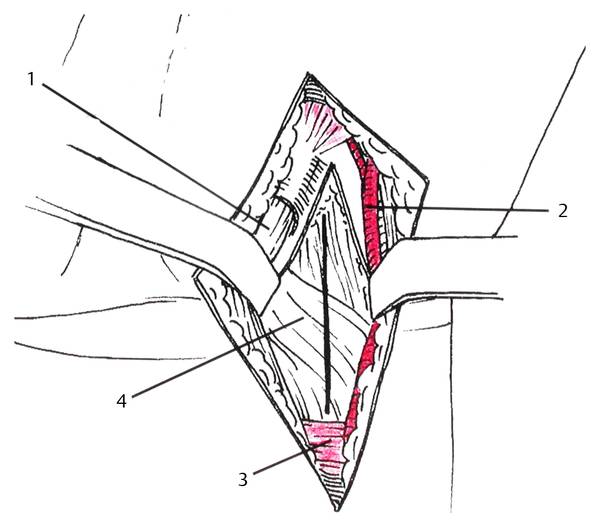
Fig. 3.2 Longitudinal capsulotomy allowing scaphoid exposure: (1) flexor carpi radialis; (2) radial artery; (3) pronatus quadratus; (4) capsule. (With permission of Elsevier-Masson. Dubrana F, Le Nen D. Manuel des voies d’abord en chirurgie orthopédique et traumatologique. Ed Masson. Paris, 2003.)
Variant To avoid injury to the radial bundle, it is better, after skin incision, to open the sheath of the FCR and to approach the capsule or distal radius through the deep surface of the same sheath after having retracted medially the flexor tendons.
Indications
Fracture of the distal radius (volar locking plate)
Osteotomy of the distal radius (malunion, Kienböck disease)
Scaphoid fixation and grafting (vascularized or non-vascularized)
Ganglion cysts of the pulse gutter
Total denervation of the wrist (one of the surgical steps)
Trapezium Approach
The skin incision is made first longitudinal along the lateral edge of the first metacarpal bone on its proximal two-thirds, then it bends to the distal flexion crease of the wrist until the lateral side of the FCR. Small subcutaneous sensitive branches of the radial nerve are exposed and protected; small veins are coagulated. One should systematically identify the dorsal lateral collateral nerve of the thumb to avoid injury. A deep incision is made along the lateral side of the first metacarpal bone and extended upward through the abductor pollicis longus. After elevation of the abductor pollicis brevis close to the bone, a longitudinal incision of the capsule exposes the base of the metacarpal bone, the trapezometacarpal (TM) joint, and the trapezium. When closing, the abductor pollicis brevis is repositioned and the abductor pollicis longus is sutured. Extension downward allows metacarpophalangeal joint surgery; extension upward along the flexor carpi radialis is for treating tenosynovitis of the FCR.
Indications
Partial or total trapezectomy, with or without implant, with or without ligamentoplasty
Total trapezometacarpal replacement
Factures of the trapezium or at the base of the first metacarpal bone
Lunate Approach: Midline Approach of the Carpal Tunnel
The skin incision is longitudinal and begins, according to the exposure required, 2 to 4 cm above the distal flexion crease of the wrist, over the palmaris longus. At the height of this crease, the incision is slightly unhooked ulnarward to avoid injury to the palmar cutaneous branch of the median nerve; it then follows close to the palm thenar crease, always remaining inward a few millimeters so as not to injure this cutaneous branch. The deep fascia is incised carefully, slightly medial to the palmaris longus, to just below the median nerve. The flexor retinaculum is incised on the ulnar side of the skin approach. At the bottom of the incision, the superficial palmar arch must be respected; this appears as a bluish structure. After opening of the retinaculum, all flexor tendons surrounded by their synovial sheath and the median nerve are exposed (▶ Fig. 3.3). This classic approach can be enlarged, either upward to the forearm to expose the radius, to release the median nerve, or to explore the flexor tendons; or downward, continuing the incision to the palm and extending therefrom by transverse approach, slightly upstream or downstream of the distal palmar crease, or a digitopalmar zigzag incision. With reflection of the flexor tendons toward the last four fingers (never dissect the median nerve, so as to avoid injury to the nerve itself or to the thenar motor branch, or adhesions), the floor of the carpal tunnel appears. Capsulotomy in front of the carpus, longitudinal or in the form of a quadrangular flap, exposes the lunate or scaphoid tubercle.