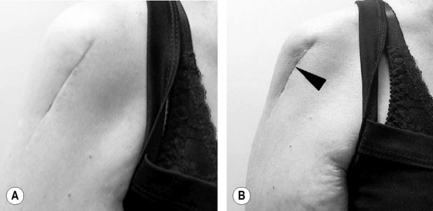
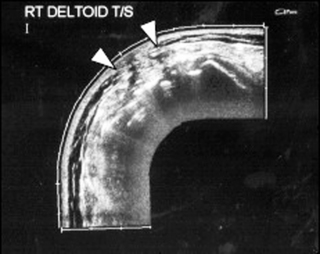
7.17 Surgery and scarring For open wounds (including surgery) and severe internal tears (ruptured tendon or ligament) wound closure and tissue strength are critical and a certain amount of scarring is necessary and inevitable. Scars differentiate and attempt to become quasi-tissue specific in response to internal and external influences. Filling defects in loose, flexible tissue, scar tissue will change to duplicate the same tissue characteristics as far as possible in the final stages of healing. Impaired mobility of soft tissues can contribute to chronic pain and tissue stiffness as well as abnormal movement patterns within the musculoskeletal system (Bouffard et al. 2008). Successful healing does not automatically correlate with return to full function. If, for example, a repaired tendon develops normal tensile strength but does not glide, it is a functional failure. Postsurgical adhesions result from injured tissues (following incision, cauterization, suturing or other means of trauma) fusing together to create abnormal connections between two normally separate surfaces of the body (Ergul & Korukluoglu 2008). Outcomes differ depending on the injured tissue, type of injury, genetic factors, and the presence of systemic disease. Alterations in the normal healing response could be associated with severe after-effects, either as a failure to heal (wound failure), or excessive repair including hypertrophic scarring, keloids, contracture, and adhesions (Occleston et al. 2008). For most patients, adhesions have little effect, while others may develop considerable clinical consequences, for example: • After laparotomy, almost 95% of patients are shown to have adhesions at later surgery (Ellis et al. 1999). Intestinal obstruction, chronic abdominal and pelvic pain, female infertility and difficult reoperation with bigger risk are also reported (Ergul & Korukluoglu 2008; Salim et al. 2008). • Even minimally invasive surgical procedures (e.g., arthroscopy) are reported as contributing to increased risk in developing knee osteoarthritis (Ogilvie-Harris & Choi 2000). This can be associated with surgical difficulties and postoperative complications in primary total knee arthroplasty (Piedade et al. 2009). • Previous abdominal surgery has been shown to be a factor in low backache, myofascial pain syndromes (Lewit & Olsanska 2004), and in compromised vascular anatomy of the abdominal wall (Rozen et al. in press). • Adhesions, tissue fibrosis and loss of tissue glide between structures can be identified as the source of pain and restriction of movement and function in up to 72% of patients after surgery for breast cancer (Lee et al. 2009). Fascia plays an important role in the body’s musculoskeletal dynamics (Stecco & Stecco 2009). This includes tension transfer across the epimysium (the fibrous envelope surrounding a muscle), and between muscles (Huijing 2007). It further contributes to the development of muscle force (Aspden 1990) and functions as a responsive, dynamic and complex mechanosensitive system for coordinated movement (Schleip et al. 2006). Fascia controls the quality of movement while keeping the bony levers and spacers within a specific functional configuration. The body is arranged in several layers, from superficial to deep (Stecco & Stecco 2009): • The skin is formed by the epidermis and dermis. • The superficial fascia consists of two or more adipose, loose connective tissue layers separated by a membranous layer(s) of collagen and elastic fibres. • The deep fascia envelops the large muscles of the trunk and forms fascial sleeves in the limbs. • The epimysial fascia lies beneath the deep fascia of the limbs. This interface consists of three distinct layers: the deep fascia, the fibrous envelope of the muscle (epimysium) and a loose areolar tissue layer between the deep fascia and epimysium (McCombe et al. 2001). The deep fascia of the trunk is often fused with and becomes the epimysial fascia for the muscles. The superficial fascia allows muscles to slide beneath the skin as they contract, while the deep fascia synchronises motor activity in order to produce smooth, resistance-free economical movements (Stecco & Stecco 2009). The body’s response to injury, either surgically or traumatically induced, is immediate. It signals repair to begin. Three dominant phases can be described: the inflammatory phase preparing the area for healing, the fibroplastic phase rebuilding the structure, and the remodeling phase providing the final form. One process is stimulated to begin, and its completion, in turn, signals another cellular response until the wound is bridged by scar. Different tissues heal at different rates. One wound can show various areas in different stages of healing. All surgery carries a risk of adhesions between tissues resulting in dysfunction in the form of restricted tissue glide, muscle imbalances, weakness, or loss of flexibility (Fig. 7.17.1). Disturbed patterns may even become evident some distance from the scar. Inflammation is crucial to the healing response. It continues throughout all healing phases, stimulating and coordinating the functions of wound repair. Inflammatory mediators regulate all aspects of tissue healing and remodeling, whether planned (as in development) or unplanned (as in tissue repair after injury). One mediator, the cytokine transforming growth factor beta 1 (TGF-β1), is unique in its widespread actions; from enhancing the deposition of extracellular matrix to acting as a potent regulator of repair by coordinating or suppressing the actions of other growth factors, cytokines and mediators (Henry & Garner 2003). The connective tissue response to the internal (inflammatory mediators and growth factors) and external (motion and directional strain) stresses applied will determine how the scar matures. Thus the scar can become either dense and unyielding (Fig. 7.17.2) or pliable and mobile. Remodeling is not restricted to the injured area only. Neighboring, noninjured tissue also changes its collagen production rate in response to inflammation. Every normal movement is accompanied by stretching, gliding and/or shifting within the surrounding soft tissue. Compromised soft tissue mobility may therefore impair motor function. Distortion of surrounding myofascial relationships can alter synergistic and antagonistic muscle balances and proprioception (Stecco & Stecco 2009). Adaptive patterns to complete or execute a movement and straining to overcome tissue resistance to produce movement are energy expensive and run the risk of producing further tissue damage (Manheim 2001). The ultimate outcome could be global dysfunction. Damaged tissues and structures need repair before the system can function efficiently again. The treatment and management of surgical scarring falls into two main categories:
Introduction
The extent of the problem
Understand fascial relationships
Anatomy of tissue layers
 In the trunk, the deep fascia is subdivided into three laminae. Each lamina is, in turn, bilaminated to accommodate superficial, intermediate or deep muscles in the trunk and neck. Thin layers of loose adipose tissue separate the various fascial laminae, allowing gliding between layers.
In the trunk, the deep fascia is subdivided into three laminae. Each lamina is, in turn, bilaminated to accommodate superficial, intermediate or deep muscles in the trunk and neck. Thin layers of loose adipose tissue separate the various fascial laminae, allowing gliding between layers.
Surgery
Treatment
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Musculoskeletal Key
Fastest Musculoskeletal Insight Engine