Hammertoe Surgery
Arthroplasty, Arthrodesis or Plantar Plate Repair?
Keywords
• Hammertoe deformity • Conservative care • Surgical management
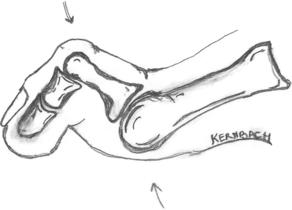
Hammertoe deformity is defined as dorsiflexion of the proximal phalanx on the metatarsal head at the metatarsal phalangeal joint (MTPJ), and plantarflexion of the intermediate phalanx on the proximal phalanx at the proximal interphalangeal joint (PIPJ).1 The distal interphalangeal joint (DIPJ) may be dorsiflexed, plantarflexed, or in a neutral position (Fig. 1).2 Contracture of the involved joints can be rigid, semirigid, or flexible. In severe instances of hammertoe deformity, dislocation or subluxation of the MTPJ can occur and this can further exacerbate the condition by placing retrograde pressure onto the plantar MTPJ, thereby causing further attenuation of the plantar plate with a distal migration of the plantar fat pad in a vicious circle (Fig. 2).
Painful hammertoe deformity and lesser MTPJ pain are commonplace in a foot specialist’s clinical practice. These complaints are frequently interrelated and exist concomitantly with first ray hypermobility, metarsus primus elevatus, metatarsus primus varus, metatarsal parabola abnormalities (with a negative first metatarsal protrusion distance), hallux abductovalus, gastrocnemius equinus, and obesity-driven forefoot overload syndrome.3 Hyperkeratotic lesions are often present on the dorsal apex of the hammertoe deformity, distal toe tip, and/or at the plantar MTPJ. Onychodystrophy may develop due to repetitive micro-trauma on the nail matrix secondary to the hammertoe contracture deformity. A modified Lachman test, also called a dorsal drawer test, should be used to evaluate for the presence of MTPJ predislocation syndrome.4 A comprehensive physical examination should also include an evaluation of all painful regions, hammertoe flexibility, first ray hypermobility, the Silfverskiold test for gastrocnemius equinus, and any open and closed kinetic chain differences in the reduction of deformity.3,5,6 Special care should be taken to differentiate the diagnosis of neuroma from the more common diagnosis of mechanically-induced MTPJ predislocation syndrome.
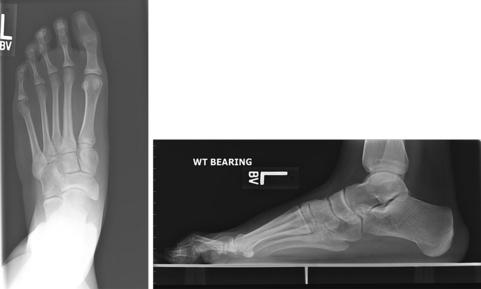
Trauma, neuromuscular disorders, and inflammatory arthropathies such as rheumatoid or psoriatic arthritis can further exacerbate the hammertoe condition. These etiologies should be considered in the workup with a comprehensive history, review of systems, physical examination, and imaging. Diagnostic imaging should include weight-bearing dorsoplantar, plantar-axial, and lateral plain film radiographs, which may elucidate early lesser MTPJ subluxation/dislocation and first ray insufficiency. Arthrography of the symptomatic MTPJ and/or magnetic resonance imaging (MRI) should be considered in cases where acute plantar plate rupture or attenuation is suspected.5,7 Blitz and colleagues7 identified anatomic variances in second MTPJ arthrography and suggested that arthrography be performed under fluoroscopic guidance and correlated with the clinical scenario. If the contralateral foot is asymptomatic, consideration should be given for its use as an arthrography comparison control with an identical injection technique.
Conservative care for chronic hammertoe deformity with associated lesser MTPJ pain includes padding, arch supports with associated top cover modifications, a rigid rocker-soled extra-depth shoe or walking boot, nonsteroidal antiinflammatory drugs, and weight loss when indicated. Padding options may include crest-buttress pads, tube foam, lamb’s wool, and/or silicon gel pads. Strict avoidance of barefoot walking, especially on hard surfaces, and placement of rugs in high traffic areas where barefoot walking or standing occurs can also help to improve the symptoms of lesser MTPJ pain. A Budin splint or Gerard Yu figure-of-eight toe strapping can also be effective in ameliorating symptoms (Fig. 3).4 In contrast to the Budin splint, toe strapping with tape has a lower profile, which allows for its use with arch supports and accompanying cushioned top covers. Intra-articular lesser MTPJ cortisone injection may actually propagate an acute-on-chronic plantar plate rupture5 and should be used judiciously under limited circumstances with protected weight bearing and concurrent toe strapping (see Fig. 3) for a minimum of 6 weeks.

Fig. 3 Bilateral Gerard Yu figure-of-eight toe strapping with 12-mm (0.5-in) paper tape placed on the base of the second toes to reduce hyperextension deformity at the MTPJ.4 Similar strapping can also be applied to the third toes as needed. This strapping is easy to perform and can be both diagnostic and therapeutic in its efficacy for treatment of predislocation syndrome.
When conservative treatment fails, surgical options for hammertoe correction can be divided into resectional arthroplasty, arthrodesis, or plantar plate repair. Hammertoes and lesser MTPJ pain may occur in isolation, or may be secondary to first ray insufficiency (ie, hallux valgus deformity). When hallux valgus is present, it must also be treated concurrently to adequately correct the position of the second toe and prevent recurrence.2,3,8 In cases of complex hammertoe deformity with lesser MTPJ pain, consideration should also be given to central metatarsal decompressional shortening osteotomies.2–4 Further consideration should be given to gastrocnemius recession when pathologic gastrocnemius equinus is present and contributing to increased forefoot load and thereby, lesser MTPJ pain and deformity.3,5
Arthroplasty
Hammertoe repair by means of simple proximal phalangeal head resection without Kirschner wire (K-wire) transfixation may lead to digital instability and/or malalignment secondary to tendon imbalance,2 particularly in the second and third toe. Isolated PIPJ resectional arthroplasty does not address the sagittal plane deformity that typically exists concomitantly at the MTPJ. This has led some surgeons to advocate for single-stage MTPJ capsular tendinous rebalancing, plantar plate repair,5,9,10 PIPJ resectional arthroplasty and/or fusion with K-wire transfixation across the MTPJ.2,11,12 In cases of hammertoe deformity with incongruity at the MTPJ, consideration should be given for open reduction of the MTPJ deformity with K-wire splintage and/or metatarsal shortening osteotomies when indicated.2,8,12
O’Kane and Kilmartin8 retrospectively reviewed 75 patients (100 toes) with an average age of 63 years who had an excisional second toe PIPJ arthroplasty without K-wire transfixation or MTPJ joint capsule release at an average of 44 months follow-up. They reported mean preoperative and postoperative AOFAS (American Orthopaedic Foot and Ankle Society) scoring of 46 and 94, respectively. However, 53 feet had adjunctive hallux valgus repair and 16 feet required both hallux valgus repair and a second metatarsal osteotomy. There were also 35 excisional arthroplasties on adjacent toes. Hence, the results of their scoring analysis were biased by the ancillary surgical procedures and not the isolated second toe PIPJ arthroplasty alone. The investigators cite the rapid return to some variety of footwear and activity at 2 weeks postoperatively as advantages to performing this PIPJ resectional arthroplasty without pinning. They further identify that the digit maintains some degree of desirable flexion after arthroplasty as another advantage. However, 31% of the toes in their study had various complications with floating toe the most common.8
Arthroplasty with K-wire splintage maintained for 6 weeks commonly results in a clinical outcome similar to PIPJ arthrodesis (Figs. 4–8). Coughlin and colleagues,11 in their review of 118 PIPJ resectional arthroplasties performed with intramedullary K-wire transfixation, found that 81% of the toes went onto PIPJ fusion and the remaining 19% had a fibrous union. In the absence of pain and instability, a fibrous union is not an indication for revisional surgery.2,11
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree