Fig. 22.1
The anatomic course of the suprascapular nerve. The suprascapular nerve (white arrows) leaves the brachial plexus and travels posteriorly under the transverse scapular ligament with the vein, while the artery (white arrowhead) travels over the ligament. The transverse scapular ligament can be identified at the base of the coracoid, just medial and posterior to the coracoclavicular ligaments. The retractor is retracting the supraspinatus muscle posteriorly. (Published with the permission of ©Felix H. Savoie, III 2015)
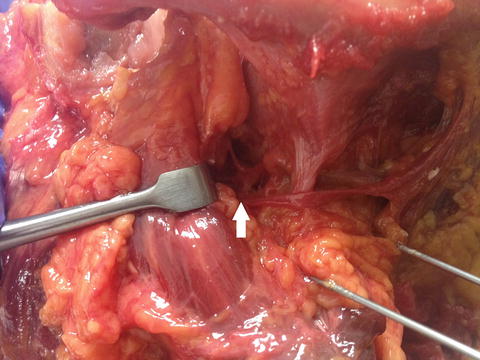
Fig. 22.2
Cadaveric dissection demonstrates the nerve branching at the white arrow, with a medial branch innervating the supraspinatus muscle, a branch diving deep along the floor of the supraspinatus fossa that continues to the spinoglenoid notch, and a small lateral sensory branch to the glenohumeral joint. (Published with the permission of ©Felix H. Savoie, III 2015)
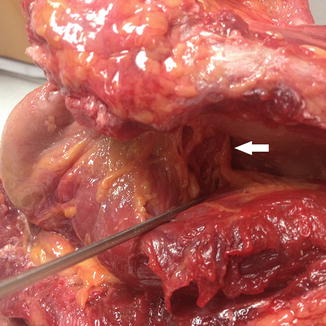
Fig. 22.3
The suprascapular nerve continues around the spinoglenoid notch at the base of the scapular spine (white arrow) and courses medially to innervate the infraspinatus muscle. In this photograph, the nerve can be seen branching out on the superior surface of the infraspinatus. (Published with the permission of ©Felix H. Savoie, III 2015)
Recent attention has been given to anatomic variants of the course of the suprascapular nerve and its associated artery and vein, with particular attention toward how these variants may be associated with compression and injury. Polguj et al. performed anatomic studies of 106 cadaveric specimens showing the constant path of the suprascapular nerve beneath the transverse scapula ligament in all specimens [19]. However, the course of the artery and vein was found to be highly variable, and a proposed classification system was offered. The majority of specimens (61 %) were found to have the suprascapular artery pass above the transverse scapular ligament and the vein below the transverse scapular ligament in type I of this classification (Fig. 22.1). Type II specimens showed both the artery and vein passing above the transverse scapular ligament; this configuration was present in about 17 % of specimens. Type III specimens showed both the artery and vein passing below the ligament (12 %). A type IV classification was reserved for other variants including double veins and vessels that passed below the anterior coracoscapular ligament (a ligament found in over half of the specimens dissected).
Pathogenesis
Extrinsic compression and traction of the suprascapular nerve has been shown to cause neuropathy. The suprascapular notch and the spinoglenoid notch are the two implicated locations of compression. Aiello et al. were able to distinguish between entrapment of the nerve at the spinoglenoid notch and the suprascapular notch, usually as a result of a ganglion cyst in the spinoglenoid notch [1]. Repetitive microtrauma as a result of overhead activities and sports may lead to direct or indirect traction-type injury to the nerve and nearby vasculature, resulting in ischemic injury to the nerve [22]. Iatrogenic injury to the suprascapular nerve has been reported during distal clavicle resection, positioning during spine surgery, and other surgeries on or near the shoulder. Acute trauma in the case of glenohumeral dislocations, proximal humerus fractures, and scapula fractures have also been implicated [4, 5, 25]. All of these above mentioned mechanisms of injury are likely to cause compression at the suprascapular notch due to the limited translational freedom of the nerve around the narrow confines of the notch, predisposing it to injury in extreme positions of scapular depression, retraction, or abduction [26]. Compression-related neuropathy as a result of the ganglion cyst or tumor is more often a result of compression at the spinoglenoid notch [10]. The ganglion cyst may be a result of labral or capsular violations with associated extravasation of synovial fluid. This association has been challenged, yet most experienced clinicians relate that a labral tear is usually found in the presence of paralabral cysts [9, 27].
The treatment of isolated spinoglenoid compression will be elaborated further in a subsequent chapter.
Presentation
Often mimicking rotator cuff pathology, suprascapular neuropathy presents as diffuse pain over the lateral and posterior aspects of the shoulder with associated weakness. Referred symptoms can be as far as the lateral aspect of the arm, ipsilateral neck, and anterior chest well. A careful history is necessary to reveal any episodes of trauma, such as a fall on outstretched extremity, or other direct force. Trauma may include a hyper-external rotational movement, such as seen in volleyball, tennis, and water polo. The athlete may complain of resultant “soreness and weakness” that may mimic an infraspinatus tendonitis.
Physical Exam
Inspection of the shoulder may reveal atrophy in the supraspinatus and infraspinatus fossae. In the very early stages, the upper infraspinatus, just below the scapular spine, is often the first place to note subtle atrophy. Looking downward at the scapular spine on a seated patient helps discern subtle spinati atrophy. Long-standing proximal compression may show wasting of both the supraspinatus and infraspinatus, with the deltoid maintaining its bulk. Compression at the spinoglenoid notch will often show isolated wasting of the infraspinatus. Symptoms, in this case, are often vague and diffuse without an obvious associated weakness in strength attributed to the posterior deltoid and teres minor compensation [7]. Strength comparison with the contralateral arm will often demonstrate a strength difference between the two sides. Provocative maneuvers can be utilized to further assess the severity of the symptoms, including the Whipple test (Fig. 22.4), whereby the patient positions the arm in 90° of forward flexion and maximal adduction and resists downward pressure. The infraspinatus strength may be assessed by resisted external rotation with the arm adducted or with positioning the arm in 90° of abduction and full external rotation. These tests are often positive early in the disease course. Impingement tests including the Neer sign and Hawkins test are often positive, secondary to weakness in the supraspinatus and infraspinatus muscles.


Fig. 22.4
The Whipple test is performed with the affected arm in 90° of forward flexion and full adduction, resisting a downward pressure. Pain and weakness indicate supraspinatus pathology. If the patient has poor posture and a protracted shoulder (a), the test is repeated holding the shoulder in a retracted position (b). Improved strength in this position is indicative of scapular dyskinesia. (Published with the permission of ©Felix H. Savoie, III 2015)
The suprascapular nerve stretch test (Fig. 22.5) has been described in order to reproduce the posterior shoulder pain associated with compression of the nerve at the suprascapular notch [12]. This test is performed by the examiner rotating the head of the patient laterally and away from the affected shoulder while retracting the shoulder with gentle traction, applying stretch to the nerve. A positive test elicits posterior shoulder pain.


Fig. 22.5
The suprascapular nerve stretch test is performed by rotating the head of the patient laterally and away from the affected shoulder while retracting the shoulder with gentle traction, applying stretch to the nerve. (Published with the permission of ©Felix H. Savoie, III 2015)
Imaging
Patients will often receive a full set of shoulder radiographs as part of their workup to exclude other causes of shoulder pain. In the absence of concomitant pathology, radiographs are usually normal. Occasionally one might see slight superior migration of the humeral head on the glenoid due to loss of the humeral head depression effect of the posterior cuff. Radiographs of the cervical spine may be warranted to exclude radicular causes of the patient’s symptoms. In the post-traumatic setting, radiographs of the scapula and clavicle may demonstrate callus formation from healing fractures resulting in compression of the nerve. Post and Mayer described a radiograph taken from anterior to posterior of the scapula with the beam directed caudally 15–30° for a view of the suprascapular notch [21]. Depending on the severity of any bony deformity, a computed tomography (CT) scan may be indicated.
Magnetic resonance imaging (MRI) is generally indicated as the next step in imaging workup subsequent to radiographs. MRI allows for definition of the course of the nerve, associated muscle atrophy, space-occupying lesions, and view of concomitant pathology such as rotator cuff tears and labral pathology. Edema followed by atrophy of the supraspinatus and infraspinatus is the first sign of compression distinguishable on an MRI (Fig. 22.6a, b) [14]. Long-standing compression will show marked atrophy of the associated rotator cuff musculature.
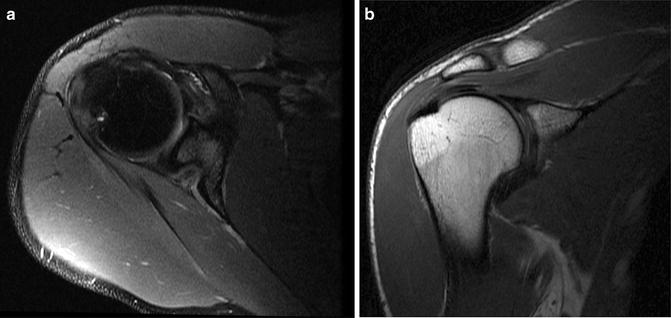
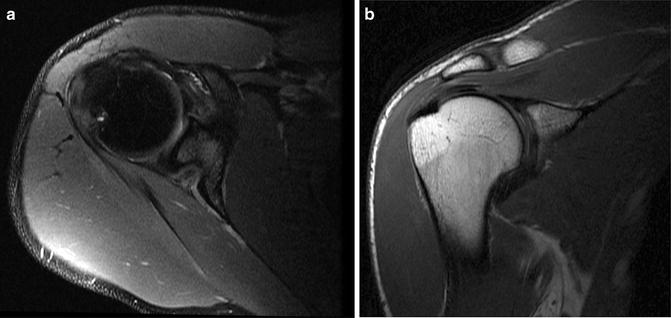
Fig. 22.6
MRI showing atrophy of the supraspinatus and infraspinatus muscles from long-standing compression of the suprascapular nerve in a young baseball pitcher. (a) Axial (b) Coronal (Published with the permission of ©Felix H. Savoie, III 2015)
Electromyographic nerve conduction studies may help specifically define the site of compression if questions still remain after the previous imaging studies are inconclusive. Severe atrophy in the musculature is associated with increased false-negative electrodiagnostic studies as the superficial electrical signal may be picked up by the more bulky deltoid muscle. In addition, the expertise of the electromyographer is paramount in the utility of electrodiagnostic studies, as a high degree of experience is required in order to properly execute the study [24].
Suprascapular diagnostic nerve blocks with local anesthetic have been described in certain cases to aid in diagnosis, with a positive test being defined as elimination of associated shoulder pain after local injection of the anesthetic [1]. The use of this test may be more practical with the use of ultrasound guidance, which has been well described for the suprascapular nerve as a diagnostic tool despite its limited appearance in the literature [17].
Nonoperative Treatment
The success of nonoperative treatment for suprascapular nerve-related symptoms is most closely related to the etiology of the problem. Injury to the nerve unrelated to direct compression has the best likelihood of recovery without surgery [20]. Symptoms that can be attributed to a defined site of compression are less likely to experience any improvement without surgical intervention. In the setting of non-compressive causes of nerve injury, a structured therapy program can be used with specific emphasis on scapula retraction, maintaining proper posture, and glenohumeral range of motion [23]. The appropriateness of duration of nonoperative treatment remains controversial. The correct diagnosis of a suprascapular nerve entrapment is often delayed, and it is common that several modalities of conservative treatment may have been administered to the patient over an extended period of time. This has led some authors to suggest operative treatment as soon as the correct diagnosis is made [20]. Others have suggested to administer a full 1-year course of conservative treatment in the absence of an obvious compressive lesion [16]. In cases where a clear spinoglenoid cyst is identifiable, aspiration of the cyst can result in sufficient decompression to permit nerve healing with sufficient rehabilitation. However, recurrence rates have been reported to be high [9, 27]. In more advanced cases, surgical decompression of either the suprascapular notch or spinoglenoid notch should be performed.
Operative Treatment
Indications for operative treatment include symptoms refractory to appropriate conservative treatment, and/or an identifiable compressive lesion to the suprascapular nerve [6]. Surgical decompression of the entrapped nerve has been shown to be successful in many series. Several open approaches have been described and have accompanying good outcomes. Vastamaki has described the open approach in which an incision is made directly over the supraspinatus fossa. The trapezius is split, allowing access to the supraspinatus muscle and fossa. The supraspinatus muscle can be retracted posteriorly to allow access to the suprascapular notch and the area of compression directly released. In most cases, the supraspinatus can also be retracted anteriorly, allowing access to decompress the spinoglenoid notch as well [28].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








