Supracondylar Femur Fractures: Open Reduction Internal Fixation
Sean E. Nork
Indications/Contraindications
Distal femoral fractures are common and affect patients of all ages. In older patients, these fractures are frequently the result of a fall from a standing position. However, in younger patients, high-energy mechanisms are common and include motor vehicle crashes, falls from height, and industrial injuries. In these patients, associated ipsilateral extremity injuries frequently occur. The entire lower extremity should be examined to identify any associated open wounds or neurovascular injuries. Although lateral and anterolateral open wounds are more common, medial and posterior open wounds exist and may suggest significant, associated, soft-tissue stripping. Compartmental syndrome, while rare, can occur in association with fractures of the distal femur and should be adequately evaluated.
The vast majority of supracondylar and/or intercondylar, distal, femoral fractures in adults are treated operatively because surgical stabilization allows early knee motion, patient mobilization, and may decrease the incidence of posttraumatic arthritis. Because of the significant muscular attachments surrounding the knee joint, maintenance of the proper anatomical and mechanical axes is difficult with nonoperative treatment. Closed management is usually reserved for elderly patients with significant medical co-morbidities and nonambulatory patients. Significant articular comminution and/or associated bone loss are not considered contraindications to operative treatment.
Preoperative Planning
Unlike many tibial plateau or pilon fractures, the majority of distal femoral fractures can be treated definitively with early operative fixation. If surgical treatment is imminently planned, the limb can be temporarily stabilized with a knee immobilizer, a bulky dressing,
or proximal tibial traction. In certain circumstances (open fractures with significant contamination, severe soft-tissue swelling, significant patient co-morbidities, unavailability of the proper implants and/or surgical personnel), surgery may be delayed. Depending on the age of the patient, the amount of shortening and the degree of comminution, a temporary, spanning, external fixation is often recommended.
or proximal tibial traction. In certain circumstances (open fractures with significant contamination, severe soft-tissue swelling, significant patient co-morbidities, unavailability of the proper implants and/or surgical personnel), surgery may be delayed. Depending on the age of the patient, the amount of shortening and the degree of comminution, a temporary, spanning, external fixation is often recommended.
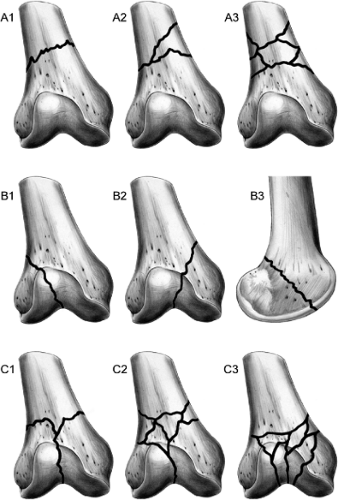
The initial radiographic evaluation consists of high-quality anteroposterior (AP) and lateral radiographs of the knee joint and the distal femur. Traction films are helpful in comminuted and shortened fracture patterns but may not be tolerated in all patients. Radiographs of the contralateral leg can assist with preoperative planning. Computed tomography (CT) scans can be helpful for understanding the patterns of comminution and for determining the appropriate surgical approach and implants. This is particularly true in high-energy injuries but may be useful in all distal femoral fractures. Coronal plane fractures of the medial and lateral condyles (Hoffa fracture) may be difficult to recognize on the injury and/or traction radiographs. Depending on the location of comminution in the distal femur, the surgical approach may require alteration. Despite numerous classification systems for distal femoral fractures, the AO/OTA system is the most useful, allows effective communication, and may influence surgical treatment (Fig. 23.1).
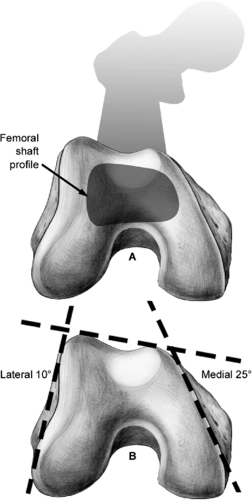
The distal femoral anatomy must be understood prior to considering a fixation strategy. The distal femur is trapezoidal when viewed from distal to proximal. The lateral metaphyseal surface is angulated approximately 10 degrees while the medial side surface is
angulated approximately 25 degrees (Fig. 23.2). This combination contributes to the widening of the condyles posteriorly relative to their anterior width. The lateral condyle extends farther anteriorly relative to the medial condyle, producing a posterior slope between the anterior condylar prominences when viewed from lateral to medial. The distal extent of the intercondylar articular surface is best appreciated on the lateral radiograph, which can be useful for determining the safe placement of implants during fixation. The central axis of the femoral shaft normally aligns with the anterior half of the femoral condyles as viewed laterally. This alignment is especially important to assess by surgeons considering the accurate placement of lateral plate constructs.
angulated approximately 25 degrees (Fig. 23.2). This combination contributes to the widening of the condyles posteriorly relative to their anterior width. The lateral condyle extends farther anteriorly relative to the medial condyle, producing a posterior slope between the anterior condylar prominences when viewed from lateral to medial. The distal extent of the intercondylar articular surface is best appreciated on the lateral radiograph, which can be useful for determining the safe placement of implants during fixation. The central axis of the femoral shaft normally aligns with the anterior half of the femoral condyles as viewed laterally. This alignment is especially important to assess by surgeons considering the accurate placement of lateral plate constructs.
Comparison radiographs with the contralateral knee are useful for determining the patient’s unique condylar width and distal femoral axes. Knowledge of the condylar width can be helpful for planning the length of implants placed in the distal femoral segment. Because of the distal femoral shape, the relative angulation of implants must be considered. Implants placed anteriorly and horizontally will be appreciably shorter than those placed perpendicular to the lateral cortex (and therefore with 10 to 15 degrees of posterior angulation). The mechanical axis of the lower extremity helps determine the proper, anatomic, valgus angulation of the lower extremity. The typical 5 to 9 degrees of anatomical tibiofemoral valgus
can be most accurately appreciated from a contralateral extremity radiograph. Similarly, the location of the mechanical axis at the knee joint can be determined intraoperatively. The normal valgus angulation of the distal femur becomes apparent during intraoperative lateral imaging as well. For the femoral condyles to overlap perfectly, the fluoroscopic beam must be appropriately positioned to compensate for the distal femoral valgus.
can be most accurately appreciated from a contralateral extremity radiograph. Similarly, the location of the mechanical axis at the knee joint can be determined intraoperatively. The normal valgus angulation of the distal femur becomes apparent during intraoperative lateral imaging as well. For the femoral condyles to overlap perfectly, the fluoroscopic beam must be appropriately positioned to compensate for the distal femoral valgus.
In general, a formal preoperative plan should be constructed on tracing paper in anticipation of the surgical procedure. This requires the availability of radiographs printed at 100% magnification. With the rapid conversion to digital recording of radiographic images at many hospitals, preoperative templating is quickly becoming a lost art. The outline of the normal distal femur should be drawn first. Then, the injured extremity-fracture fragments should be drawn on a separate piece of templating paper. The fractured segments should then be drawn into the normal outline of the distal femur (with the proper left vs. right reflection) on both the AP and lateral drawings. Based upon the fracture configuration, the bone quality, and the availability of implants, an appropriate fixation construct can be chosen.
Temporary, Spanning, External Fixation
Temporary, spanning, external fixation can be helpful in multiply injured patients and in patients with complex fracture patterns. It usually consists of a knee joint–spanning external fixator with pins placed into the tibia and the femur. Femoral pin placement can be directly anterior, directly lateral, or anterolateral. Regardless of their entry orientation, pins should be placed proximal to the anticipated surgical incision(s) for definitive fixation. Some knee flexion (10 to 20 degrees) is recommended and improves the commonly observed extension deformity of the distal femoral segment.
Fixation Devices
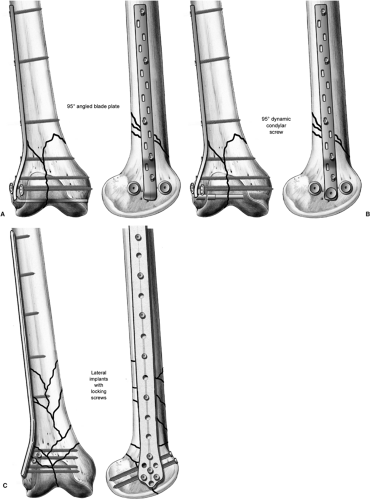
The primary focus of this chapter is on the fixation of combined supracondylar and intercondylar (AO/OTA 33C) distal femoral fractures. However, because of the versatility and number of implants appropriate for fractures of the distal femur, other fracture patterns will be mentioned. Fractures without articular involvement (33A fractures) can be treated with antegrade nails, retrograde nails, and lateral plate constructs. The choice of implant in these injuries is largely dependent upon the surgeon’s comfort, the patient’s associated injuries, and the predicted management of any potential complications due to the injury or the treatment. Fractures with partial articular involvement (lateral condyle fractures, medial condyle fractures, or tangential fractures of the posterior condyle) can be treated with lag screws, conventional plates, or a combination of both. For fractures with both supracondylar and intercondylar involvement, effective implants include conventional lateral plates (condylar buttress plate, precontoured lateral plates specific for the distal femur), lateral plates with a fixed angle (95-degree angled blade plate, dynamic condylar screw), and lateral locking plates (Fig. 23.3). In general, the surgical tactic and reduction are more important than the implant.
Conventional lateral plates are inexpensive and easy to apply. Angulation of the screws in the distal segment may be advantageous in fractures where multiple lag screws are required to stabilize any articular-surface comminution. The biggest disadvantage is the inability of these implants to prevent postoperative varus deformation due to screw loosening, especially in the distal articular block. This may be most significant in open fractures, patients with osteopenia, and fractures with associated bone loss.
Fixed-angled lateral implants include the 95-degree angled blade plate, the 95-degree condylar screw, and the lateral fixed-angled screw-plate devices. All of these implants have the advantage of minimizing varus deformation by eliminating screw toggling in the distal metaphyseal bone. Blade plates can be placed quite distally and do not remove significant bone from the distal articular segment. However, these implants are technically difficult to place and require a single perfect entry location. This is especially important in distal
femoral fractures with associated articular comminution that require a prior surgical stabilization of the multiple articular fragments. These implants may prevent ideal placement of the condylar blade distally. The dynamic condylar screw is easier to implant and allows submuscular implantation. However, this device removes a significant amount of bone and cannot be placed as distally as an angled blade plate. Locking plates, in addition to maintaining the coronal plane reduction, allow for placement of multiple fixed implants (screws) into the distal segment. Thus, they allow for some flexibility in screw location and may be more forgiving. These implants have the further advantage of having specifically designed surgical jigs that enhance submuscular implantation.
femoral fractures with associated articular comminution that require a prior surgical stabilization of the multiple articular fragments. These implants may prevent ideal placement of the condylar blade distally. The dynamic condylar screw is easier to implant and allows submuscular implantation. However, this device removes a significant amount of bone and cannot be placed as distally as an angled blade plate. Locking plates, in addition to maintaining the coronal plane reduction, allow for placement of multiple fixed implants (screws) into the distal segment. Thus, they allow for some flexibility in screw location and may be more forgiving. These implants have the further advantage of having specifically designed surgical jigs that enhance submuscular implantation.
Surgery
Patient Positioning
The patient is positioned supine on a radiolucent table that allows unimpeded fluoroscopic imaging in both planes. A small bump placed beneath the ipsilateral hip should be sized to ensure that the femur is in neutral rotation, assisting with the intraoperative assessment of extremity rotation during and after reduction. The knee is placed in slight flexion over a custom ramp or folded blankets with an additional small rolled bump at the fracture site (Fig. 23.4). This improves the sagittal plane reduction of the fracture by relaxing the primary deforming force of the gastrocnemius. In addition, this position facilitates intraoperative, lateral, fluoroscopic imaging of the proximal thigh without obstruction from the contralateral extremity.
The entire limb is prepped and draped from the ipsilateral pelvis to the toes, allowing intraoperative manipulation of the leg and access to the femur proximally as needed. If traction radiographs in the AP and lateral planes have not been obtained previously, these can be obtained at this time. A sterile tourniquet can be applied proximally if desired.
Incision and Surgical Approaches
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree