Subtrochanteric Femur Fractures: Reconstruction Nailing
Thomas A. Russell
Indications/Contraindications
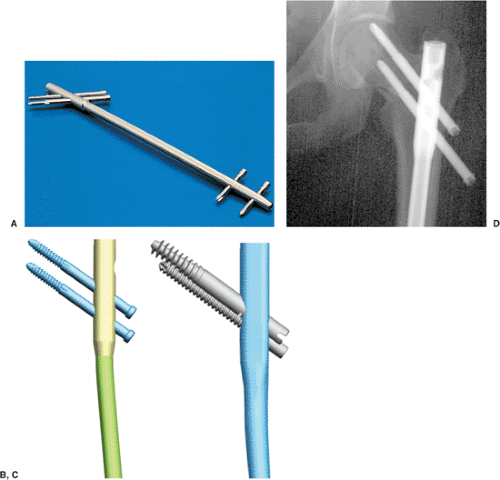
Reconstruction or cephalomedullary nails are specialized, antegrade, femoral, intramedullary nails designed to provide fixation into the femoral head and neck for selected, complex, proximal-femoral fractures. Reconstruction nails are a subset of cephalomedullary nails that are distinguished by two proximal interlocking screws that permit sliding lag-screw fixation into the femoral head, which enhance rotational stability in the proximal femur, and distal interlocking screws, which ensure rotational and axial stability. In addition, the geometry of the nail is altered throughout its length with variations in cross section to maximize nail strength and to minimize its stiffness. This modulation in cross section is especially important in the subtrochanteric region where fatigue stresses are relatively high. All reconstruction nails have an anterior bow to facilitate nail insertion.
The original reconstruction nail was the Russell-Taylor Reconstruction Nail (Smith & Nephew, Memphis, TN) introduced in 1986. It was a closed-section implant designed for a piriformis entry. The nail was calibrated to approximate 95% of the intact bending stiffness and 50% of the rotational stiffness in the intact femoral diaphysis. The proximal cross section was modified to enable a higher fatigue life in the subtrochanteric region and was 15 mm in diameter in this area with the diaphyseal diameter available in 12, 13, and 14 mm (Fig. 20.1). This original design was frequently referred to as a “second-generation interlocking nail.” Subsequently, newer generations of reconstruction nails have been introduced by various manufacturers. They vary in their proximal geometries, diameter, cross-sectional design, and proximal screw geometries (see Fig. 20.1A–C).
Mechanically, a statically locked reconstruction nail can be used to stabilize injuries from the femoral neck to approximately 4 cm above the knee. Reconstruction nails were originally designed for subtrochanteric femoral fractures, pathologic femoral fractures, and
selected, ipsilateral, femoral neck and shaft fractures. Segmental fractures of the femur, in which the proximal fracture extends into the upper femoral metaphysis, are also good indications for reconstruction nails. Reconstruction nail techniques are also used for deformity correction and stabilization of malunions, nonunions, and failed plate fixation of subtrochanteric femur fractures.
selected, ipsilateral, femoral neck and shaft fractures. Segmental fractures of the femur, in which the proximal fracture extends into the upper femoral metaphysis, are also good indications for reconstruction nails. Reconstruction nail techniques are also used for deformity correction and stabilization of malunions, nonunions, and failed plate fixation of subtrochanteric femur fractures.
A reconstruction nail should not be considered the nail of first choice for diaphyseal fractures of the femur because of the complexity of targeting and placing screws in the femoral head. However, in pathologic fractures and osteoporotic femoral fractures, reconstructions nails are often recommended to prevent subsequent femoral-neck fractures. Reconstruction nailing is contraindicated in children with open, proximal, physeal plates.
Second-generation reconstruction nails with piriformis entry portals should be avoided in displaced femoral-neck fractures and four-part intertochanteric fractures due to their propensity for fixation loss with rotation and varus loading. This so-called “Z-effect” results in loss of proximal screw fixation with intrusion of the cephalic screw into the joint space and subsequent backing out of the inferior head and neck screw (see Fig 20.1D).
In an effort to minimize fracture deformity and loss of reduction or fixation, third-generation reconstruction nails, such as the TriGen Trochanteric Reconstruction Nail (Smith & Nephew, Memphis, TN) for use with trochanteric entry portal, have been designed.
In an effort to minimize fracture deformity and loss of reduction or fixation, third-generation reconstruction nails, such as the TriGen Trochanteric Reconstruction Nail (Smith & Nephew, Memphis, TN) for use with trochanteric entry portal, have been designed.
Russell and Taylor described a classification for subtrochanteric femur fractures based on the presence or absence of fracture involvement of the lesser trochanter/medial calcar and greater trochanter (piriformis fossa) (Fig. 20.2). Fractures involving the lesser trochanter but without extension into the greater trochanter (Russell-Taylor IB), are perhaps the best indication for a piriformis-portal reconstruction nail (Fig. 20.3). Historically, group 1 Russell-Taylor fractures were considered optimal for intramedullary nail techniques with piriformis portal approaches, and group 2 Russell-Taylor fractures were most often treated with plate and screw techniques. Now, almost 20 years since the first reconstruction nail was introduced, the techniques of nailing have undergone such significant improvements that many Russell-Taylor group II fractures can be addressed with an intramedullary hip screw (IMHS) or third-generation trochanteric reconstruction nails.
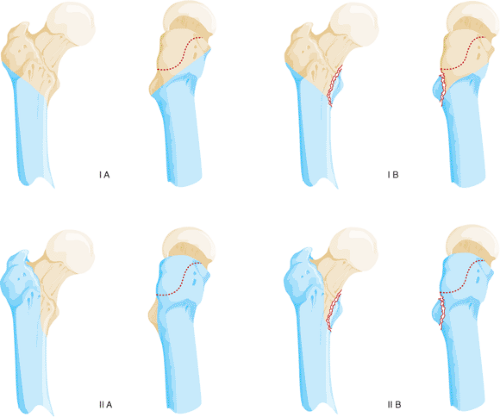 Figure 20.2. Diagram of components of Russell-Taylor IB subtrochanteric pattern with greater trochanter intact and lesser trochanteric fracture. |
Preoperative Planning
Subtrochanteric fractures often occur in high-energy trauma in younger patients and lower-energy falls in the elderly. With high-energy subtrochanteric fractures, associated injuries are found in up to 50% of patients. Open subtrochanteric fractures are rare, as are compartment syndromes, but both of these complications increase the morbidity of the injury if rapid assessment and treatment are not instituted.
Patients with subtrochanteric femur fractures invariably have hip or thigh pain, an external rotation deformity, and angulation in the proximal thigh if the extremity is not splinted. Frequently (depending on the mechanism and time elapsed since injury), ecchymosis and swelling of the thigh are apparent. Neurological or vascular injuries are uncommon with subtrochanteric fractures unless they are the result of penetrating trauma.
Preoperative radiographs should include anteroposterior (AP) and lateral views of the entire femur including the hip and knee. The radiographs should be carefully inspected to rule out intra-articular propagation of fractures or concomitant degenerative disease. In patients with complex fracture patterns or extensive comminution, radiographs of the uninjured femur may be used to estimate nail diameter and length. Radiographic templates for planning an operation in which reconstruction nails are available from most of the implant manufacturers.
If surgery is delayed, restoration of length at the fracture site must be obtained with skeletal traction before closed nailing. Failure to restore length may lead to excessive intraoperative traction and resultant pudendal or sciatic nerve injuries.
High-quality radiographs must be scrutinized to determine whether the fracture extends into the greater trochanter and piriformis fossa. With the widespread use of rapid CT scanners in trauma units, inclusion of proximal femur scans of patients with hip injuries is an excellent method for determining trochanteric involvement. In patients with extension of the fracture above the lesser trochanter, a coronal split in the proximal fragment is frequently present. This may result in comminution of the proximal fragment with loss of the entry portal during reaming and nailing. In these cases, reconstruction nailing may be contraindicated. If the fracture is nailed, an open reduction of the proximal fragment with provisional stabilization of the trochanteric region via reduction forceps is strongly advised.
Most reconstruction nails are now available in sizes ranging from 10 to 16 mm in diameter with lengths between 240 and 500 mm. The nails are right-sided and left-sided, to compensate for the anteversion of the femoral neck in relation to the shaft axis in the coronal plane. To facilitate screw entry into the femoral head, the proximal locking-screw holes are oriented anteriorly 8 to 15 degrees in relation to the distal screw holes. When
using reconstruction nails, surgeons typically also use two sliding lag screws proximally to maximize purchase in the femoral head and to minimize rotation of the proximal fragment. These lag screws vary between 5 and 8 mm in diameter.
using reconstruction nails, surgeons typically also use two sliding lag screws proximally to maximize purchase in the femoral head and to minimize rotation of the proximal fragment. These lag screws vary between 5 and 8 mm in diameter.
Precise knowledge of the neck-shaft angle of the screws in relation to the nail, spacing between the proximal screws, and their enclosed diameter are important in implant selection. Nail neck-shaft angles vary from 125 to 135 degrees. Higher-angle designs maximize sliding capabilities but are difficult to insert in hips with a relative varus position. Lower-angle designs have higher stresses and less sliding capability but are easier to insert. Most designs are moving toward a compromise of 130 degrees. In most designs, reconstruction nails have an effective spread between the two proximal screws of 11 to 21 mm. Measurement of the preoperative radiographs is necessary to understand the patient’s neck-shaft angle and to plan screw spacing and final nail position. Reconstruction nails are typically enlarged proximally to compensate for the higher stresses in the subtrochanteric region. This must be recognized in preoperative planning because additional reaming of the proximal fragment is necessary in relation to the diaphyseal reaming. Distal interlocking screws are usually 4.5 to 6.4 mm in diameter and vary from full-threaded to partially threaded designs.
Appropriate nail length and diameter depend on the size of the patient and the extent of femoral comminution. To minimize the risk of nail failure, the largest implant suitable for the patient should be used such that excessive amounts of cortical bone are not removed. Even when interlocking is used, the nail should fill the medullary canal at the isthmus to minimize translational deformities. For maximal stability, static locking is recommended in acute fractures. The nail tip should extend into the distal femoral metaphysis to avoid stress risers in the diaphyseal area and facilitate distal interlocking.
Surgical Technique
I currently use the minimally invasive nail-insertion technique (MINIT) in conjunction with the TriGen nail system with both piriformis and trochanteric nail designs. MINITs are designed to protect soft tissues and preserve bone; they are not just percutaneous techniques. They emphasize precise portal placement and preservation, as well as trajectory control, to avoid malreductions and damage to the proximal femur.
Patient Positioning
The supine position for patients is recommended for reconstruction nailing because it is familiar to most surgeons and allows adequate visualization of the hip in both AP and lateral views, which is critical to successful implantation of the device. The lateral decubitus position, which allows better visualization of the entry portal than does the supine position, is helpful with revision nailing, especially in patients who have experienced previously failed nailings due to incorrect entry portals. It is also helpful with reverse obliquity fractures because the lateral position reduces the medial translation of the shaft component.
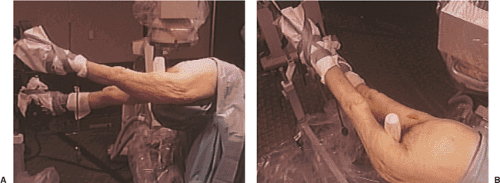
With the patient in the supine position, the unaffected limb and trunk are abducted while the affected extremity is adducted. To reduce the distal shaft fragment to the proximal fragment, the affected hip is flexed 15 to 35 degrees with maintenance of the heel-to-toe relation (Fig. 20.4). Traction is applied after flexion positioning through the foot holder attached to the fracture table or through a skeletal pin in the distal femur or proximal tibia. Rotational alignment of the proximal fragment is determined with the image intensifier. The distal fragment is rotated to align with the proximal fragment (a true lateral of the knee is confirmed with overlapping of both femoral condyles). The surgeon must remember that femoral-neck anteversion in adults averages 15 degrees in Caucasian populations, but it may be up to 30 degrees in Asian populations. In the supine position, the leg will usually lie in 0 to 15 degrees of external rotation when the distal fragment is correctly rotated. In the lateral decubitus position, the foot and leg should be internally rotated approximately 15 degrees to match the tendency of the femoral head to orient toward the floor in a pendulum-like fashion.
Patient Preparation
The patient should be prepped and draped from the iliac crest, including the buttocks and lateral thigh, distally to below the knee. The image-intensifier arm should be covered with a sterile isolation drape. A first-generation cephalosporin (or substitute in the patient with penicillin allergies) is administered. Vancomycin or an aminoglycoside is added if the fracture is open. Usually cephazolin (1 g by IV) is continued for 24 to 48 hours after surgery in patients with closed fractures. Reconstruction nailing of open fractures should be performed only after appropriate debridement and irrigation of the open fracture wound. Delayed nailing is recommended for grade IIIB fractures. Reprepping and redraping of the extremity are required to minimize cross contamination at the nail insertion site.
Surgical Approach (Russell-Taylor Reconstruction Nail 1986)
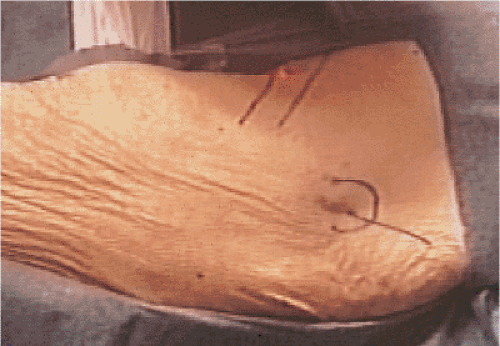
A 10-cm, oblique, skin incision is made just proximal to the greater trochanter (Fig. 20.5). The fascia of the gluteus maximus is incised, and the muscle is opened in line with its fibers. The subfascial plane of the gluteus maximus is identified, and the trochanteric or piriformis fossa is palpated.
Femoral Preparation
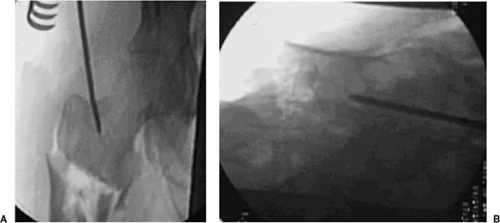
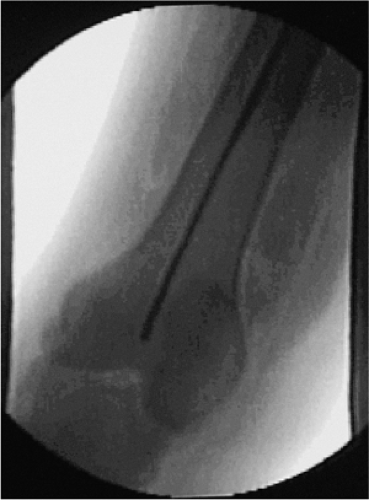
Establishing the correct portal for nail entry is crucial. Incorrect starting points can lead to angular deformities. For conventional, reamed, piriformis, intramedullary nailing, the correct starting point is in the piriformis fossa. However, for reconstruction nailing, the portal of entry is slightly anterior to the fossa. Because the femoral neck arises from the anterior portion of the proximal femur, moving the starting point 3 to 4 mm anteriorly facilitates proximal screw insertion. A 3.2-mm threaded guide pin is inserted at the entry site and confirmed by fluoroscopy to be in the midline of the femur in both AP and lateral views (Fig. 20.6). The entry portal is enlarged with the cannulated reamer over the guide pin (Fig. 20.7). If the proximal femoral fragment is flexed, externally rotated, and adducted to such a degree that the entry portal cannot be visualized, then the surgeon should manipulate the proximal fragment with a pointed reduction forceps or percutaneously inserted Schanz pin into a position such that the AP projections show a normalized fragment.
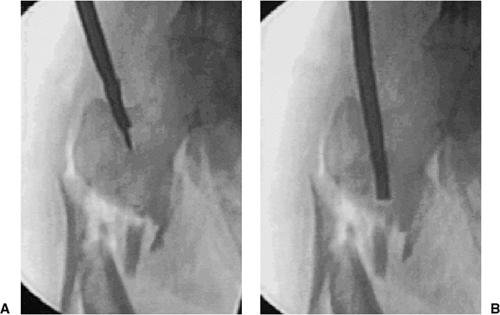 Figure 20.7. A,B. For correct entry portal, the guide wire should be overreamed with an 8-mm cannulated rigid reamer. |
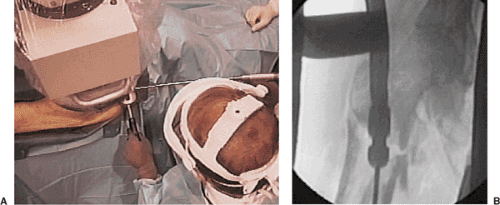
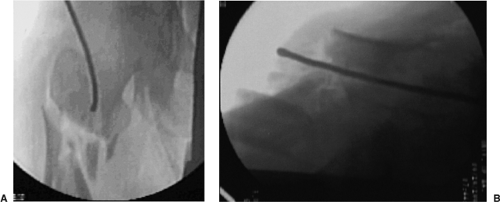 Figure 20.8. A,B. A 3.2-mm guide wire is inserted into fracture site. The tip of wire is bent to facilitate fracture reduction. |
To assist in reduction of the shaft fracture, a ball-tipped guide wire is bent at its tip. The wire is advanced to the level of the fracture with the curve opposing the medial cortex. Its position is confirmed within the femur by AP and lateral views taken with the image intensifier (Fig. 20.8). The proximal fragment is reduced to the distal fragment manually or with an internal fracture-alignment device (Fig. 20.9). The guide wire is advanced into the center of the distal fragment until its tip reaches the distal femoral-epiphyseal scar. The position of the guide wire is verified within the femur by image intensification (Fig. 20.10).
The femur is reamed in 0.5-mm increments from 9.0 mm to at least 1.0 mm more than the proposed nail diameter. In patients with a large anterior bow of the femur, as seen on lateral radiographs, or fracture extension into the distal one fourth of the femur, the surgeon should overream 1.5 to 2.0 mm larger than the nail diameter. The final reamer diameter should be verified with the reamer template before nail selection and insertion. A nail that has a larger diameter than the last reamer used should never be inserted. The proximal 8 cm of the femur is reamed to 15 mm in diameter with progressive reamers (starting with a 9-mm reamer) to accommodate the enlarged proximal end of most reconstruction nails (Fig. 20.11). Because the proximal fragment must be reamed substantially, the surgeon must avoid the destruction of the proximal entry portal that can be caused by eccentric reaming, which usually occurs during insertion of the reamer and during its extraction. To avoid this complication, a slotted hammer or other instrument to direct a medial force on the reamer shaft should be used during insertion and extraction (Fig. 20.12).
Verification of the proper nail length may be determined by two separate methods: the guide-wire method or the nail-length gauge. With either method, residual distraction at the fracture site must be eliminated. In the guide-wire method, the distal end of the guide wire is placed between the proximal pole of the patella and the distal femoral-epiphyseal scar, while a second guide wire is overlapped to the portion of the reduction guide wire extending proximally from the femoral entry portal. To determine nail length, the length (in mm) of the overlapped guide wires is subtracted from 900 mm. In another alternative, a nail-length ruler is placed on the skin of the anterior thigh (unaffected femur preoperatively; affected femur intraoperatively) with its distal end between the proximal pole of the patella and the distal femoral-epiphyseal scar. The c-arm is moved to the proximal end of the femur, and the correct nail length is read directly from the stamped measurements on the nail-length ruler.
The medullary exchange tube is placed over the guide wire to maintain fracture reduction while the ball-tip guide wire is replaced with a nail-driving wire (without ball tip). The medullary exchange tube is removed. With the Russell-Taylor system, the reaming guide rod and nail driving rods are identical, so placement of the medullary exchange tube is unnecessary.
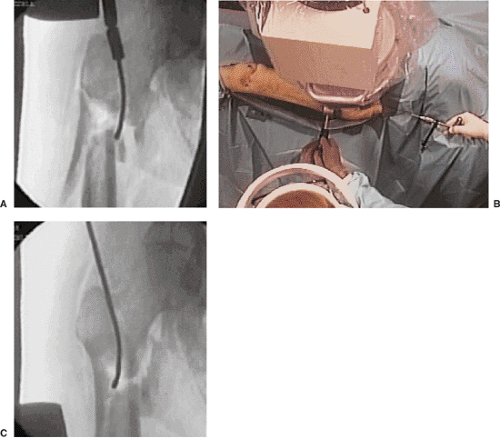 Figure 20.9. A–C. Combination of external force, internal guide, and adjustment of fracture table into abduction to accomplish fracture reduction. |
 Figure 20.11. Progressive flexible reamers in 0.5-mm increments with proximal 8- to 9-mm overreaming for reconstruction-nail proximal expansion. |
Nail Insertion
The appropriate nail is attached to the proximal driving/proximal drill guide. When assembled properly, the nail will have an anterior bow, and the orientation of the proximal drill guide points laterally.
Either the sliding hammer or supine driver is assembled to the proximal drill guide, and the nail is inserted over the guide wire. The proximal drill guide acts as a handle to control rotation and aid in insertion of the nail (Fig. 20.13). The surgeon must not strike the proximal drill guide directly, because this may deform the targeting device and compromise proximal interlocking. Once the nail has been inserted, the proximal targeting device should be retightened. The nail is driven under radiographic control to within 1 to 2 cm of its anticipated depth.
The anatomy of the proximal femur varies from person to person, so a reconstruction nail is inserted to the point where the upper end of the nail will accommodate two proximal screws into the femoral head. Frequently, minor adjustments in nail position, either proximal or distal, are necessary to line up the holes in the nail within the femoral head and neck. Nail insertion and screw placement can be initially performed with the nail-length ruler and a radiopaque ruler or guide. Its outline is drawn with a skin marker over the femoral head and neck (Figs. 20.14 and 20.15). With the nail nearly fully seated, the inferior drill sleeves are placed into the proximal drill guide to extrapolate the eventual location of the inferior screw.
The c-arm is positioned to obtain a true lateral view of the femoral head and neck. The proximal targeting guide is aligned with the c-arm axis by rotating the proximal drill guide
in the transverse plane (Fig. 20.16). If the proximal targeting device is radiopaque, the guide is centralized with respect to the femoral head, bisecting the femoral head in the coronal plane as seen on the true, lateral, c-arm view. The posterior and anterior portion of the femoral head must be seen in relation to the proximal drill guide for the surgeon to confirm that the screws will be contained within the femoral head (Fig. 20.17). Further verification of the proximal guide wires, drill bits, and locking screws may be obtained with oblique c-arm views. With a skin marker, a horizontal line is drawn on the lateral thigh as a reference to correct rotation of the proximal drill guide (Fig. 20.18). The traction is released, and the nail is seated. The intramedullary guide wire is removed from the femur.
in the transverse plane (Fig. 20.16). If the proximal targeting device is radiopaque, the guide is centralized with respect to the femoral head, bisecting the femoral head in the coronal plane as seen on the true, lateral, c-arm view. The posterior and anterior portion of the femoral head must be seen in relation to the proximal drill guide for the surgeon to confirm that the screws will be contained within the femoral head (Fig. 20.17). Further verification of the proximal guide wires, drill bits, and locking screws may be obtained with oblique c-arm views. With a skin marker, a horizontal line is drawn on the lateral thigh as a reference to correct rotation of the proximal drill guide (Fig. 20.18). The traction is released, and the nail is seated. The intramedullary guide wire is removed from the femur.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree