Subtrochanteric Femur Fractures: Plate Fixation
Michael J. Gardner
Eric E. Johnson
Dean G. Lorich
Indications/Contraindications
Open reduction and internal fixation (ORIF) with a fixed-angle plate, while used less commonly today, is an excellent method of treatment for selected subtrochanteric femur fractures (1,2,3,4,5,6,7,8,9,10,11,12,13). The blade plate has traditionally been used most commonly, but with the recent development and refinement of locking screw-plate technology, fixed-angle screw-plate constructs are being used more frequently. Plate fixation has a long history of successful application for proximal femur fractures, but instills a certain degree of anxiety among many surgeons. Outside of trauma centers, fixed angle plates are infrequently used implants. However, these implants offer several advantages when compared with other forms of fixation for proximal femoral fractures (4). They can be used in severely comminuted fractures, ipsilateral hip and shaft fractures, and subtrochanteric fractures with extension into the base of the neck or peritrochanteric region.
Blade plates and locking plates possess many unique qualities found with few other implants. They offer excellent stability and rotational control in complex fractures, can be used after corrective osteotomy about the hip, provide immediate fracture compression through surgeon-controlled application, and can offer valuable salvage options for failed fixation of other devices used in the proximal femur. Like any technically demanding procedure, immediate and long-term outcomes are optimized with experience and mastery of the surgical technique. Fixed-angle plating is an excellent implant when using indirect reduction and biological plating of both proximal and distal femoral fractures (4,14,15). Indirect reduction and fixation with these devices provide mechanically sound stabilization, allowing rapid mobilization and early, protected, weight bearing.
Fixed-angle plating, with either a standard blade plate or a fixed-angle locking-screw plate system, is indicated for many of proximal femoral fractures, including subtrochanteric and subtrochanteric-intertrochanteric fractures, fractures with extension into the basilar femoral neck, and some combined femoral-shaft and femoral-neck fractures. Alternative implants for these fractures include dynamic condylar screw devices and reconstruction cephalomedullary nails (5,9,12,16,17). Relative contraindications to traditional fixed-angle plate osteosynthesis for subtrochanteric fractures include elderly patients with osteoporotic
bone whose poor bone quality may compromise extramedullary fixation stability; unreliable patients who cannot comply with protected, postoperative, weight bearing; and surgeons unfamiliar with the technique.
bone whose poor bone quality may compromise extramedullary fixation stability; unreliable patients who cannot comply with protected, postoperative, weight bearing; and surgeons unfamiliar with the technique.
In general, two operative techniques are available for reduction of the proximal femur with fixed-angle plates: direct or indirect reduction. Direct reduction is recommended when the injury involves two main, large fragments (proximal and distal shaft fragments) and only one or two butterfly fragments with minimal comminution. Anatomic reduction and individual lag-screw fixation of the large butterfly fragments can usually be achieved without difficulty (16). Indirect or biological reduction is the preferred technique when moderate to severe comminution is present. In the latter case, anatomic reduction of individual fragments is technically impossible, and the required soft-tissue stripping of the fragments leads to devascularization. The goal of indirect reduction is to restore anatomic length, axis alignment, and rotation of the extremity, using both the implant and a femoral distractor in concert (4). The most appropriate method of fixation is a bridging technique in which a long plate, with relatively few, well-spaced, possibly locking, screws are used. Indirect reduction also relies upon the ability of the surgeon to tension the soft-tissue envelope with distraction of the fracture back to length with minimal disturbance of the surrounding fracture hematoma and periosteum.
Preoperative Planning
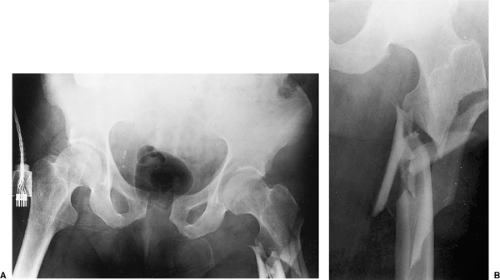
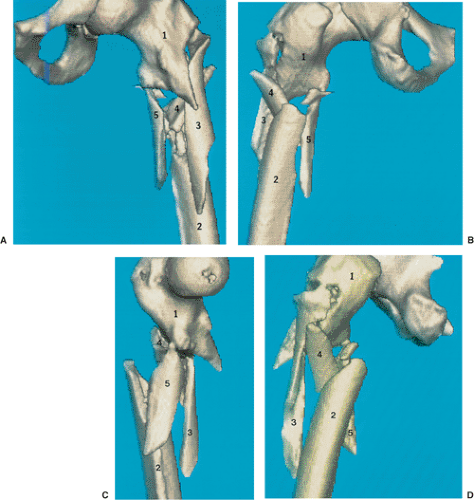
Accurate preoperative planning is critical when a fixed-angle plate is to be used for proximal femoral fractures. The surgeon should be familiar with implants and techniques of the AO/ASIF group before attempting this procedure. To avoid intraoperative complications, the surgeon must address several key points in preoperative planning of plate osteosynthesis. If a blade plate is being planned, the correct insertion site of the blade, the appropriate length of both the blade and the plate portion of the device, and the number of lag and plate compression screws are important to consider. If a locking plate will be used, the surgeon should consider the proximal or distal position of the plate that is necessary to allow correct placement of the screws into the femoral neck and understand that the length of the plate is crucial. The first step in planning osteosynthesis is to reconstruct the proximal femoral fracture by drawing all the individual fracture fragments into a reduced position. Frequently, multiple radiographs of the involved side are required because of fracture fragment displacement and rotation (Figs. 19.1 and 19.2).
In blade plating, the key to a good reduction is correct placement of the blade, and thus the next step is to determine the correct entry site of the seating chisel in the lateral greater trochanter. Most commonly, this is just proximal and lateral to the most prominent portion of the greater trochanteric ridge (Fig. 19.3). Using this landmark will, in the majority of cases, place the blade in the inferior portion of the femoral head and proximal to the inferior aspect of the femoral neck.
To assist in planning the subtrochanteric fracture reduction, AO blade-plate templates can be used to estimate the blade length and side-plate size. Blade lengths are available in 10-mm increments, starting at 50 mm, and side plate lengths are determined by the number of holes, which range from 5 to 26 holes with special order implants. The blade portion of the plate should reach to within 1.0 to 1.5 cm from the inferior central portion of the femoral-head articular surface. Estimation of the side plate length and number of screw holes below the most distal extent of the fracture is possible from the preoperative plan. At least four screws engaging eight cortices are necessary distal to a comminuted subtrochanteric fracture. Alternatively, the plate length may be increased, and screws may be spaced out along the length of the shaft fragment. This approach distributes the deforming forces over a greater distance and leads to a more stable construct. After planning the reduction of the fracture fragments into an acceptable position and tracing the most appropriate plate template over the reconstructed femur, the surgeon confirms the preoperative plan in a step-wise fashion, verifying the implant size, number of screws above and below the fracture, and the correct trochanteric entrance site.
When planning preoperatively for a locking screw-plate device much of the templating is similar to process use for a blade plate, with several additional issues requiring attention. Once the fracture is reconstructed on paper the right or left AO template should be selected, and the appropriate plate length can be determined. Plate lengths vary from 2 screws to 16 screws along the shaft of the plate. These newly designed plates have special combination-plate screw holes that allow either 4.5-mm compression screws or 4.0-mm or 5.0-mm locking screws to be inserted. Three fixed-angle screws are used for proximal fixation into the femoral head and neck, at angles of 95 degrees (7.3-mm screw), 120 degrees (7.3-mm screw), and 135 degrees (5.0-mm screw). There is little room for adjustment after inserting these screws once the plate placement is decided, so the correct plate position on the lateral femoral cortex is necessary. As with a blade plate, recent improved understanding in biological plating techniques has indicated that a longer plate with well-spaced screws, leaving several holes unfilled, is preferable.
Surgery
Surgery is performed by placing the patient in either a lateral decubitus position with cross-table fluoroscopy, or via supine positioning on a radiolucent fracture table. If lateral positioning is used, the extremity is prepped and draped free, allowing manipulation of the fracture fragments and facilitating “frog lateral” views that provide orthogonal x-ray visualization of the fracture and correct position of the plate and screws in the proximal femur.
A direct, lateral, surgical approach to the femur is performed, extending from several centimeters proximal to the greater trochanter to a level distal enough to allow reduction of the side plate to the femoral shaft (Fig. 19.4). After dissection through skin and subcutaneous tissue, the tensor fascia lata is incised and the vastus lateralis is released from the
posterior aspect of the femur and intermuscular septum and reflected anteriorly. It is important to adequately expose the greater trochanter. During this dissection, the surgeon should take care to minimize stripping of individual comminuted bone fragments (Fig. 19.5).
posterior aspect of the femur and intermuscular septum and reflected anteriorly. It is important to adequately expose the greater trochanter. During this dissection, the surgeon should take care to minimize stripping of individual comminuted bone fragments (Fig. 19.5).