Subtrochanteric Femur Fractures: Intramedullary Nailing
Clifford B. Jones
INTRODUCTION
Subtrochanteric femur fractures are much less common than hip or shaft fractures. They are usually associated with high-energy trauma in young adults or with lower-energy falls in the elderly. The subtrochanteric region of the femur is an area of high compressive stresses medially along the lesser trochanter and calcar and correspondingly high distraction forces laterally along the greater trochanter and proximal femur. Successful treatment methods require neutralization of these forces while maintaining the blood supply to enhance healing.
Intramedullary nailing of the proximal femur has become the standard method of treatment for most subtrochanteric femur fractures. Contemporary femoral nails are categorized by their screw orientation and nail design. Standard antegrade femoral nails have a radius of curvature or anterior bow to facilitate its insertion into the femoral canal. Their proximal screw insertion pattern is either transverse or oblique and directed from the greater to the lesser trochanter. Reconstruction nails are similar to standard antegrade nails but are reinforced proximally to accommodate large oblique interlocking screws that are directed into the femoral head. Currently, nails are labeled as piriformis or trochanteric entry nails. Distally, interlocking screw insertion can be performed transversely from lateral to medial or are multidirectional. Either combination can be utilized for reconstruction nailing of subtrochanteric fractures. With these options, a full-length statically locked reconstruction nail of sufficient diameter can be utilized to treat fractures extending from the greater trochanter to the distal femoral metaphysis.
INDICATIONS AND CONTRAINDICATIONS
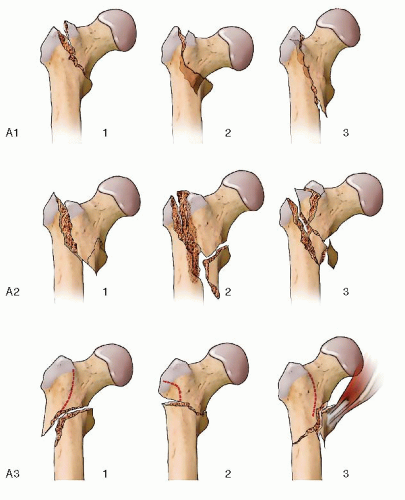
The OTA/AO fracture classification describes subtrochanteric fractures as 31-A (1) (Fig. 21.1). This subgroup of fractures includes intertrochanteric, pertrochanteric, and subtrochanteric, which can be confusing because of conflicting terminology and regional differences. For this reason, Russell and Taylor based their classification on the integrity or compromise of the greater trochanter/piriformis fossa region and the lesser trochanter/medial calcar region (2) (Fig. 21.2). Not surprisingly, fracture extension into the greater trochanter and piriformis fossa creates problems with nailing and increases the risk of comminution and instability. Fracture extension into the lesser trochanter and medial buttress creates problems with sagittal alignment and varus angulation.
A reconstruction nail can be utilized for virtually all acute subtrochanteric femur fractures. This implant can also be utilized for some ipsilateral femoral neck and shaft fractures. Since the reconstruction nail protects the entire femur, it is an excellent implant to treat a wide variety of fracture types. It can be also used for prophylactic nailing of impending and pathologic femur fractures. With screw(s) directed into the femoral head, a reconstruction nail is often used to treat patients with osteoporotic femoral shaft fractures who may be at risk for a femoral neck fracture around their nail should another fall occur. It is also useful in treating atypical (bisphosphonate) femoral fractures (3, 4 and 5). The implant can be inserted through a trochanteric entry site for selected proximal femoral fractures in adolescents. Reconstruction nails are useful in the treatment of malunions, nonunions, and failed plate fixation of selected proximal femur fractures. Whenever possible, closed nailing is preferred over an open procedure to decrease the risk of infection and improve healing. However, the goals of fracture reduction with proper alignment and healing are more important than nailing technique.
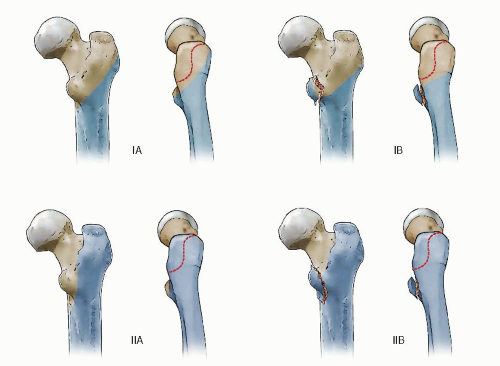 FIGURE 21.2 Components of the Russell-Taylor IB subtrochanteric pattern with greater trochanter intact and lesser trochanteric fracture. |
There are several contraindications to nailing of subtrochanteric fractures. The first and foremost contraindication is surgeon skill. These are complex injuries and there is long learning curve that must be mastered for successful nailing. Significant comminution and displacement of the greater trochanter or fracture extension into the femoral neck are relative contraindications to nailing. A preexisting femoral diaphyseal deformity, femoral implant, or stemmed total knee arthroplasty are also contraindications to nailing.
PREOPERATIVE PLANNING
Subtrochanteric fractures occur with a bimodal frequency (6). Young adults usually sustain high-energy fractures with associated injuries and fracture patterns. Older elderly patients sustain lower-energy fractures with falls through osteoporotic bone. A patient with a femur fracture following high-energy trauma mandates a thorough trauma evaluation for other life- or limb-threatening injuries. Subtrochanteric fractures usually present with a limb shortening, external rotation, and pain. The proximal femur is exquisitely tender, and any motion in the limb is painful. Fortunately, nerve and vascular injuries are uncommon.
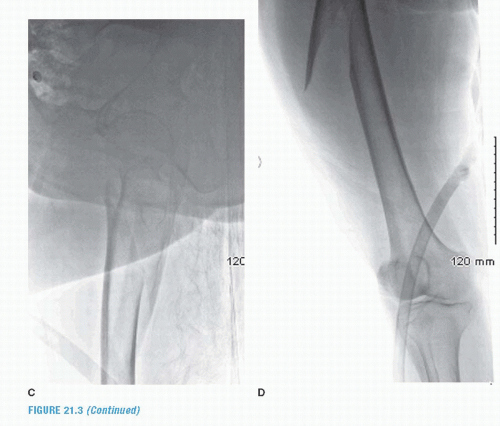
Preoperative imaging consists of a low anterior-posterior (AP) radiograph of the pelvis and AP and lateral radiographs of the hip (Fig. 21.3). The entire femur must be imaged to evaluate for preexisting deformities, retained hardware, or a distal prosthesis that could impede intramedullary nailing. We often obtain contralateral femoral radiographs to serve as a template for neck-shaft angulation, neck-shaft transition, medullary diameter, anterior femoral bow, and limb length. This is especially important when there is comminution or bone loss. Furthermore, in some small stature people and races, nail insertion may be impossible secondary to a relatively short neck-shaft transition, short neck width, and small medullary diameter. Traction radiographs are obtained with gentle and gradual traction of the limb in a neutral rotation. These radiographs are helpful to evaluate the fracture morphology, pattern, and extent. In the past, oblique radiographs have been used to evaluate the femoral neck but have been replaced by computed tomography (CT) imaging. CT scans with axial, coronal, sagittal reconstruction are the best modality to evaluate the femoral neck, piriformis fossa, and greater trochanteric anatomy (Fig. 21.4). It is best performed with some traction and the leg in neutral rotation. Fracture extension into the piriformis fossa and/or greater trochanter with a coronal split complicates femoral nailing. If the
integrity of the proximal femoral canal is compromised, the stability of the nailing construct may be impaired. Therefore, an open or semiopen nailing technique may be required for reduction and subsequent nailing. Alternatively, a periarticular proximal femoral-locking plate may be indicated.
integrity of the proximal femoral canal is compromised, the stability of the nailing construct may be impaired. Therefore, an open or semiopen nailing technique may be required for reduction and subsequent nailing. Alternatively, a periarticular proximal femoral-locking plate may be indicated.
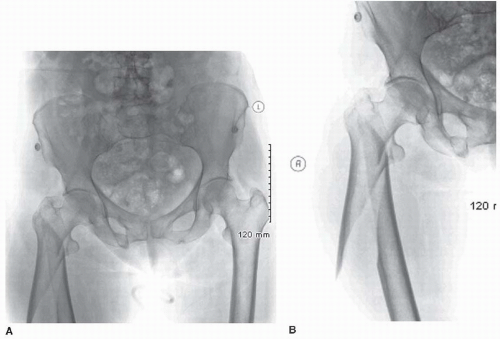 FIGURE 21.3 Injury radiographs of AP pelvis (A), AP hip (B), Lat hip (C), and AP femur (D) of subtrochanteric femoral fracture in 63-year-old female after a low-energy fall. |
For most patients, fixation within 24 hours of admission is necessary because of pain, continued blood loss, risk of deep vein thrombosis, and pressure sores. Patients should be aggressively resuscitated, have routine blood chemistries, and be typed and cross-matched for surgery. A metabolic panel including calcium, vitamin D, parathyroid, and thyroid stimulating hormone should be obtained in elderly patients with lower-energy fractures. Deep vein thrombosis prophylaxis with sequential compression devices and/or chemical methods should be initiated postoperatively. Depending on the fracture pattern, associated injuries, and surgeon preference, traction should be started to maintain length and reduce blood loss and reduce pain.
PERIOPERATIVE EVALUATION
Nail selection is dependent on surgeon experience, fracture pattern, proximal femoral geometry, and femoral diaphyseal anatomy. Inexperience, failure to understand the deforming forces, and inadequate imaging studies greatly increase the chance of fracture malreduction. Some ethnicities and races of small stature have relatively narrow femoral necks, short neck-shaft transition, and small medullary canals, making reconstruction nailing very difficult or impossible. If the fracture anatomy is not clear, contralateral femoral radiographs may help with preoperative planning, measurements, and templating.
Reconstruction nails are available in many lengths and diameters (Fig. 21.5). Depending on the manufacture, the nail has the ability to be utilized in left or right femurs only or interchangeably for both left and right based on the screw configuration proximally. Most reconstruction type nails are expanded or thickened in the upper end to accommodate the proximal screws and high mechanical forces in the proximal femur. The transition from the thickened proximal portion to the diaphyseal portion is variable depending on the manufacturers. Trochanteric entry nails typically have a 4 to 10 degrees bend or angulation in the coronal plane compared to standard reconstruction nails that are designed for piriformis fossa entry and have no angulation. The proximal interlocking screws are usually angled anteriorly (8 to 15 degrees) to accommodate the anteversion of the femoral neck and cephalad (120 to 135 degrees) to accommodate the neck-shaft angulation. Despite the nail anteversion, excessive posterior nail entry can compromise screw insertion into the femoral neck and head. Failure to restore the normal neck-shaft angle can severely compromise screw insertion into the femoral head. Proximal screw size varies from 5.0 to 8.0 mm and spread is 1.5 to 2 cm. With varus reductions or atypical anatomy, screw insertion can be suboptimal or impossible. The proximal screws are either partially or fully threaded. Only full-length femoral nails should be utilized to distribute force from proximal to distal and protect the entire femur in elderly osteoporotic bone. In younger patients with more comminuted fracture patterns, larger diameter nails are recommended. For older more osteoporotic fractures, nail diameter has to be tailored to the patient’s anatomy to avoid distal cortical penetration. In these situations, I prefer nails with a smaller anatomic radius of curvature or smaller nail diameters (<11 mm) that allow for more central nail position distally and lessen the risk of the anterior cortex penetration. Because of inherent fracture instability, all reconstruction nails should be locked distally with either one or two screws.
Secondary to the proximal deforming forces, devices that realign the proximal femur in both the sagittal and coronal planes are beneficial (Fig. 21.6). Large and small tenaculum clamps (Weber Clamp, large
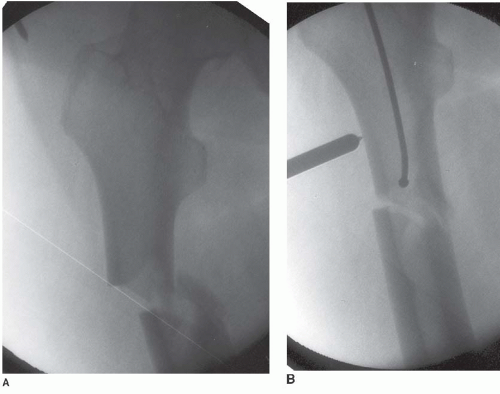
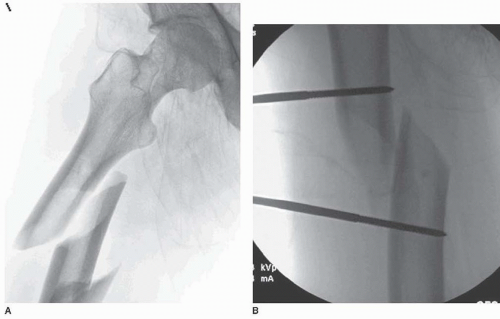
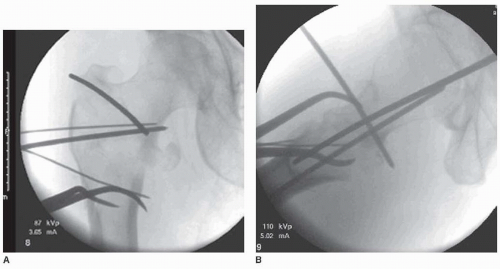
and small, 1 to 2 each) can be inserted through small strategically applied incisions directly over the fracture site to anatomically reduce spiral fractures or translate transversely oriented fractures (Fig. 21.7). Ball-tipped spike pushers (3,7) can translate and reduce large fracture fragments (Fig. 21.8). Schantz pins (2.5 and/or 5.0 mm) inserted percutaneously or openly can help realign, reduce, translate, and derotate fracture fragments. The Schantz pins can be inserted in a bicortical fashion temporarily for the initial reduction maneuver and then converted to a unicortical position after the ball-tipped guide wire has been inserted (Fig. 21.9). Anterior to posteriorly directed Schantz pins can act as pollar-blocking pins to narrow the metaphysis and correctly direct reaming and subsequent nail insertion. Kirschner wire insertion (0.62 mm) anteriorly or posteriorly to the entry portal proximally can aid in reconstruction of complex, multiplanar fracture patterns, and solidify a tubular construct proximally for reaming and nailing without displacing the fracture (Fig. 21.10).
and small, 1 to 2 each) can be inserted through small strategically applied incisions directly over the fracture site to anatomically reduce spiral fractures or translate transversely oriented fractures (Fig. 21.7). Ball-tipped spike pushers (3,7) can translate and reduce large fracture fragments (Fig. 21.8). Schantz pins (2.5 and/or 5.0 mm) inserted percutaneously or openly can help realign, reduce, translate, and derotate fracture fragments. The Schantz pins can be inserted in a bicortical fashion temporarily for the initial reduction maneuver and then converted to a unicortical position after the ball-tipped guide wire has been inserted (Fig. 21.9). Anterior to posteriorly directed Schantz pins can act as pollar-blocking pins to narrow the metaphysis and correctly direct reaming and subsequent nail insertion. Kirschner wire insertion (0.62 mm) anteriorly or posteriorly to the entry portal proximally can aid in reconstruction of complex, multiplanar fracture patterns, and solidify a tubular construct proximally for reaming and nailing without displacing the fracture (Fig. 21.10).
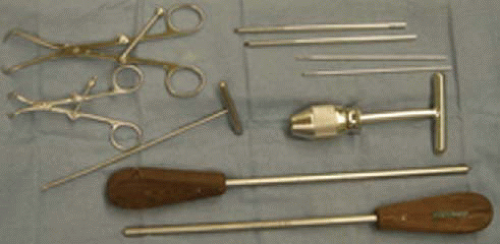 FIGURE 21.6 Assistive reduction devices for proximal femoral fracture reduction: small and large Weber clamp, 2.5- and 5.0-mm Schantz pins, Shoulder Hook, Universal Chuck, and Ball-Tip Spike Pusher. |
PATIENT POSITIONING
The patient can be positioned either supine or lateral on a fracture table. The supine position is more common since it is familiar to surgeons and staff, and patient positioning is faster and the fracture reduction may be improved (Fig. 21.11). Furthermore, the supine positioning facilitates intraoperative visualization of the proximal femur with the C-arm, which is critical for successful fracture reduction and nailing (Fig. 21.12). The disadvantage of the supine position is longitudinal traction on the extended limb often exacerbates multiplane proximal femoral fracture deformity. Some of these difficulties can be overcome by lateral nailing on a fracture table. However, the lateral position is less familiar to younger surgeons and OR staff. It also requires different equipment to accommodate the patient and extremities while on the fracture table.
Intraoperative traction can be accomplished with a boot or skeletal pin traction. Boot traction can be performed in the majority of patients if surgery is performed within the first 48 hours. If surgery is further delayed, skeletal traction may be necessary to restore leg length. If this is required, the traction should be periodically reduced or released during the case to minimize the risk of a pudendal or sciatic nerve injury. The use of paralyzing agents during surgery also facilitates fracture reduction. Intraoperative or manual traction on a regular operating room table is not recommended due to the difficulty of consistently restoring length with this method and the need for a dedicated leg holder or skilled assistant. In a small percentage of patients with high-energy trauma, particularly those with a “dashboard” mechanism of injury, an occult knee ligament injury may be present. Therefore, in a patient with a painful swollen knee, skeletal traction through a distal femoral pin may be a safer alternative until the knee injury is better clarified.
High-quality AP and lateral radiographs of the hip, with the patient on the fracture table, are essential to determine the fracture reduction and femoral neck anteversion angle. Usually, the x-ray beam has to be angled about
10 to 25 degrees from the floor to obtain a true lateral view. AP visualization may require a slight rollover and cephalad tilt of the beam to accommodate the neck flexion and abduction. The monitor should be placed at the end of the fracture table so that both surgeon and fluoroscopy technician can easily see the screen. If the patient is lateral on the fracture table, AP visualization is accomplished with the beam parallel to the floor while the lateral image is obtained with the beam upright but tilted cephalad 30 to 45 degrees to better visualize the femoral neck.
10 to 25 degrees from the floor to obtain a true lateral view. AP visualization may require a slight rollover and cephalad tilt of the beam to accommodate the neck flexion and abduction. The monitor should be placed at the end of the fracture table so that both surgeon and fluoroscopy technician can easily see the screen. If the patient is lateral on the fracture table, AP visualization is accomplished with the beam parallel to the floor while the lateral image is obtained with the beam upright but tilted cephalad 30 to 45 degrees to better visualize the femoral neck.
The opposite uninjured leg is a good template to assess limb rotation, length, and alignment preoperatively. In the supine position, the fracture should be reduced as well as possible before beginning the procedure. First, externally rotate (not internally rotate as with intertrochanteric fractures) the secured limb through the boot holder. Second, apply traction through the peroneal post and foot piece. Third, flex the foot traction device about 15 to 20 degrees. Fourth, provide about 10 to 15 degrees of adduction to improve nail insertion trajectory. Once the above steps are performed, begin fluoroscopic assessment of the reduction and provide small incremental changes in the above parameters to “fine-tune” the reduction. The contralateral leg can be positioned in a scissored or hemilithotomy position. Scissoring can accommodate longer procedures but can interfere with lateral visualization. Hemilithotomy positioning facilitates lateral visualization but may be of concern with extended length cases (increased compartmental pressures) and patients with limited hip motion. With either method, persistent intraoperative monitoring of the uninvolved leg for pressure areas and compartments is necessary.
A cephalosporin antibiotic is administered intravenously within 1 hour of skin incision and continued for 24 to 48 hours postoperatively. The prep and drape must extend from the ipsilateral lower chest wall to the midcalf. Following irrigation and débridement of open fractures, I routinely reprep and drape.
FRACTURE REDUCTION
Whenever possible, fracture reduction should be performed and confirmed fluoroscopically before the surgical incisions are made. Since the fracture may be in relative flexion initially, reduction of the flexion redirects the skin incision anteriorly and aids in proper entry site selection. Remember that correct fracture reduction requires restoration of length, rotation, and alignment in both coronal and sagittal planes (Fig. 21.13). AP, lateral, and oblique (roll over or roll under) images will assist in the assessment of fracture reduction.
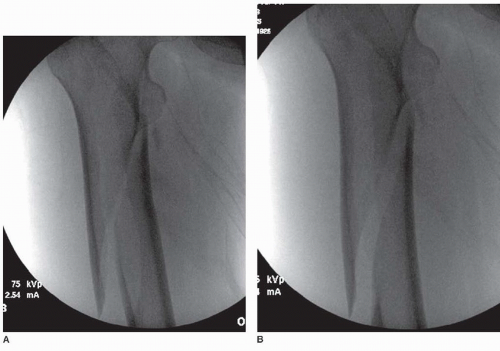
When the fracture is persistently flexed and in varus, the proximal segment should be reduced with either a ball-tipped spike pusher or Schantz pin placed through a small skin incision. Usually, this will be performed through a small anterolateral incision that counters the flexion and abduction yet is out of the plane of image intensifier. With the fracture aligned, the entry site should be more easily obtained by bringing the trochanter and piriformis fossa more in line with the axis of the femoral shaft. For spiral fracture patterns, a combination of both a ball spike pusher and Weber tenaculum clamps can efficiently reduce and maintain the fracture reduction (8). Again, through a 3- to 4-cm anterolateral incision, spread the vastus in line with its fibers and insert the Weber clamp (i.e., perpendicular to the diaphysis in both planes). Once the location of the fracture is confirmed on fluoroscopy, the clamp is opened enough to slide it over the cortex and then closed to reduce the fracture (Fig. 21.14). Loosening the footplate prior to tightly clamping the fracture often helps to improve rotational alignment before final tightening. If the fracture does not reduce, it is usually malrotated or flexed, which is
best seen on the lateral view (Fig. 21.15). Utilizing a ball spike pusher (anteriorly to posteriorly) on the flexed proximal segment with the fracture reapproximated but not compressed often facilitates translation of the flexed proximal segment allowing reduction (Fig. 21.16).
best seen on the lateral view (Fig. 21.15). Utilizing a ball spike pusher (anteriorly to posteriorly) on the flexed proximal segment with the fracture reapproximated but not compressed often facilitates translation of the flexed proximal segment allowing reduction (Fig. 21.16).
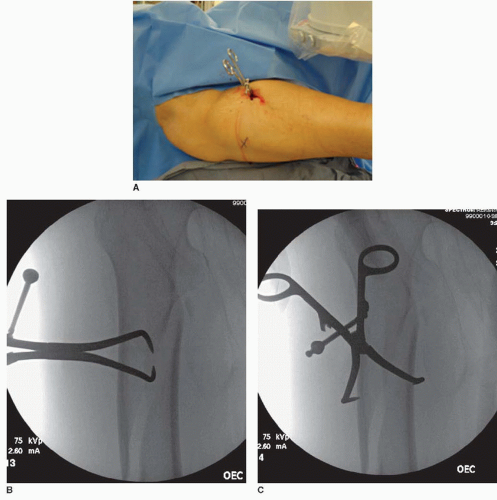 FIGURE 21.14 For a spiral fracture pattern, a 4-cm incision is created, and a large Weber clamp is inserted parallel to the muscle fibers done to the bone (A). Once against the bone and parallel to the fracture plane, the clamp is rotated 90 degrees (B), slided alongside the bone, and compresses the fracture utilizing the tines only (C).
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|