Fig. 9.1
Approximate phases of healing. Acute (0–6 days), sub-acute (3–21 days), and chronic (> 21 days)
During the sub-acute phase, growth and regeneration take place primarily through angiogenesis intermixed with collagen formation. This is stimulated by multiple growth factors including vascular endothelial growth factor (VEGF), platelet derived growth factor (PDGF), and fibroblast growth factor (FGF; Table 9.1). While this process is an integral part to overall healing, it can also result in scar tissue formation or prolong the overall healing process [1, 3]. Therapies should be aimed at reducing such effects while maximizing the benefits of the sub-acute phase of healing.
Table 9.1
Function of growth factors involved in sub-acute healing phase
Growth factor | Functions |
|---|---|
VEGF | Growth of new blood vessels |
PDGF | Migration and proliferation of fibroblasts and smooth muscle cells |
FGF | Growth of new blood vessels |
Endothelial cell migration in damaged tissues | |
Skeletal muscle development | |
TGF-β (beta) | Stimulates fibroblast chemotaxis |
Enhances collagen production | |
Strong anti-inflammatory effect |
Defining Chronic
Chronic injury can be defined both quantitatively and histologically. These injuries involve a prolonged course of repair and regeneration when compared to sub-acute injury. This consists of continued satellite cell differentiation, type I collagen production, and fibroblast proliferation [4]. Typically, chronic injuries are the result of maladaptive patterns of regeneration and repair resulting in persistent inflammation and decreased function [5]. This can be exacerbated by severity of injury, overuse, or premature return to previous level of activity. For those interested in additional detail on the pathophysiology of skeletal muscle injury and the phases of healing, an extensive review can be found in Chap. 4.
Gastrocnemius
Gastrocnemius muscle injuries occur most frequently in middle-aged or older adults, although these injuries will also afflict younger athletes. Most vulnerable are those who participate in one of the following sports: running, basketball, football, skiing, and racquet sports [6]. Biomechanically, the most common mechanism of injury is caused by a sudden knee extension while the foot is already dorsiflexed [7, 8]. The location of injury within the gastrocnemius is primarily the medial head at the myotendinous junction (MTJ). This region is considered the weakest part of the muscle–tendon complex [9]. The medial head also has a prolonged attachment, which may provide stronger forces than the lateral head of the gastrocnemius [8].
Most sub-acute gastrocnemius strains will be evident by history and physical exam. Patients will usually recall a single event antecedent to symptom onset, although occasionally, the event is either forgotten or was overshadowed by distracting events such as sport participation. When prompted, the patient may be able to localize the site of pain at onset to the medial calf, or they may report vague posterior leg pain.
Examination sequence is similar to other orthopedic injuries: inspect for swelling, ecchymosis, or deformity. The examiner should then palpate carefully for a single or broad-based tender location. A palpable defect should be sought as well. The novice must be cautioned, as sometimes a normal myotendinous junction may be interpreted as being defective. Examining the contralateral leg can provide comparison. The examiner may also ask the patient to provide a plantar flexion force against resistance (i.e., the examiner’s hand) to elicit pain or a noticeable defect. Inspection and palpation can also be performed with the patient standing, followed by heel-rise efforts if tolerated.
Imaging typically is not required to make the diagnosis. However, the elite athlete may benefit from magnetic resonance imaging (MRI) or ultrasound examination to gain additional information on prognosis and healing. Imaging is also useful to help exclude other causes of calf pain, which include thrombophlebitis, compartment syndrome, ruptured popliteal cyst, or plantaris rupture [8]. Diffuse swelling to the lower leg may also prompt the clinician to consider deep vein thrombosis (DVT). If diagnostic imaging is needed, the two primary methods include MRI and ultrasound; however, MRI is preferred for sub-acute injuries due to increased visibility of muscle injuries [8]. In particular, T1-weighted images are beneficial in the assessment of sub-acute hemorrhage associated with gastrocnemius strains [8]. MRI is also superior to ultrasound in sensitivity regarding follow-up of healing injuries due to increased resolution. Repeat imaging can be used to evaluate severity and the time course of injury. MRI can be used to determine prognosis by measuring the longitudinal length of muscle injury, which correlates to time lost from injury [9]. Severity of injury is determined by the severity of intramuscular edema, hemorrhage, and fiber injury, which in turn will also affect prognosis [8]. Ultrasound may be more favorable than MRI when cost and convenience are taken into account. Thus, ultrasound may be preferable if repeat examinations are planned to evaluate the ongoing healing process. Observation of remaining fluid collection may serve as an additional prognostic determinate in overall healing [10] (Fig. 9.2).
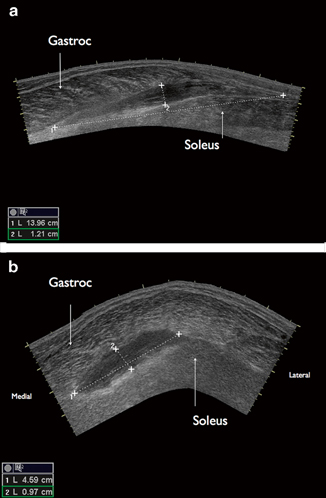
Fig. 9.2
a Ultrasound image, sagittal orientation. Hematoma in tissue plane dissecting gastroc muscle from the soleus muscle. b Ultrasound image, axial orientation. Hematoma in tissue plane dissecting gastroc muscle from the soleus muscle
For many patients, full recovery from muscle injury in the posterior leg may take up to several months before returning to previous pain-free activity level [10]. However, the sub-acute phase of injury begins long before then, and treatment choices can affect the extent and timing of recovery. Treatments aimed at the sub-acute phase are discussed at the end of the chapter and detailed in other chapters in this book.
Soleus
The soleus muscle is positioned deep to the gastroc. In considering primary muscle injuries it is largely ignored because until recently the soleus was thought rarely to get injured [11]. Several factors contribute to neglecting this muscle. Clinically an injury to the gastroc garnishes all the attention due to the dramatic presentation and frequency of occurrence, while a concomitant or isolated soleus injury is subtle and often goes unnoticed. Imaging studies may also underreport soleus injuries. Ultrasonography , although an excellent diagnostic tool, is very operator dependent, and an inexperienced examiner without a high index of suspicion may overlook an injury to the soleus. In addition, the deeper location of the soleus makes evaluation with ultrasound more difficult. Finally, the soleus is made up of predominately Type I (slow-twitch) fibers, a muscle type not typically associated with muscle strains . Consequently, soleus strain is thought unlikely and not commonly considered when patients have posterior leg pain. Despite these reasons for neglecting the soleus, it is an important injury to consider in the patient with sub-acute or chronic posterior leg pain, particularly if provoked by repetitive activity.
Injuries to the soleus can occur in various locations throughout the muscle. The two areas most affected are the musculotendinous junction and the myofascial junction. Musculotendinous junction strains are more common and occur at the distal intramuscular tendon or the proximal medial and lateral aponeuroses. The locations of the medial and lateral aponeuroses are just distal to the muscle origin, on the posterior tibia and fibula, respectively. The two pennate structures merge centrally to form the intramuscular central tendon as they move distally toward the Achilles tendon. Strains occurring away from the tendons are considered myofascial. Primarily, this occurs at the myofascial junction with the gastrocnemius or at the junction of the posterior compartment of the leg [11] (Fig. 9.3).
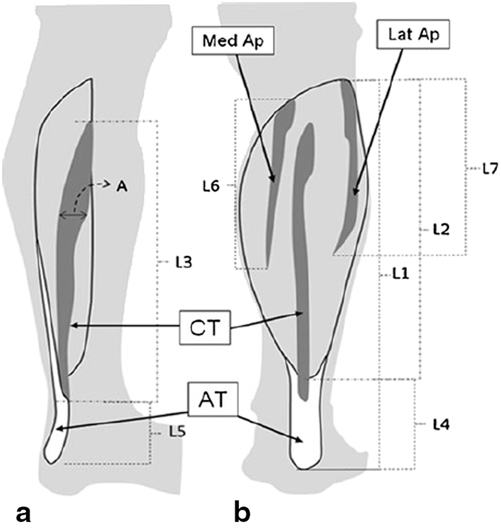
Fig. 9.3
a Sagittal view facing medial aspect of calf. b Posterior coronal view. CT Central tendon, AT Achilles tendon, Med Ap Medial aponeurosis, Lat Ap Lateral aponeurosis (Common location of plantaris strain in bold). (From [11]. Reprinted with permission from Springer Science + Business Media)
History and physical exam help to differentiate a soleus injury from a gastrocnemius injury . Soleus injury occurs during low-impact activity such as walking or jogging. Frequently, a sentinel event is lacking. Typical presentation symptoms include: calf tightness, stiffness, and worsening pain over the course of several days [7]. Palpitation of the various aponeuroses, along with flexing the knee during examination, may help illicit more objective findings. Knee flexion eliminates the confounding influence of the gastroc. If deemed clinically necessary, imaging with ultrasound or MRI can clarify diagnostic uncertainty. Due to the deeper location of the soleus, MRI is considered superior to ultrasound for determining degree of injury [11].
There is a paucity of literature regarding the treatment of soleus injury. This is likely due to the decreased frequency of soleus injury relative to gastrocnemius injuries and the challenges in diagnosing soleus injuries. This injury may also be underappreciated in current clinical practice because symptoms can often resemble that of delayed-onset muscle soreness [11]. However, these injuries should benefit from a similar treatment approach used for gastrocnemius injury described below.
Plantaris
The plantaris is an accessory muscle working in conjunction with the soleus and gastrocnemius muscles to provide a minimal amount of plantar flexion of the calf. The muscle belly itself is small, while the tendon is one of the largest in the body [12]. The plantaris muscle is absent in 7–10 % of the population [13, 14]. The plantaris muscle originates on the superior posterior aspect of the lateral femoral condyle, just medial to the lateral head of the gastrocnemius. The muscle belly of the plantaris travels from this origin, in an inferior obliquely medial direction extending an average 10 cm. The muscle belly then gives way to a long slender tendon whose course extends between the medial head of the gastrocnemius and soleus eventually accompanying the Achilles tendon to insert on the medial aspect of the calcaneus.
Injuries to the plantaris are often overlooked. Historically, prior to soft tissue imaging techniques such as MRI or ultrasound, surgical exploration was necessary to prove plantaris tendon rupture. Since imaging is not commonly performed in posterior leg muscle injuries, the true incidence of plantaris rupture is unknown. Further impairing incidence data, clinical suspicion of plantaris muscle injury can be delayed because strains of the muscle may lack a sentinel traumatic event. Plantaris injuries can occur in isolation or as a component of multiple tissue traumas accompanying an anterior cruciate ligament (ACL) tear, lateral compartment bone contusion , or arcuate ligament injury [14].
The evaluation of plantaris injuries begins with a thorough history. The clinician may need to assist the patient to recall symptom onset, acute or insidious, mechanism of injury and early clinical symptoms. Like gastrocnemius injuries, the mechanism usually combines forcibly extending the knee on a fixed dorsiflexed ankle. This history can understandably lead to misdiagnosis of plantaris injury as a strain to the medial head of the gastrocnemius [15]. This may be exacerbated by patient history that includes an inciting event with audible “pop” sensation. The clinician may expect the history to include pain; however, Allard describes two patients whose primary complaint consisted of vague muscle soreness and a cramping sensation [16]. Likewise, in the right clinical setting a differential diagnosis must also consider DVT .
Physical examination for a suspected plantaris rupture is frustratingly nonspecific. Pertinent physical findings consist of swelling in the posterior medial upper calf. This is in distinction to the medial head gastroc tear that usually occurs at the myotendinous junction. A tender, palpable mass can sometimes be appreciated just below the popliteal fossa. Visible hemorrhage may or may not be present. Full range of motion at the ankle and knee are possible. A false positive Homans’ sign for DVT is also possible [16].
Imaging is not usually necessary or indicated to confirm a plantaris muscle or tendon tear. However, imaging is indicated for diagnostic clarification when DVT or neoplasm is considered. Characteristics of plantaris tear on MRI include a fluid presence interspersed between the gastroc and soleus [16]. This is in distinction to intramuscular edema seen with gastroc or soleus muscle strain. Although a concomitant gastroc strain is possible, an isointense gastroc and soleus muscles is typical, thereby assisting to differentiate this mass from neoplasm. A retracted muscle belly is seen with complete ruptures at the myotendinous junction.
MRI or ultrasonography is the modality of choice for imaging. The plantaris tendon is an avascular structure, so imaging displays an isointense mass between the gastrocnemius and soleus muscles [14, 16].
Ultrasonography provides a less costly alternative to MRI for assessment of plantaris injuries. Advancements in ultrasound have led to greatly improved resolution. Interpretation and assessment is operator dependent. Fluid collections between the gastroc and soleus are easily appreciated by ultrasound. Ultrasonography also offers the opportunity to simultaneously assess the leg for DVT.
Treatment for plantaris injury is conservative. Management will be similar to gastrocnemius strain, often because the clinician is not initially thinking of possible injury to the plantaris muscle. Rest, ice, and nonsteroidal anti-inflammatory drugs (NSAIDs) are the modalities recommended. There has not been documented treatment with other therapeutic measures; however, those listed below may have benefits. Surgery is not necessary for confirmation of injury or treatment [16]. Although, surgery performed for diagnostic clarification has been done [15] (Table 9.2) .
Table 9.2
Comparison of posterior lower limb muscular injuries
Plantaris tendon tear | Soleus injury | Gastrocnemius strain | |
|---|---|---|---|
History | Acute popping (+/−) | Ache | Explosive activity |
Insidious soreness, swelling, cramping | Worsening pain over days | Progressive swelling, pain | |
Calf tightness, stiffness | |||
Physical | Associated knee pathology | Medial, lateral, or distal calf pain | Medial calf tenderness |
Imaging | US or MRI | MRI preferred, US | US or MRI |
Severe/Prolonged or Delayed Recovery of Muscle Injuries in the Posterior Leg
Resolution of injuries to the posterior lower leg musculature depends on several factors. Most notably, the severity of muscle strain may dictate a prolonged course toward recovery. Strains are typically graded I–III to outline severity. Grade I strains involve partial muscle tears with no identifiable loss of muscle integrity. Grade II strains involve anywhere from 10 to 50 % muscle disruption, while grade III muscle strains involve at least 50 % loss of muscle integrity [17]. These more severe injuries in turn require a prolonged rehabilitative process and healing time. A variety of factors (premature return to play, poor treatment protocol, and delay in injury detection) may prolong healing and result in maladaptive restoration and chronic injury. This in turn increases scar tissue formation and tissue disorganization altering muscle function. Consequently, the muscle becomes dysfunctional and a source of chronic pain.
In severe strains, patients may require a period of non-weight bearing and immobilization until the muscle heals enough to tolerate ambulation. However, injuries that have reached the chronic phase are usually unresponsive to rest and will exhibit pain and weakness that limit function on resumption of activity. Therefore, treatments emphasizing restoration of structure and function are generally recommended for chronic strains. Eccentric exercises may be beneficial as they promote strengthening of passive tissue elements and have proven useful in chronic muscle tendinopathy [18]. Other treatments such as platelet-rich plasma (PRP) may provide chemokines and growth factors at a cellular level to create a local milieu to promote healing. Proprioceptive exercises along with biomechanical correction may help reduce symptoms and prevent or delay injury recurrence. Soft tissue mobilization and manual therapy techniques may reduce tissue adhesions, improve tissue organization, and stimulate a local healing response [19, 20].
Calcific Gastrocnemius Tendonitis
Calcific tendonitis has been observed as a cause of chronic posterior leg pain in few case reports dating back as early as 1981. This condition is primarily observed in the elderly. While calcium pyrophosphate dihydrate (CPPD) crystals are a relatively common finding in the gastrocnemius (incidence as high as 32 % in patients with average age of 72), associated tendonitis is a rare cause of chronic pain [21]. In the case reports, the condition affected elderly women and symptoms included posterior knee pain with decreased knee flexion. Initial workup included plain radiographs followed by computed tomography (CT) and/or MRI. Patients responded to treatments including repeated local corticosteroid injection or surgical decompression after failed conservative management [21]. Newer minimally invasive techniques such as ultrasound-guided tenotomy may prove beneficial but as yet are unsubstantiated in the literature.
Chronic Exertional Compartment Syndrome
The lower extremity is comprised of four compartments including the anterior, lateral, superficial posterior, and deep posterior compartments . The gastrocnemius, soleus, and sural nerve make up the superficial posterior compartment. The deep posterior is made up of the flexor hallucis longus, flexor digitorum, tibialis posterior , posterior tibial nerve, and posterior tibial artery and vein. The deep posterior compartment is the most common cause of posterior compartment syndrome making up 45 % of all chronic exertional compartment syndrome (CECS) in the posterior lower extremity [22]. CECS occurs when increasing physical activity results in elevated intra-compartment pressures causing reduced regional blood flow to affected muscles. Poor flow in turn causes symptoms of ischemia, which include pain, paresthesias, cramping, and weakness. This condition is commonly seen in athletes (especially runners) under the age of 30 years affecting both males and females equally.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








