Structural Allografts for Acetabular Revision
Mansour Abolghasemian
David Backstein
Oleg Safir
Allan E. Gross
Case Presentation
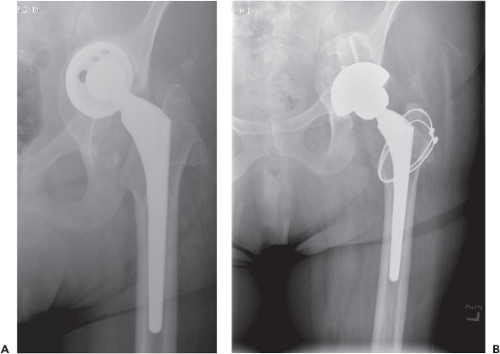
A 30-year-old patient presented with pain 10 years following a total hip arthroplasty performed as part of treatment of a chondrosarcoma. Plain radiographs (Fig. 111.1) show a loose roof ring, with severe bone loss and acetabular protrusio. Revision surgery was planned and given the patient’s young age, consideration was given for a structural allograft to restore bone stock.
Managing bone loss is the most challenging part of acetabular revision surgery. The surgeon faces some degree of bone loss in any revision surgery due to the bone removed at the time of primary arthroplasty, stress-shielding, osteolysis, and possible bone loss at the time of revision surgery (1).
Preoperative Evaluation
After the decision to proceed to revision surgery is made, the severity of bone loss should be estimated. For an orthopedic surgeon who is not comfortable with more complex revision surgeries, the ability to identify more challenging cases can assist identifying cases that should be referred to a revision center. For the revision surgeon, it is likewise crucial to understand the pattern of bone loss so that appropriate instruments, implants, and bone allograft are available for the surgery. We have been using our classification for acetabular bone defects for 19 years (2). This classification is based on preoperative radiologic and intraoperative findings. Table 111.1 presents this classification. This is an easy classification to remember and its validity has been confirmed (2,3). It also provides treatment guidelines especially during the surgery.
Radiologic Evaluation
The radiologic investigation is mainly based on plain radiographs in AP and lateral views. To better evaluate the posterior and anterior columns, iliac and obturator oblique views could be considered. We examine the integrity of the medial wall and presence of protrusio acetabuli (indicating cavitary medial bone loss) in the AP view using standard guidelines (4). As a general principle, a loose implant tends to displace into the deficient part of the acetabulum. Because of the normal anteversion of the acetabulum, posterior column defects
cause the implant to migrate laterally and anterior column defects cause it to migrate medially in an AP pelvis radiograph. Medial migration of the old implant implies a medial wall deficiency (type II) that is usually associated with an anterior wall defect if Kohler line is crossed. A limited anterior wall defect usually does not interfere with the stability of an uncemented cup if the inferior rim of the acetabulum (the bottom part of the tear drop) remains intact, since 3/4 of the acetabular periphery will still be supportive. They can be considered type II defects.
cause the implant to migrate laterally and anterior column defects cause it to migrate medially in an AP pelvis radiograph. Medial migration of the old implant implies a medial wall deficiency (type II) that is usually associated with an anterior wall defect if Kohler line is crossed. A limited anterior wall defect usually does not interfere with the stability of an uncemented cup if the inferior rim of the acetabulum (the bottom part of the tear drop) remains intact, since 3/4 of the acetabular periphery will still be supportive. They can be considered type II defects.
Table 111.1 Gross Classification of Acetabular Bone Loss | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
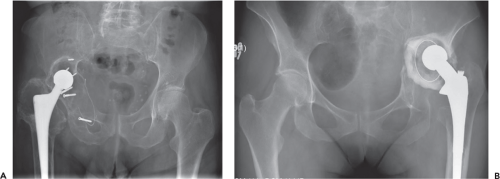
The dome of the acetabulum is also checked. Pure superior or superomedial displacement of the old acetabular component into the dome of the acetabulum with an intact superior rim could be indicative of a contained superior defect (type II) (Fig. 111.2). Any superolateral displacement of the old cup is a sign of superior defect of the acetabular wall, usually associated with some posterior wall deficiency (type III or IV) (Fig. 111.3). A large superior defect that leaves the acetabulum totally unsupportive and causes the component to migrate into the defect is a type IV defect (Fig. 111.4A). Ischial osteolysis signifies posterior column and wall deficiency. Complete disruption of superior and inferior halves of the acetabulum signifies the presence of pelvic discontinuity and a type V defect (Fig. 111.4B). Having these criteria in mind, the surgeon can predict the severity of the bone loss preoperatively. However, the real bone loss is often more severe than what the preoperative radiograph would suggest.
It is often advantageous to perform a CT scan to assess the remaining bone stock more accurately, especially the integrity of the anterior and posterior walls and the thickness of medial wall. This will help the surgeon prepare the requirements for an appropriate surgery. Preoperative imaging studies frequently underestimate the severity of bone loss and the final classification should be performed intraoperatively after the previous component is removed and the
acetabulum is cleaned of granulomatous tissue and debris. Angiography (either conventional or CT-based) is of help when the implant has migrated medially into the pelvis (particularly if such migration occurred acutely or in association with a deep infection) and is felt to be close to the major vessels.
acetabulum is cleaned of granulomatous tissue and debris. Angiography (either conventional or CT-based) is of help when the implant has migrated medially into the pelvis (particularly if such migration occurred acutely or in association with a deep infection) and is felt to be close to the major vessels.
 Figure 111.3. Type III acetabular defect. Twenty years after resection arthroplasty of an infected THA. |
Type I defects are amenable to revision by a standard cemented or preferably uncemented acetabular component. Type II contained defects are usually filled by morselized bone graft and reconstructed using a cemented or an uncemented cup (5). Massive type II defects that do not provide a support for a cup, however, may need more complex reconstructions. Segmental defects as seen in type III or IV should be reconstructed so that the new acetabular component will have enough structural support.
There are two main methods for reconstructing segmental defects, biologic and nonbiologic. Whenever the long-term stability of the construct is dependent on a direct bond of the components to the host bone with ingrowth or ongrowth, the fixation would be considered as biologic. This includes the use of porous-coated implants and porous augments. On the contrary, if the integrity of the construct is not related to the biologic function of the host bone such as when the implants are attached to the host bone through a layer of cement or with screws, the reconstruction would be nonbiologic. Some techniques like impaction grafting and a cemented cup or using roof rings or cages that rely on the fixating screws can be mentioned as examples of nonbiologic methods.
One of the options to achieve implant stability is the use of structural allografts, which are the objective of this chapter. Once being the standard method of treating segmental defects, it is employed much less frequently at the present time. The surgical technique in addition to special facilities needed to prepare the allograft and preserve its sterility and mechanical properties, has limited its use to some specialized centers. The long-term longevity of the graft has been a matter of concern, since resorption of the allograft tissue is a common event (6). The advent of ultra-porous materials, for example, trabecular metal, has introduced an easier technique with theoretical advantages and promising short-term results (7).
The main advantage of using structural allografts is the potential for restoring bone stock while providing structural support for the acetabular implant (8,9). One prerequisite for achieving these advantages is union of the allograft to the host bone. Any condition that hinders union, for example, radiation, should be considered a relative contraindication for using an allograft. Active infection is another contraindication (10). Considering the complexity of the technique of using allografts, severe comorbidities that preclude long surgeries are also considered contraindications for the technique (10).
Surgical Technique
The surgery is done with the patient in the lateral decubitus position. Securing the patient in a true lateral decubitus position is of paramount importance to have a valid reference for positioning the acetabular component during the surgery.
Our preference is to use a lateral approach, although a posterior approach can be equally advantageous. We perform a trochanteric osteotomy whenever anything more than a simple use of an uncemented cup is anticipated (see Chapter 103). After incising the fascia, we identify the posterior border of gluteus medius. The gluteus medius and gluteus minimus muscles are reflected anteriorly to expose the tendon of piriformis muscle. The interval between the gluteal muscles and piriformis is the plane to start the osteotomy. We have used a modified trochanteric osteotomy in the last decade that leaves about 1 cm of the posteromedial part of the greater trochanter attached to the main fragment of the femur. In this way, the whole mass of posterior soft tissue, including the capsule and short external rotators will remain intact. This has markedly decreased our dislocation rate (11).
The length of the osteotomy depends on whether the femoral component is also being revised. The vastus lateralis is left attached distally to the trochanteric fragment regardless of its length. Whenever removing a cemented or a well-fixed uncemented stem is planned, a modified extended trochanteric osteotomy (ETO) is performed (12). However, if only the acetabular component is being revised, or if exposing the femoral canal during revision of the stem is not deemed necessary, a modified trochanteric slide osteotomy is enough (13). In either case, the continuous sling of gluteal muscles and vastus lateralis diminishes the rate of superior migration of the trochanter, should a nonunion occur (Fig. 111.5) (14).
The osteotomy fragment along with the attached muscles is displaced anteriorly and the pseudocapsule of the joint is excised. After removing the old component, the acetabulum is debrided so that the whole rim of the acetabulum is exposed. Usually only minimal reaming is needed to reach bleeding bone. Great caution is encouraged in reaming the medial wall not to perforate the bony wall and violate the pelvic viscera. Whenever in doubt, we use a drill hole and a depth gauge to determine the thickness of the medial wall of which we try to preserve at least 3 to 4 mm. The ultimate classification of the acetabular defect is performed at this point. A trial cup is placed into the acetabulum and the acetabulum is visually divided into four quadrants (Fig. 111.6A). The proportion of uncovered area is assessed for each quadrant and the total uncoverage percentage is calculated. If there is a segmental defect of more than 50% of the acetabular rim, it is considered a major column defect. Smaller defects are considered minor column defect. Presence of a pelvic discontinuity should be meticulously investigated. Apparent integrity of the columns is not enough to rule out a pelvic discontinuity. Using a Cobb elevator, gentle pressure is exerted to the inferior half of the acetabulum. If the inferior segment including ischium moves independent of the superior segment, a pelvic discontinuity is diagnosed.
There is no need for a structural support for defects that constitute up to 30% of the acetabulum. Morselized allograft could be applied to the defect to restore bone stock for rerevisions. However, any defect greater than 30% should be augmented by a structural support (i.e., minor column graft for defects of 30% to 50% and major column graft for defects greater than 50%).
Segmental Defects less than 50% of the Acetabulum (Type III, Minor Column Defect)
The defect is usually superior, either superoanterior or superoposterior. This defect can be the result of a primary dysplastic hip, the combined effect of stress-shielding and osteolysis, and the edge-loading of the acetabular rim by a loose, abducted cup.
In the setting of a type III defect, the trial cup may obtain at least partial stability in spite of the defect. However, several studies have shown that less than 60% to 70% bone coverage of the cup may jeopardize the long-term stability of a cementless cup (15,16). Therefore, it is recommended to fill the defects that are larger than 30% of the acetabulum with a structural support. Structural allograft has been the traditional option. Other options will be discussed later in this chapter.
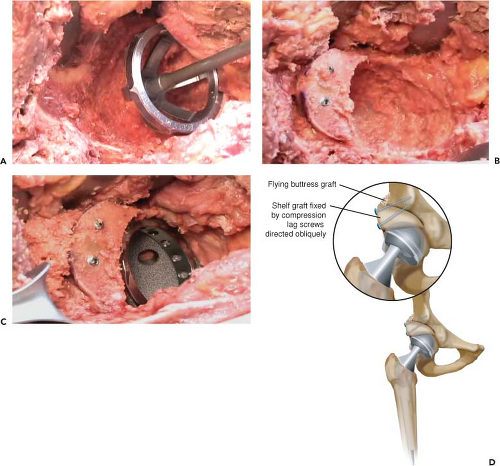
Minor column allografts (also called shelf grafts) can replenish the bone defect for future revisions (8). Because most of the surface of the cementless cup will be in contact with the host bone, the loads will be mostly transferred to the host bone and there is no need to protect the allograft with a cage.
Our preference for a minor column graft has been a femoral head allograft of a young male, but in a large acetabulum, an acetabular allograft might be needed. The allograft is thawed in warm proviodine (betadine) solution while the acetabular preparation is carried out. For a femoral head allograft, a female reamer is used to remove the cartilage but to retain the dense subchondral bone and then it is sculpted to accommodate the allograft to the defect. Intimate contact of the allograft and host bone is important. We prefer to avoid exposing the cancellous part of the allograft to the host soft tissue, since this theoretically results in higher rates of allograft resorption and collapse.
The allograft is then secured to the supra-acetabular bone with two or three 4.5 malleolar or 4 cancellous screws accompanied by washers. The orientation of the screws should be ideally parallel to the joint reaction force direction which is in a coronal oblique plane aiming superomedially. Then, another series of reamings is performed starting with the smallest reamer that engages the introitus, going up to the size selected for the cup, so that the allograft becomes flush with the host bone (Fig. 111.6B). Because the allograft bone is harder than the patient’s own bone, it is very easy to ream eccentrically toward the native parts of
the acetabulum. This should be avoided. Typically no more medial reaming is performed at this stage. The acetabular component is then inserted (Fig. 111.6C,D). Our implant of choice in the revision scenario is a trabecular metal revision cup (Fig. 111.7). When revising a type III acetabulum, it is usually possible to place the cup in the desired abduction and anteversion. Thus, a modular TM cup could be used. Nonetheless, a tantalum revision cup possesses some advantages. The liner is cemented to the cup and can be positioned independent of the cup to compensate for a malpositioned cup. Extra screws can be inserted through the tantalum material in any desired direction and the cement mantle will compensate for the prominence of the screw heads, allowing the liner to be seated. Some morselized reaming autograft is then applied between the allograft and ilium (flying buttress graft) to encourage union (Fig. 111.6D). After revising the implants, the trochanteric fragment is attached to the femur using at least two cerclage wires.
the acetabulum. This should be avoided. Typically no more medial reaming is performed at this stage. The acetabular component is then inserted (Fig. 111.6C,D). Our implant of choice in the revision scenario is a trabecular metal revision cup (Fig. 111.7). When revising a type III acetabulum, it is usually possible to place the cup in the desired abduction and anteversion. Thus, a modular TM cup could be used. Nonetheless, a tantalum revision cup possesses some advantages. The liner is cemented to the cup and can be positioned independent of the cup to compensate for a malpositioned cup. Extra screws can be inserted through the tantalum material in any desired direction and the cement mantle will compensate for the prominence of the screw heads, allowing the liner to be seated. Some morselized reaming autograft is then applied between the allograft and ilium (flying buttress graft) to encourage union (Fig. 111.6D). After revising the implants, the trochanteric fragment is attached to the femur using at least two cerclage wires.