Grade
Pain
Imaging findings
Description
I
No
Imaging evidence of stress fracture, no fracture line
Asymptomatic stress reaction
II
Yes
Imaging evidence of stress fracture, no fracture line
Symptomatic stress reaction
III
Yes
Non-displaced fracture line
Non-displaced fracture
IV
Yes
Displaced fracture
Displaced fracture
V
Yes
Nonunion
Nonunion
Grades I and II injury lack a distinct fracture line. However, they do have imaging evidence of stress reaction (hyperintensity on magnetic resonance imaging T2-weighted and STIR [short-tau inversion recovery], increased uptake on technetium-99m-labeled methylene diphosphonate bone scan [triple phase bone scintigraphy], or cortical thickening and sclerosis on plain radiographs and computed tomography [CT]). The difference between Grade I and II is the absence (Grade I) or presence (Grade II) of symptoms. Visualization of a fracture line on imaging makes the fracture a Grade III or higher. The difference between Grade III and IV is the absence (Grade III) or presence (Grade IV) of fracture displacement. A Grade V injury represents fracture nonunion.
Stress fractures may additionally be dichotomized into “low-risk” and “high-risk” [9]. High-risk stress fractures are those prone to displacement, nonunion, delayed union, and re-fracture. High-risk fractures present a challenging situation, often requiring either surgery or a lengthy duration of nonsurgical management, which, for some competitive athletes, may be potentially career-ending. High-risk fractures include anterior tibial diaphysis, femoral neck tension side, patella tension side, talar neck, proximal fifth metatarsal, central dorsal tarsal navicular, medial malleolus, and hallucal sesamoids [9]. Not all stress fractures of the tibia, however, are high risk. Posteromedial tibial stress fractures, frequently seen in runners and other endurance athletes, as opposed to the tension-sided anterior cortical fracture, are on the compression side of the tibial shaft and respond more favorably to nonsurgical treatment.
Risk Factors
Stress fractures may occur in two distinct scenarios: abnormal stresses applied to normal bone (fatigue) or normal stresses applied to abnormal bone (insufficiency). Thus, risk factors are based upon these two inciting causes. Insufficiency fractures may commonly be due to metabolic bone disease, endocrinopathy, chronic renal disease, post-radiation therapy, smoking, infection, and benign or malignant bone tumors (pathologic fracture). These fractures are frequently observed in the sacrum, vertebral bodies, pubic rami, calcaneus, and proximal femoral diaphysis [10]. Fatigue fractures are overuse injuries. Thus, training errors, competition, nutrition, equipment, extremity biomechanics, and bony alignment all play significant roles in the development of fatigue stress fractures (Table 10.2). Girls and women with the “female athlete triad” are especially at risk for bone stress injuries, including both stress reaction and stress fracture [11]. They often exhibit characteristics of both fatigue and insufficiency fracture, with amenorrhea or oligomenorrhea, overall energy deficiency imbalance, and low bone mineral density osteoporosis [11].
Table 10.2
Risk factors for fatigue tibial stress fractures in runners
• Rapid increase in training intensity |
• Rapid increase in training mileage |
• Leg-length discrepancy |
• Knee stiffness |
• Increased hip adduction |
• Subtalar eversion and foot pronation |
• Pes cavus |
• Female athlete triad |
• Hard running surfaces |
• Old, worn running shoes |
History
The patient’s history is a key component of establishing a correct diagnosis in the patient assessment for a suspected stress injury of bone (Table 10.3). It requires not only asking specific questions pertinent to a chief complaint, but also actively listening and responding with successive adaptive questions related to the patient’s responses. It is advantageous to obtain the history and examine the patient prior to viewing images.
Table 10.3
Clinical history pearls for evaluation of tibial stress fracture
• History of prior stress fracture |
• Recent increase in training intensity, duration, or equipment |
• Focal pain localization—with activity, including weight bearing, running, jumping |
• Pain progression from after activity, to with activity, to activities of daily living, to rest |
• Female athlete triad |
The history of present illness can often all but definitively make a diagnosis prior to even examining the patient or reviewing images in assessment of the possible tibial stress fracture. Characterization of the principal symptoms attributable to the chief complaint should describe seven entities [12]: Location, quality, severity, timing (onset, duration, frequency), setting, exacerbating and relieving factors, and associated manifestations. Pertinent positive and negative findings from the past medical history, family history, social history, review of systems, and medication list are all also very relevant. Patient demographics and epidemiology must also not be overlooked, especially age and gender, as these factors do play a significant role in evaluating overuse injuries.
Pain Localization
Pain location is an important component in clinical diagnosis. In the diagnosis of tibial stress fracture, it is vital to localize exactly where the patient feels the most severe pain, either at rest or with activity. If necessary, it may be beneficial to have the patient run or jump for 5–10 min to reproduce the symptoms and better pinpoint the location of pain. The main additional differential diagnosis in the evaluation of shin pain in possible overuse injury is medial tibial stress syndrome, or “shin splints.” In diaphyseal tibial stress fractures, the pain is frequently insidious in onset, over a prodromal 2- to 4-week course, and often coincides with a change in training volume and/or intensity. Initially, the pain is after activity, then progresses to during activity, especially weight-bearing during running or jumping on the affected leg, and may progress to activities of daily living and/or at rest. Anterior or anterolateral, tension-sided, tibial stress fractures often present in jumpers, ballet, or dancers at the central one-third of the diaphysis and the athlete typically points with one finger “this is where it hurts.” Compression-sided fractures often present in runners at the posteromedial tibia (similar to medial tibial stress syndrome). However, these fractures may present proximally, distally, or in the mid-shaft. Patients may point to a focal area of pain or may more broadly or vaguely state that “it hurts around this area.” Patients with medial tibial stress syndrome similarly complain of vague diffuse exertional pain along the posteromedial border of the tibia at the mid-distal portion of the shaft.
Patients with stress fractures in other locations of the tibia often complain of focal tenderness to touch and weight-bearing pain. Similar to diaphyseal fractures, these fractures may initially be only after activity, progress to pain with activity, and eventually be present with activities of daily living and/or rest. In medial malleolar stress fractures, patients will complain of weight-bearing pain at the medial malleolus, especially with running, and pain with ankle motion. In patients with proximal tibia stress fractures, activity-related weight-bearing pain is common at the location of the fracture.
Exacerbating and Relieving Factors
Circumstances that aggravate a painful sensation often clue the clinician into the diagnosis. Factors that relieve pain include rest, medications, and procedures. In patients with tibial stress fracture, exacerbating factors include running (e.g., compression side posteromedial tibia), jumping or dancing (e.g., tension-side anterior tibia due to force of posterior calf musculature), and weight bearing (e.g., ambulation). Relieving factors usually include rest, reduction in weight bearing and loading of the leg, anti-inflammatory medications, and ice cryotherapy.
A helpful history pearl that may distinguish medial tibial stress syndrome and tibial stress fracture is the pain response to a training session. Patients with stress fractures tend to have worsening of pain in the location of the fracture with a single training session as the session progresses to the point that the athlete sometimes has to stop due to pain. Athletes with medial tibial stress syndrome, in the early stages, may actually have pain at the beginning of a training session that gradually subsides during that training session.
Other Findings
The clinician must be cognizant of other possible contributing coexistent pathology that may predispose the athlete to stress fracture. A thorough foot exam may reveal rigid pes cavus, subtalar pronation, tarsal coalition, muscle imbalance, weakness, or stiffness. Pes planus has also been shown to predispose to medial tibial stress syndrome [8]. However, other studies have shown, rather than pes planus, it is the ratio of subtalar everter to inverter muscles (in favor of eversion) that is predictive of increased risk of medial tibial stress syndrome [13]. Evaluation of leg-length is necessary as a significant leg-length discrepancy is associated with tibial stress fracture [14].
Physical Examination
The physical examination for the lower limb with an overuse injury should be comprehensive and systematic. This allows for consistency and reproducibility during examination of patients with not only tibial stress fractures (Table 10.4), but all potential causes. It should, just as questioning during a proper history, be adaptive as well. Physical assessment of any limb or joint requires visual inspection, palpation, motion, strength, and special (e.g., vibration tuning fork [15], tuning fork with stethoscope [16], and hop [17]) testing. Further, in order to understand if pathology is present in the involved tibia, the clinician must also thoroughly examine the contralateral tibia as well, with the knowledge that bilateral stress fractures may coexist. Extensions of the tibial stress fracture physical examination require evaluation from as far proximal as the lumbar spine and down the entire lower extremity as needed. This requires an assessment of coronal plane alignment, femoral version, tibial torsion, and pedal arch. Further, assessment of core strength, hip impingement, knee and ankle stability, and musculotendinous unit tightness (e.g., hamstring, hip adductors, iliotibial band, gastrocnemius-soleus-Achilles, plantar fascia) is warranted. Although the physical examination of the possible tibial stress fracture should focus on the presenting chief complaint, a comprehensive physical examination should also identify other abnormalities that may predispose the patient to other overuse injuries (i.e., injury prevention).
Table 10.4
Physical examination pearls in the evaluation of tibial stress fractures
• Focal point tenderness at the site of the fracture |
• Edema, palpable periosteal thickening |
• Positive single-leg “hop” test, although nonspecific |
• Positive “tuning fork” test |
• Absent compartment swelling, nerve symptoms |
• Evaluate for possible contributing coexistent pathology (e.g., muscular tightness, contracture) |
• Running gait observation and analysis |
Tibia-Specific Physical Examination
The key physical examination finding to distinguish a tibial stress fracture from other causes of leg pain is primarily focal point tenderness at the location of the fracture, usually the anterior or medial tibia. As opposed to the latter, patients with medial tibial stress syndrome frequently have more diffuse, nonfocal tenderness along the posteromedial middle to distal one-third of the tibia and not the anterior tibia. If the patient reports that the pain only occurs after an activity, such as running, then the clinician should have the patient go outside of the clinic and run, or in the training room or physical therapy arena, run on a treadmill. The tenderness may be exacerbated by a tuning fork test. The tuning fork test has a sensitivity, specificity, positive predictive value, and negative predictive value of 75 %, 67 %, 77 %, and 63 %, respectively. The single-leg hop test is also frequently utilized in the evaluation of all lower extremity stress fractures, not just the tibia [18]. However, this test is nonspecific, as it is also positive in up to 46 % of patients with medial tibial stress syndrome [19]. Edema and palpable periosteal thickening are also observed in patients with tibial stress fractures. In patients with medial tibial stress syndrome, edema is usually absent.
Inspection
Thorough inspection of the tibial stress fracture requires observation of the core and entire lower extremity. In addition to the patient himself/herself, shoe wear patterns should also be observed. One should also note prior surgical incisions and observe any deformity or asymmetry in alignment, swelling, calluses, and blisters. The clinician should observe for any swelling, edema, ecchymosis, or erythema. Gait evaluation by either observation in clinic or outside of clinic, on a treadmill or via digital video analysis gives a real-time evaluation of biomechanical factors that may predispose to stress injuries of the tibia (Fig. 10.1a–c).
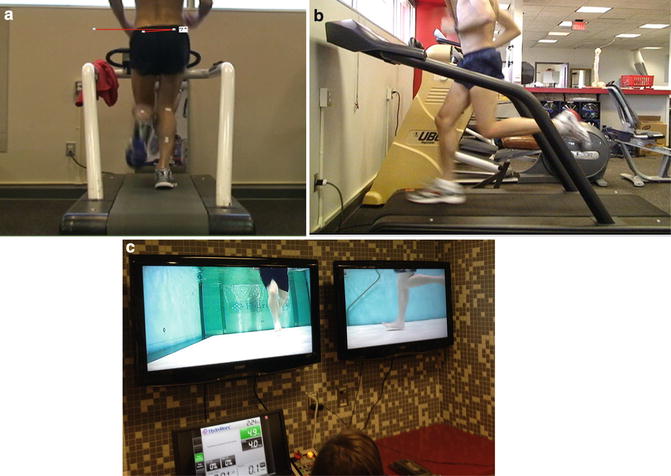
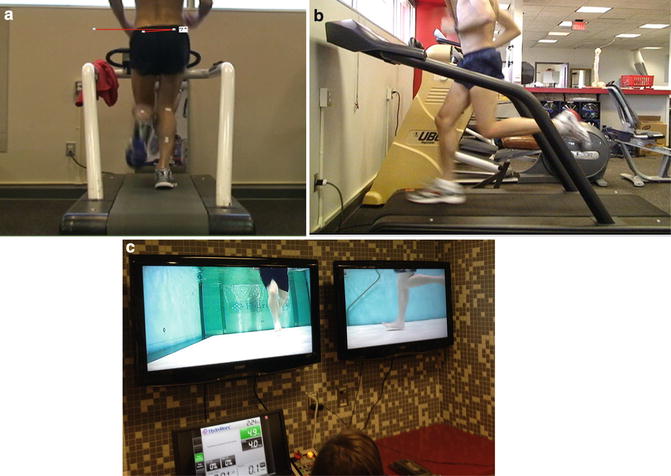
Fig. 10.1
(a) Posterior still-frame photograph from a treadmill running gait analysis of an elite-level distance runner demonstrating 7° of pelvic tilt. (b) Lateral still-frame photograph from the same runner demonstrating stride length with neutral foot-strike. (c) Still-frame photograph of gait analysis performed on an elite-level long jumper via aquatic treadmill as the athlete recovered from a tibial stress fracture
Palpation
This is a key component in the tibial stress fracture evaluation. All osseous and soft tissue structures warrant palpation. In the leg, this includes, among others, the subcutaneous tibia, the knee joint, tibial tubercle, fibular head, medial and lateral malleoli, the popliteal fossa, calf musculature and Achilles tendon, and plantar fascia. The patient with a tibial stress fracture may exhibit focal tenderness with percussion testing, a positive tuning fork and single-leg hop test, and edema. Patients with medial tibial stress syndrome usually exhibit more diffuse, nonfocal tenderness along the posteromedial mid-distal tibia without edema. Patients with medial malleolar stress fractures have tenderness over the medial malleolus and pain with forced passive ankle dorsiflexion and rotation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








