Author
Year
Sex
Age
Unilateral or bilateral
Fracture type
Fracture location
Sport
Treatment
Devas
1960
M
23
U
Longitudinal
Lateral facet
Running
Fragment excision
Devas
1960
M
28
U
Transverse
Middle 1/3
Running/hockey
Suture tension band
Sugiura
1977
M
12
U
Transverse
Distal 1/3
Soccer
–
Sugiura
1977
M
17
U
Transverse
Distal 1/3
High jump
–
Hanel
1981
M
15
B
Transverse
Distal 1/3
Basketball
ORIF
Tibone
1981
M
34
B
Transverse
Distal 1/3
Basketball
Fragment excision, patellar tendon repair
Dickason
1982
M
12
U
Transverse
Distal 1/3
Soccer
Cast
Hensal
1983
M
17
B
Transverse
Middle 1/3
Basketball
ORIF K-wire tension band
Iwaya
1985
M
12
U
Longitudinal
Lateral facet
Running
Activity modification
Iwaya
1985
M
11
U
Longitudinal
Lateral facet
Japanese fencing
Activity modification
Iwaya
1985
F
10
U
Longitudinal
Lateral facet
Gymnastics
Activity modification
Dickoff
1987
M
25
U
Longitudinal
–
Running
Activity modification
Schranz
1988
M
27
U
Longitudinal
Lateral facet
Running
Fragment excision
Jerosch
1989
M
20
U
Transverse
Distal 1/3
Soccer
ORIF K-wire tension band
Rockett
1990
M
20
U
Transverse
Distal 1/3
Basketball
Knee immobilizer
Teitz
1992
M
23
U
Transverse
Distal 1/3
Skiing/sailboarding
ORIF K-wire tension banda
Teitz
1992
F
36
U
Transverse
Distal 1/3
Belly dancing
Cast
Oginni
1993
M
29
U
Transverse
Distal 1/3
Palmwine tapper
Fragment excision, patellar tendon repair
Pietu
1995
M
16
U
Transverse
Distal 1/3
Basketball/skiing
Splint
Garcia Mata
1996
M
23
U
Transverse
Junction middle/distal 1/3 s
Soccer
Splint/cast
Mason
1996
F
48
U
Transverse
Middle 1/3
Running
ORIF
Mason
1996
F
15
U
Transverse
Distal 1/3
Gymnastics
Knee immobilizer
Mason
1996
M
23
U
Transverse
Middle 1/3
Basketball
Activity modification
Orava
1996
M
25
U
Transverse
Distal 1/3
Volleyball
Cast
Orava
1996
F
19
U
Longitudinal
Lateral facet
Running
Fragment excision
Orava
1996
F
19
U
Transverse
Distal 1/3
High jump
ORIF tension band
Orava
1996
M
22
U
Transverse
Distal 1/3
Soccer
ORIF K-wire tension band
Orava
1996
F
21
U
Transverse
Distal 1/3
Orienteering
ORIF tension band
Brogle
1997
M
22
U
Transverse
Distal 1/3
Basketball
ORIF cannulated screws
Garcia Mata
1999
M
12
U
Transverse
Junction middle/distal 1/3 s
Soccer
ORIF screw fixation
Mayers
2001
M
21
U
Transverse
Distal 1/3
Weight lifting
ORIF tension band
Crowther
2005
M
35
U
Transverse
Distal 1/3
Tennis
ORIF K-wire tension band
Carneiro
2006
M
64
B
Transverse
Middle 1/3
Running
ORIF K-wire tension band
Keeley
2009
M
20
U
Transverse
Distal 1/3
Basketball
ORIF single cortical screw
Sillanpaa
2010
F
18
U
Longitudinal
Lateral facet
Floorball/floor hockey
Absorbable cross pins
Definition
Stress fractures occur because of repetitive loading of a bone. A stress fracture occurs when the repetitive load (stress) is less than the ultimate strength of the bone, as opposed to a traumatic fracture which occurs when a single loading episode exceeds the ultimate bone strength and the bone fractures. In engineering terms, a stress fracture is a fatigue failure that occurs when the repetitive load and cycles exceed the endurance strength of a material. Non-biologic materials, such as metals and polymers, cannot auto-repair so a fatigue failure occurs when the microscopic damage accumulates and results in a macroscopic failure. However, biologic tissues, such as bone, have the potential to heal and repair themselves. Therefore, microscopic damage (microfractures) must accumulate faster than the bone can repair and remodel itself in order for a catastrophic macroscopic failure (displaced fracture) to result.
Mason et al. [2] summarize Daffner and Pavlov’s work [3] to describe two types of stress fractures. “There are two types of stress fractures: fatigue fractures and insufficiency fractures. Fatigue fractures occur when increased stresses are applied to normal bone. Insufficiency fractures occur when normal stresses are applied to bone that has been weakened by a generalized disorder such as osteoporosis or osteomalacia.” With the possible exceptions of females with the female athlete triad or older athletes with osteoporosis, patellar stress fractures in athletes should be classified as fatigue fractures.
Patellar stress fractures have been described in children with cerebral palsy [4–8]. The presumed mechanism of injury is the increased quadriceps muscle forces required for ambulation with a “crouched” gait. Additionally, many children with cerebral palsy have seizure disorders and certain antiseizure medications can cause osteoporosis. Because this subgroup of patients are not usually competitive athletes, the diagnosis and management of this patient subgroup will not be included in this chapter. Patella stress fractures after total knee arthroplasty have been described [7, 9]. It is likely that such fractures are insufficiency fractures due to osteonecrosis of the patella (Fig. 9.1). This patient fell after he felt a “pop” and his knee buckled. The fracture was treated with a locked reconstruction plate (Fig. 9.2).

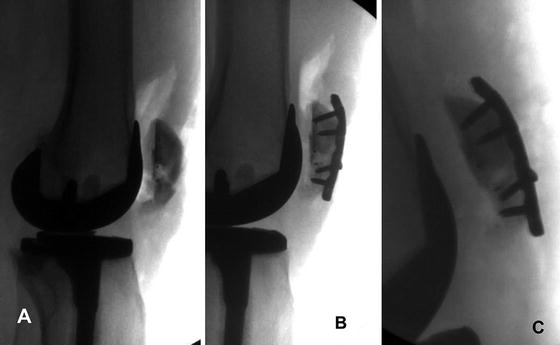

Fig. 9.1
Lateral radiograph showing an atraumatic transverse patella fracture after a total knee arthroplasty. Published with kind permission of © Gregory A. Brown 2014
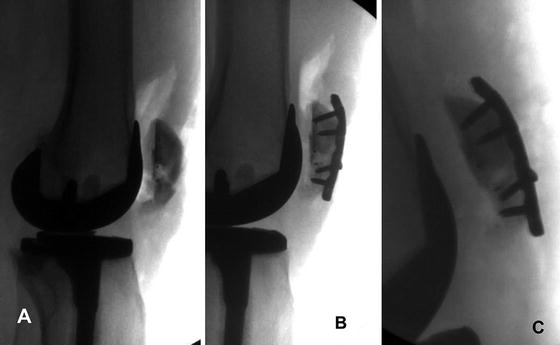
Fig. 9.2
Lateral radiographs depicting (a) provisional reduction with cerclage suture; (b) patella fracture short segment fixation with a locking reconstruction plate; and (c) healed fracture 3 months postoperatively. Published with kind permission of © Gregory A. Brown 2014
Patellar stress fractures have been described after previous surgical procedures involving the patella. Boden and Osbahr [7] describe patellar stress fractures after harvesting bone-patellar tendon-bone grafts for anterior cruciate ligament reconstruction. The stress concentration effect of the bony defect increases the effective stress at the site of the bony defect resulting in a stress fracture. Gregory et al. [10] reported three cases of longitudinal patella stress fractures after transosseous extensor mechanism repair. The stress concentration effect of the longitudinal drill holes increased the effective stress in the patella causing a stress fracture. MRI images of one of the cases demonstrated tunnel enlargement or cystic changes that would further increase the stress concentration effect. Thaunat and Erasmus [11] reported on three cases of avulsion fractures of the medial patella after previous medial patellofemoral ligament reconstruction. However, all three events were associated with trauma, so the designation of this being a stress avulsion fracture could be debated.
A bipartite patella arises when a secondary patella ossification center fails to unite with the primary ossification center. According to the Saupe classification as cited by Gaheer et al. [12], there are three types of bipartite patella: (1) inferior pole (Type I, 5 %), (2) lateral margin (Type II, 20 %), and (3) superolateral pole (Type III, 75 %). The junction of the bipartite patella fragment may become painful due to repetitive stress [13] and may be considered a “stress” response. If the superolateral Type III bipartite patella becomes persistently painful and does not respond to non-operative management, it can be excised and the quadriceps tendon repaired to the patella. Okuno et al. [14] reported four cases of traumatic separation of a Type I bipartite patella. Two cases were treated with open reduction and internal fixation and two cases were treated with cast immobilization.
Incidence
The incidence of patella stress fractures is exceedingly rare. Two retrospective series [15, 16] and one prospective series [17] of stress fractures in athletes do not report patella stress fracture incidence (presumably due to the rarity of the diagnosis). The largest series [16] notes the anatomic distribution of stress fractures is tibia (49.1 %), tarsals (25.3 %), metatarsals (8.8 %), femur (7.2 %), fibula (6.6 %), pelvis (1.6 %), sesamoids (0.9 %), and spine (0.6 %). Wall and Feller [18] report a German series by Csizy, Babst, and Fridrich with an anatomic distribution of tibia (33 %), navicular (20 %), metatarsals (20 %), femur (11 %), fibula (7 %), and pelvis (7 %). The incidence of patella stress fractures is so rare; neither series delineates patella stress fractures. However, Iwamoto and Takeda [15] include a review of four series that delineate patella stress fractures: Sugiura (2/162 = 1.2 %), Tajima (2/111 = 1.8 %), Sakai (1/251 = 0.4 %), and Iwamoto (1/196 = 0.5 %). The pooled incidence is 0.83 % (6/720). Therefore, the incidence of patella stress fractures appears to be less than 1 %. Given the percentage of sports medicine patients with stress fractures presenting to a sports medicine clinic is approximately 2 % (196/10,276 = 1.91 %) [15] and patellar stress fractures comprise less than 1 % of stress fractures, the probability of seeing a patient with a patella stress fracture is less than 0.02 % (2/10,000).
Because the incidence of patellar stress fractures is so low, all case reports published in English are tabulated in Table 9.1. Twenty-three authors reported on 35 cases (Devas—2 cases [19], Suguira as reported by Mason [2]—2 cases [20], Hanel—1 case [21], Tibone—1 case [22], Dickason—1 case [23], Hensal—1 case [24], Iwaya—3 cases [25], Dickoff—1 case [26], Schranz—1 case [27], Jerosch—1 case [28], Rockett—1 case [29], Teitz—2 cases [30], Oginni—1 case [31], Pietu—1 case [32], Garcia Mata—2 cases [33, 34], Mason—3 cases [2], Orava—5 cases [35], Brogle—1 case [36], Mayers—1 case [37], Crowther—1 case [38], Carneiro—1 case [39], Keeley—1 case [40], and Sillanpaa—1 case [41]). Table 9.1 includes the case report author, year of publication, patient sex, patient age, unilaterality or bilaterality of fracture, fracture type (transverse or longitudinal), fracture location, sport, and treatment.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








