Fig. 13.1
Lateral radiograph of a classic stress fracture in the posterior body of the calcaneus approximately 3 weeks after the onset of symptoms in a long distance runner

Fig. 13.2
T1-weighted MRI scan demonstrating a stress fracture of the calcaneus, as indicated by the dark, jagged line running perpendicular to the axis of the posterior tuberosity
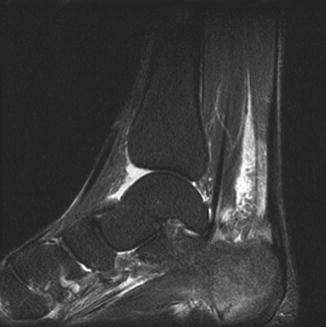
Fig. 13.3
Short tau inversion recovery (STIR) MRI image of the calcaneal stress fracture in the same patient as Fig. 13.2. Note the surrounding edema in the posterior tuberosity
Treatment
There is a strong consensus for nonoperative treatment of calcaneal stress fractures, and indeed the only report in the literature of surgical repair is that of a 67-year-old woman who sustained displaced fractures of both calcaneal tuberosities during a 3-week hiking trek [17]. Both fracture fragments were displaced substantially superiorly, compromising Achilles tendon function. The fragments were reduced and fixed with cancellous screws. In the several large series of calcaneal stress fractures reported from the military [1–3, 5, 6], and for the few calcaneal stress fractures reported in athletes [8, 11, 12], nonoperative management invariably has led to full resolution of symptoms and a return to the previous level of activity. Nonoperative treatment consists of 2–6 weeks of restricted weight-bearing activity, until the pain with weight-bearing resolves, followed by a gradual resumption of vigorous activities such as running and jumping. There are no reports on the need for cast immobilization during the acutely painful period, and long-term shoe-wear modification to treat recurrent or residual symptoms does not seem to be necessary.
The experience with military recruits has demonstrated that premature return to vigorous activity, prior to full resolution of weight-bearing symptoms, can lead to a recurrence of symptoms [2]. To avoid a recurrence of symptoms in athletes, Haverstock [13] recommended a two-phase plan to restore function. Phase I includes rest with non-weight bearing and activity restriction until the patient is pain free with weight bearing. This phase may take as long as 8 weeks. Then, in Phase II, activities are gradually reintroduced over a 6- to 12-week period. During this time, if pain returns activity should be decreased.
With the exception of the one case report noted above [17], no displacement of a stress fracture of the body of the calcaneus has been reported, and healing consistently occurs in this cancellous bone. To our knowledge, no long-term sequelae have been reported with this fracture.
Special Circumstances
Two cases of stress fracture of the anterior process of the calcaneus in association with a fibrous calcaneonavicular coalition have been reported in athletes [18, 19], and there is one report in the literature of a stress fracture of the body of the calcaneus in association with a talocalcaneal coalition [20]. In all three cases, the authors postulated that there was increased stress on the calcaneus due to restriction of rear foot motion caused by the coalition. Two of these fractures were treated nonoperatively with full resolution of symptoms. One of the anterior process fractures [19] was treated surgically with excision of the calcaneonavicular coalition and compression screw fixation of the stress fracture. This professional rugby player had returned to full activity without pain within 6 months.
A stress fracture of the anterior process of the calcaneus without a calcaneonavicular coalition was reported by Taketomi et al. [21] in a 14-year-old female basketball player. Because of persistent pain at 6 months after the onset of symptoms, the ununited fracture was treated surgically with multiple drilling across the fracture site with a 1.5-mm Kirschner wire. Following 4 weeks of postoperative non-weight bearing cast immobilization, the patient gradually resumed activity. The fracture was healed radiographically at 6 months, and she resumed playing basketball without pain.
In 2004, Ogden et al. [22] reviewed a group of 14 skeletally immature athletes with persistent heel pain for at least 9 months. All had the clinical diagnosis of Sever’s disease, or calcaneal apophysitis. An MRI scan was obtained, and, in each case, it demonstrated edema and hemorrhage in the metaphysis of the calcaneus, consistent with the diagnosis of stress fracture. All 14 patients were treated with a cast (3) or a removable ankle-foot orthosis (11) and non-weight bearing for 3–4 weeks. In all cases the symptoms subsided following immobilization, and everyone was able to gradually resume sports participation without pain. The authors concluded that Sever’s disease is a “… chronic (repetitive) injury to the actively remodeling trabecular metaphyseal bone that results in a variably sized stress injury…” and that it is not an apophysitis. This observation has not been confirmed by others.
In summary, stress fractures of the calcaneus result from impact loading and occur occasionally in runners. The typical fracture traverses the posterior body of the calcaneus and many can be diagnosed clinically. Following 2–3 weeks of symptoms, most can be confirmed radiographically as a condensation of new bone. In the absence of plain radiographic findings, magnetic resonance imaging can be used to identify the fracture line and associated marrow edema; however, caution must be used to not “over read” these MRI findings in athletes. Virtually all of these fractures heal completely with rest and avoidance of impact loading, allowing the athlete to resume his or her sport at previous levels of performance.
Sesamoids
Stress fractures of the sesamoids occur rarely in athletes, and the literature contains only a few sparse retrospective reports of small case series, usually focused on a common treatment scheme. As a result, there is little good evidence upon which to base treatment decisions.
The rarity of these fractures has been documented in three reports on stress injuries in athletes [7], college athletes [8], and collegiate track and field athletes [9]. A total of 169 stress injuries to bone were confirmed by scintigraphy [7] or MRI [8, 9] in these three studies; 87 occurred in the foot, but only three involved a sesamoid bone, two medial, and one lateral.
The medial sesamoid, which is larger and longer, lies within the substance of the tendon of the medial head of the flexor hallucis brevis, and the smaller and rounder lateral sesamoid lies within the substance of the tendon of the lateral head of the flexor hallucis brevis [23]. Portions of the abductor hallucis (medially) and the adductor hallucis (laterally) insert onto the sesamoids which are held together securely by the intersesamoid ligament [24]. Dietzen [25] pointed out that the sesamoids have no appreciable periosteum, as their plantar surfaces are covered by the plantar aponeurosis and dorsally they are covered by articular cartilage where they articulate with the metatarsal head.
Both sesamoids arise from multiple ossification centers between 7 and 10 years of age [24], and, not infrequently, the ossification centers fail to fuse together resulting in partition (bipartite or multipartite), particularly of the medial sesamoid [26]. While the reported rates of partition range widely from 0.1 to 33.5 %, the most frequently reported rates are 10 % for the medial and 1 % for the lateral sesamoid [24, 26]. Partition occurs with equal frequency in males and females, and, when present, it is bilaterally symmetrical in about 25 % of cases [27]. Partition of a sesamoid can be misinterpreted as a fracture on plain radiographs, and one study in military recruits has shown that mild to moderately increased scintigraphic activity over a bipartite sesamoid does not necessarily reflect clinically significant pathology [28]. These issues can cloud the assessment of the athlete with pain on the plantar aspect of the first metatarsal head.
Clinical Presentation
An athlete with a stress fracture of either sesamoid will develop pain that is usually well localized to the plantar aspect of the foot under the first metatarsophalangeal joint. The pain is usually insidious in onset, aggravated by athletic activity, and relieved by rest. These fractures are thought to result from repetitive forced dorsiflexion and seem to occur more frequently in running and jumping sports in which the great toe is loaded in dorsiflexion [27, 29]. In one series of 10 athletes [30], 7 were noted to have a plantarflexed first ray. Both sexes seem to be equally vulnerable, with certain sports showing a predilection (football in males [30] and gymnastics and dancing in females [30, 31]). In coed sports such as long distance running fracture rates are similar between males and females. Most of these fractures have been reported in young college age adults, with the youngest reported case occurring in a 7-year-old ballerina [31]. In addition to having activity-related pain on the ball of the foot, on physical examination most patients will have tenderness well localized to the affected sesamoid, some local swelling, and often increased pain with passive dorsiflexion of the great toe [32].
In many of the reported cases the diagnosis has been delayed, and in one series of 15 cases [33], the time between onset of symptoms and definitive diagnosis averaged 43 weeks. Three factors appear to be responsible for this delay. First, because these fractures occur in competitive athletes, many will try to “run through” or “play through” the pain and not report it to their medical team. Many athletes apparently do not seek medical attention immediately, and some do not do so for many weeks or months [34]. Secondly, in contrast, if the athlete is evaluated soon after the onset of symptoms, as with other stress injuries to bone, the initial radiographs may not demonstrate any abnormality, and the diagnosis of stress injury is not made. Finally, a slowly healing, or ununited, stress fracture may be difficult to distinguish on plain radiographs from a bipartite or tripartite sesamoid which has become symptomatic due to overuse.
The differentiation of a symptomatic partitioned sesamoid (“sesamoiditis”) from a slowly healing stress fracture can be suggested by plain radiographs [35] and then facilitated by assessment with bone scanning [36, 37] and/or magnetic resonance imaging [35, 38]. On plain radiographs, the typical stress fracture is transverse and only minimally displaced with a fairly distinct fracture surface (Fig. 13.4). Mittlmeier and Haar [39] have pointed out that instability of a stress fracture may be demonstrated by progressive separation of the fragments over time. In contrast, the components of a partitioned sesamoid are usually rounded with smooth surfaces and, when measured in combination are larger than the size of a non-partitioned sesamoid [35] (Fig. 13.5). Technetium-99 bone scanning will demonstrate increased uptake at a stress fracture site, often before the fracture is visible on plain radiographs [36, 37], and magnetic resonance imaging can demonstrate both stress reactions and stress fractures with a higher degree of sensitivity and greater specificity than bone scanning [38]. It should be remembered that inflammation due to overuse involving a partitioned sesamoid may result in a positive bone scan or magnetic resonance finding [35].



Fig. 13.4
Typical radiographic appearance of a fractured lateral sesamoid

Fig. 13.5
Typical appearance of a bipartite medial sesamoid. Note the smooth rounded surfaces and also note that the two parts in total are much larger than the lateral sesamoid
Magnetic resonance imaging is the diagnostic modality of choice currently when clinical signs and symptoms point to a stress reaction or fracture as the cause and plain radiographs are normal [35]. The best planes for imaging are coronal (perpendicular to the long axis of the first metatarsal) and sagittal. T1- as well as T2-weighted images (including fat suppression or STIR sequences) should be obtained (Fig. 13.6). Contrast enhancement does not appear to be necessary. These images will demonstrate slightly decreased intensity on T1-weighted images and marrow edema on the T2-weighted images. It should be remembered, however, that similar MRI findings can be seen with sesamoiditis and osteonecrosis of the sesamoid bones [35].
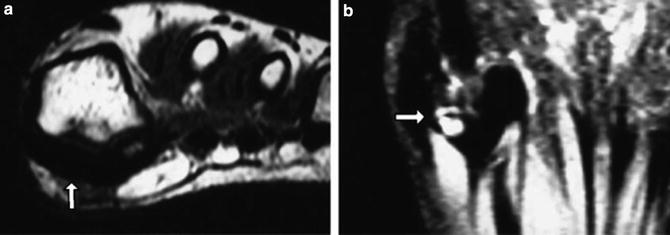
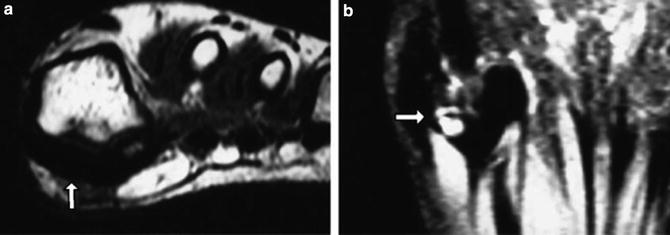
Fig. 13.6
(a) Axial T1 demonstrating a medial sesamoid stress fracture with marrow signal replacement by edema. (b) Coronal T2 fat-suppressed image of the same patient showing a transverse dark line consistent with fracture. Reprinted from Sports Medicine Clinics, 25(4), Joseph Wall, John F. Feller, Imaging of stress fractures in runners, 781–802. Copyright 2006, with permission from Elsevier
In summary, stress fracture of the sesamoids is primarily a clinical diagnosis confirmed by imaging studies. When plain radiographs clearly demonstrate a fracture, further imaging is not necessary [35]. When the clinical findings strongly suggest a stress fracture, but X-rays are negative, MRI will usually demonstrate one when it is present. On the other hand, no evidence of increased uptake on bone scan, or no evidence of marrow edema on MRI in the presence of normal radiographic findings (or partition of the sesamoid) should lead to further investigation.
Treatment
Treatment of a stress fracture of the sesamoid is based in part upon the duration of symptoms prior to presentation. As noted above, many athletes will try to ignore the injury pain soon after its onset and may present only after several weeks or months of persistent pain that limits performance. Most of the clinical treatment series reported in the literature focus on surgical treatment in patients with persistent symptoms who have failed nonoperative treatment [37, 39–41]. In these cases, nonoperative treatment typically consisted of cessation of the athletic activity and use of a short leg cast for 6–8 weeks followed by the use of a custom molded orthotic device with gradual resumption of sports as symptoms allowed. Richardson [27] noted that stress fractures of the sesamoid “…usually heal adequately with rest and nonoperative treatment.” He recommended non-weight bearing cast treatment for 6–8 weeks followed by the use of a molded orthotic device with relief under the first metatarsal head. Dietzen [25] described the use of a custom made orthotic device consisting of a rubber lined plastic arch support with a J-shaped pad to relieve pressure on the affected sesamoid. This orthotic device was further described by Axe and Ray [30]. Unfortunately, we could find no clinical series in the literature reporting on the effectiveness of early nonoperative treatment of sesamoid fractures.
Three techniques have been described for the surgical treatment of persistently symptomatic nonunion of stress fractures of the sesamoids: excision, bone grafting, and screw fixation.
Excision
In 1982 van Hal et al. [32] were the first to report successful treatment of four patients with ununited and persistently symptomatic stress fractures by complete excision of the sesamoid (two medial and two lateral). All four resumed athletic activities with no residual symptoms. In their series of 26 feet in 10 athletes and 13 “active patients,” Saxena and Krisdakumtorn [42] excised the tibial sesamoid in 16 and the lateral sesamoid in 10 with generally good results. However, two patients developed hallux valgus, one developed hallux varus and one developed great toe stiffness requiring a subsequent arthrodesis. In a biomechanical study in cadavers, Aper et al. [43] concluded that complete resection of the medial, lateral, or both sesamoids resulted in a decrease in the effective moment arm of the flexor hallucis longus, but partial resection of either sesamoid alone did not. In light of these findings, more recent authors have recommended partial, rather than total, sesamoid excision, when possible [27, 29, 39]. Biedert and Hintermann [29] described the use of a medial incision to excise the proximal fragment of a tibial sesamoid nonunion with repair of the flexor tendon after excision of the fragment. Richardson [27] describes excision of the fibular sesamoid through both a dorsal and a plantar approach.
Bone Grafting
In the single largest reported series of patients with nonunion of the sesamoids, Anderson and McBryde [44] described a technique of autogenous bone grafting without internal fixation. Among a group of 24 patients, five had sustained an acute sesamoid fracture and the remaining 19 did not recall an acute injury but developed chronic pain as the result of daily athletic activities and were assumed to have stress fractures. Following failure of conservative treatment, all 24 underwent autogenous cancellous bone grafting of a minimally displaced (3 mm or less) tibial sesamoid nonunion. Twenty-one of the 24 were evaluated at long-term follow-up; in 19 cases the nonunion was healed radiographically and 17 patients had returned to their previous level of athletic activity. While there are no other reports in the literature documenting the effectiveness of this bone grafting technique, Anderson reports that he continues to use it in competitive athletes with good success as long as there is minimal diastasis between the fracture fragments, no gross motion between the fragments, and viability of both fragments [45].
Percutaneous Screw Fixation
In 2002 Blundell et al. [40] described a technique of percutaneous screw fixation of both medial (5) and lateral (4) transverse sesamoid fractures after they failed a course of nonoperative care. Eight of the fractures occurred gradually over time and appear to have been stress fractures; seven were in high-performance athletes. Through a stab incision, the distal pole of the sesamoid was exposed and using image intensification a guide wire was placed across the fracture, which was then compressed with a self-tapping Barouk screw (DePuy International, Leeds, UK). At 6 months after surgery, all nine patients had returned to their previous level of athletic activity with no reported complications. Similar good results of compression screw fixation have been reported by Mittlmeier and Haar [39] and Pagenstert et al. [41]. This technique, however, should be used with caution and only in experienced hands, as the small sesamoid can be shattered easily by over-aggressive screw compression.
In summary, in athletes stress fractures can occur in either sesamoid bone, probably as the result of excessive repetitive tension on the plantar plate structures of the first metatarsophalangeal joint. Pain underlying the first metatarsal head combined with local swelling and tenderness should make the examiner suspect a stress reaction or fracture even with normal appearing radiographs. Magnetic resonance imaging may facilitate the diagnosis. When diagnosed early, avoidance of pain inducing activity should lead to resolution of symptoms and fracture healing. Continued stress despite pain (as is often the norm with many athletes) may lead to delayed union or frank nonunion of the fracture. At this point it may be difficult to distinguish partition of the sesamoid from stress fracture, but this is likely only an issue of semantics, as persistent severe symptoms, unrelieved by activity and shoe-wear modifications, will require surgical intervention. Partial excision of an ununited fracture can lead to satisfactory results, as can autologous cancellous bone grafting. Alternatively, in skilled and experienced hands, when there is minimal displacement and two reasonably sized fracture fragments, percutaneous screw fixation can provide a simple means of securing healing and restoring the athlete to a high level of performance.
First Through Fourth Metatarsals
First Metatarsal
In large surveys of foot fractures, the first metatarsal has only rarely been implicated in stress fractures [46, 47]. These fractures typically occur at the proximal metaphyseal/diaphyseal junction [48]. There are case reports in non-athletes noting that increased medial stresses on the foot may be an inciting factor [49, 50]. Case reports of these fractures in athletes suggest that they can usually be treated nonoperatively. One such case report involved the apparent gradual evolution of a Salter-Harris III stress fracture at the base of the first metatarsal in a 14-year-old male athlete. While he could recall no specific trauma to the affected foot, the patient experienced pain dorsally over the first ray with extended walking or when jumping/landing while playing basketball. Although the specific etiology of this fracture was not identified, symptomatic treatment with rocker sole shoe modification and activity limitation yielded complete resolution of his symptoms [51]. In a similar case report, a 14-year-old female field hockey player was found to have bilateral first metatarsal stress fractures. The same treatment was initiated (rigid-soled shoes and relative rest), yielding similarly successful results with radiographic healing of the fracture and clinical resolution of symptoms [52].
Second, Third, and Fourth Metatarsals
Background
The middle metatarsals (second, third, and fourth) are cross-sectionally weaker than the first and fifth metatarsals [53]. Thus, it is no surprise that stress fractures of these metatarsals are common, representing a majority of the reported metatarsal stress fractures in athletes [48, 54–57]. Metatarsal stress fractures were initially recognized over 150 years ago in members of the military and called “march fractures.” While they continue to be a frequent cause of injury in members of the military, especially new recruits, middle metatarsal stress fractures are also commonly seen in dancers and other athletes [54, 58–60].
Pathophysiology
Activities or conditions that increase chronic stress on the feet can predispose patients to lesser metatarsal stress fractures. Studies have linked several nonathletic factors to metatarsal stress fractures as well, including varus foot deformities, diabetic neuropathy, osteoporosis, rheumatoid arthritis, and surgeries such as metatarsal osteotomy, resection of adjacent metatarsals, endoscopic plantar fasciotomy, and Keller bunionectomy [61–65]. Less common causes of lesser metatarsal fracture include reports of soft tissue osteochondromas and plantar ganglion cysts that alter the forces on the plantar aspect of the foot [66–68].
Military personnel represent a unique type of “athlete,” and are often subject to unusual foot stresses, such as those that result from marching or operating military machinery. One study found that among Royal Marine military recruits in the UK, third metatarsal stress fractures were the most commonly experienced stress fracture, accounting for 38 % of all stress fractures recorded in the study [69]. Stress fractures in military recruits have been found to result from repetitive, low-impact plantar stresses caused by marching [15, 70], and from the mechanics of running particular to soldiers wearing boots. Biomechanical analyses have shown that forefoot loading pressures (secondary to significantly earlier peak rear foot eversion when running in military boots) were significantly higher in military recruits who had a history of metatarsal stress fractures [71].
While the precise microscopic pathogenesis of stress fractures in the middle metatarsals is not known, studies have shown that the material strength of the metatarsal bones, rather than the geometry, is of central importance in determining their susceptibility to stress fractures. In vitro tests of human second metatarsals demonstrated that a high bone mineral density and high volumetric cortical density were most strongly correlated with an ability to resist cantilever bending [72]. There has also been speculation that repeated stress leads to the formation of microcracks which then progress to overt stress fracture [73, 74]; however, in vitro studies of microcracks in metatarsals have yet to be causally linked to stress fractures [75].
Clinical Presentation
Although commonly associated with runners and ballet dancers, second through fourth metatarsal fractures can occur in any sport that involves repetitive loading of the forefoot [48]. These fractures often present with pain that is poorly localized, ill-defined, and only triggered by specific foot positions; swelling over the dorsum of the foot; and midfoot pain exacerbated by weight bearing [76–79].
Second metatarsal stress fractures in athletes tend to occur in one of two areas: (1) the base and (2) the distal diaphysis. Fractures in these two areas are associated with differing clinical patterns: proximal fractures have been found to be associated with lower bone mass, lower training volumes, and chronic/multiple metatarsal fractures, whereas distal fractures are found in higher-stress, higher-impact training, such as running [80]. Proximal fractures of the middle metatarsals have a worse prognosis than distal fractures, with increased recovery time, and higher rates of delayed union and nonunion [81, 82]. Stress fractures can also be seen in less common areas such as the metatarsal head.
Ballet dancers are at risk for foot injuries, and particularly for stress fractures of the second metatarsal base [77, 83–89]. This predilection for the base of the second metatarsal is relatively unique to dancers, and is thought to be caused by the foot and body movements that put unusual stresses on the feet, including standing “en-pointe” with the entire body weight supported on the toes and the fully plantarflexed foot. Similar stresses and fractures have also been seen in classical Irish dancers [90]. While often seen in dancers, this injury is not unique to dancing and also can be seen in sports such as basketball, soccer, and running [91]. It was traditionally thought that ballet dancers with a relatively short first ray experienced second metatarsal stress fractures more commonly than dancers with a relatively long hallux. However, studies in both dancers and non-dancers have found no correlation between hallux length and middle metatarsal stress fractures [92, 93].
Runners are especially prone to second through fourth metatarsal stress fractures [94], with up to 20 % of 211 collegiate runners sustaining stress reactions to these metatarsals over their careers [8, 9]. Running was the most common sport to cause a stress fracture in a database review of 320 athletes treated for stress fracture, and those patients who sustained metatarsal stress fractures averaged 38 miles a week for men and 26 miles a week for women [57]. Among experienced runners with no history of metatarsal fracture, a change in footwear from regular running sneakers to barefoot-simulating shoes has been associated with the occurrence of second metatarsal stress fracture, supporting the idea that alterations in the direction and magnitude of repetitive foot stresses can play a role in the pathogenesis of middle metatarsal stress fractures in athletes [95].
Imaging
Imaging should begin with plain radiographs, which may show a progression of periosteal reaction over time, as in the second metatarsal shaft fracture seen in Fig. 13.7. More sensitive studies such as MRI can be used to identify stress reactions before they become evident on X-ray (Fig. 13.8). Recent studies have also shown the effectiveness of ultrasonography in early detection of metatarsal fractures that may not be visible on plain radiographs [78, 96–98].

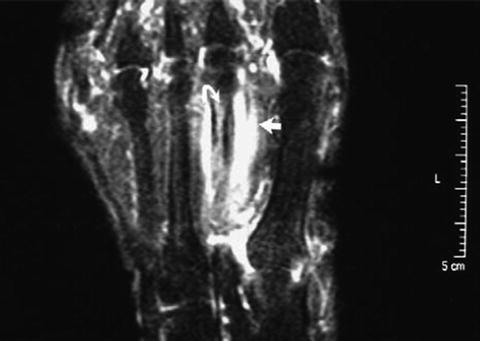

Fig. 13.7
Progression of a second metatarsal stress fracture over 3 months. Note the progression of periosteal reaction. Reprinted from Radiologic Clinics of North America, 40(2), Imaging of stress fractures in the athlete, 313–31. Copyright 2002, with permission from Elsevier
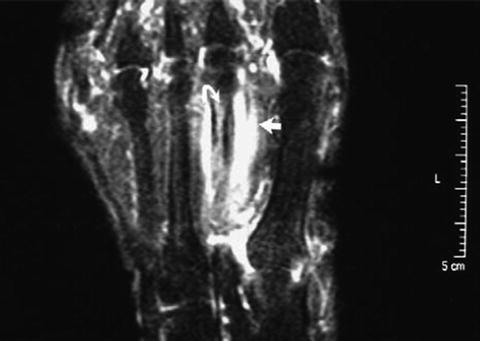
Fig. 13.8
Short tau inversion recovery (STIR) image of a second metatarsal stress fracture. The curved arrow shows bone marrow edema and the straight arrow surrounding soft tissue swelling. Reprinted from Sports Medicine Clinics, 25(4), Joseph Wall, John F. Feller, Imaging of stress fractures in runners, 781–802. Copyright 2006, with permission from Elsevier
Treatment
Treatment of second through fourth metatarsal stress fractures is generally nonsurgical. Nondisplaced fractures of the metatarsal shaft have a good prognosis, generally requiring only a soft dressing, a firm, supportive shoe or cast boot, and progressive weight bearing; though immobilization and non-weight bearing is sometimes indicated if less pain persists. An attempt at closed reduction may be indicated if there is dorsal or plantar displacement of the metatarsal shaft of more than 3–4 mm, or if angulation exceeds 10°, though the intermetatarsal ligament typically holds the metatarsal heads well aligned and prevents plantar prominence [99].
Supplemental bone stimulation of fracture healing can be considered in athletes. In one study of 19 young ballet dancers with fractures of the lesser metatarsals, early treatment was initiated with external shock wave therapy (ESWT) or pulsed electromagnetic fields (EMF), with good results in all of the dancers [100].
Prevention
Prudent increase in training, footwear and early imaging with sensitive modalities may help prevent second through fourth metatarsal stress fractures. In several studies of stress fractures in military recruits, alteration of the stresses on the feet using orthotics was found to reduce the pathological stresses and the incidence of middle metatarsal stress fractures [79, 101]. A study of collegiate basketball players showed that prophylactic MRI imaging of the feet can reveal pathologic changes secondary to athletic stresses in the metatarsals, including bone marrow edema that may precede stress fracture [102]. Recognition of this pre-fracture state may allow prevention and earlier treatment.
Fifth Metatarsal
Classification/Grading
Historically, there has been confusion and inconsistency in the classification of fractures of the fifth metatarsal. Fractures of the proximal fifth metatarsal are often associated with the eponym Jones fractures. In 1902 Sir Robert Jones reported a small series of fractures, including his own, at the metaphyseal/diaphyseal junction of the fifth metatarsal [103]. These fractures were further clarified as extending into the articular facet between the fourth and fifth metatarsal [104]. Jones fractures have typically been considered acute injuries without prodromal symptoms, and therefore are not considered stress fractures.
The terms “pseudo-Jones fractures” and “dancer’s fracture” also confuse the issue of classification. Pseudo-Jones fractures are avulsion injuries of the proximal fifth metatarsal base which exit proximal to the articulation of the fourth and fifth metatarsal, and are acute injuries [105]. The term dancer’s fracture typically refers to an acute spiral oblique fracture of the fifth metatarsal shaft [106]. When describing fractures, it is more useful to avoid eponyms and to instead specify the location and chronicity of the fracture.
The fifth metatarsal has classically been divided into three zones with zone I representing avulsion injuries, zone II representing “Jones” fractures, and zone III representing stress fractures in the proximal 1.5 cm of the diaphysis (Fig. 13.9a) [55, 107–109]. It has been suggested by Polzer et al. that, given the amorphous differentiation between zones II and III, fractures in both areas be considered as a single group, as their etiology, healing potential and treatment preferences are similar (see Fig. 13.9b) [110, 111]. Indeed, it appears that consistently differentiating between these zones is difficult, and any fracture distal to the tuberosity of the fifth metatarsal may have a component of stress and overuse, even if the fracture occurs after an acute incident.
Fig. 13.9
(a) The classification of Lawrence et al., indicating the proximal diaphysis as the site of fifth metatarsal stress fractures [108]. (b) The classification of Plozer et al., which combines the region of traditional diaphyseal stress fractures with fractures that extend into the distal 4–5 metatarsal articulation, as both behave similarly. Reprinted from Injury, 43(10), Polzer H, Polzer S, Mutschler W, Prall WC, Acute fractures to the proximal fifth metatarsal bone: development of classification and treatment recommendations based on the current evidence, 21626–32. Copyright 2012, with permission from Elsevier
One of the most frequently cited classification systems focusing on chronicity is that of Torg, which was designed to aid in clinical management. Torg originally described 46 fractures distal to the tuberosity of the fifth metatarsal, all of which occurred in athletes [112]. Type I fractures represent acute or acute-on-chronic injuries and have evidence of mild periosteal reaction and a sharp fracture line. Type II fractures are delayed unions and demonstrate a fracture line with associated periosteal reaction, with or without radiolucency from bone resorption around the fracture line, and with medullary sclerosis. Type III fractures are nonunions and demonstrate obliteration of the medullary canal along with periosteal hypertrophy and a widened fracture line. Among surgically treated fifth metatarsal stress fractures, there is evidence of increasing time to union with Type II and III fractures, supporting the clinical relevance of this classification [113, 114].
More recently, a classification system has been proposed that highlights the importance of fracture gap. Lee et al. divided fifth metatarsal stress fractures into complete (A) and incomplete (B) categories [113, 114]. Type A fractures are further subdivided into A1 fractures, which appear acute without signs of periosteal reaction, and A2 fractures, which are acute-on-chronic injuries and have evidence of periosteal reaction. Type B fractures are subdivided into B1 fractures, which have a fracture gap <1 mm, and B2 fractures, which have a fracture gap >1 mm. Among athletes treated with tension band wiring, the B2 fractures with a gap >1 mm demonstrated a significantly increased time to union, indicating that the presence of a fracture gap may well influence outcome in athletes [113, 114].
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree








