The operative management of developmental dysplasia of the hip is technically challenging. To achieve excellent results, surgeons need to select the most appropriate operative treatment, minimize the risk of complications, and be aggressive in the management of serious complications, such as redislocation and avascular necrosis, when they occur. This article outlines specific steps and strategies to assist in each of these key steps.
- •
Outcomes from the operative management of developmental dysplasia of the hip (DDH) are highly dependent on 2 major factors: first, the ability of a surgeon to accurately assess DDH and select the appropriate surgical procedure, and, second, the skill and precision with which the surgery is performed.
- •
Postoperative redislocation after open reduction is in most cases a preventable complication that can be avoided by adhering to surgical principles outlined in this article.
- •
The next most important complication or sequela in the surgical management of DDH is avascular necrosis (AVN). This is an iatrogenic problem because it is not seen in the natural history of DDH.
Introduction
Outcomes from the operative management of DDH are highly dependent on 2 major factors: first, the ability of a surgeon to accurately assess DDH and select the appropriate surgical procedure and, second, the skill and precision with which the surgery is performed. AVN or osteonecrosis and growth disturbance may result from intrinsic or extrinsic factors and are often unavoidable iatrogenic sequela of open or closed hip reduction. Redislocations may be unavoidable but surgical technique is nevertheless important.
Postoperative redislocation after open reduction is in most cases a preventable complication that can be avoided by adhering to surgical principles outlined in this article. Redislocation has the potential to compromise all future attempts at restoring normal function to the hip. The first section of this article addresses how to avoid this devastating complication by highlighting some key steps in the surgical technique of open reduction of the dislocated hip. The second section discusses how to decide when to add a pelvic osteotomy, a femoral osteotomy, or both to enhance the stability of the newly reduced hip. The third section of this article outlines how to salvage the hip that has suffered a redislocation.
The next most important complication or sequela in the surgical management of DDH is AVN. This is an iatrogenic problem because it is not seen in the natural history of DDH. The fourth section of this article discusses strategies to reduce the AVN rate and, finally, the fifth section describes how to manage it when it does occur.
Preventing redislocation of the hip after open reduction through an anterior approach
The following are the major reasons why a hip may redislocate postoperatively:
- 1.
Failure to identify and expose the true acetabulum and achieve a concentric reduction.
A thorough knowledge of the pathoanatomy of a child’s dislocated hip is crucial to successfully achieving adequate exposure of the true acetabulum and achieving a concentric reduction. The authors have found it helpful to use a surgical headlamp to assist with visualization during open reductions. Using a standard Smith-Peterson approach through a bikini line incision, the anterior aspect of the hip must be exposed to the medial aspect of the acetabulum and laterally to the level of the apex of the dislocated femoral head. After dividing the long head of rectus femoris just distal to its attachment to the anterior inferior iliac spine, the surgeon should spend time fully exposing the anterior aspect of the hip joint capsule. Unless excellent exposure of the hip joint capsule is achieved one cannot hope to perform a well-placed capsulotomy to visualize the true acetabulum. The exposure involves 2 key maneuvers. The first is to develop a plane of dissection superolaterally between the joint capsule and the hip abductors along the line of the reflected head of rectus femoris. This tissue plane can then be connected to the subperiosteal plane previously developed along the lateral aspect of the ilium using curved Mayo scissors. The second maneuver is to develop the tissue plane across the anterior aspect of the hip joint capsule. The iliopsoas tendon is firmly adherent to the anterior capsule at this point and it is critical to bluntly dissect this plane, such that a Langenbeck retractor or Hohmann retractor may be placed medial to the true acetabulum between the iliopsoas tendon and the anterior capsule. The authors find that the combination of a spade-shaped periosteal elevator and a large swab are ideal instruments to achieve this step in a safe and controlled manner. Failure to free the iliopsoas from the capsule at this point compromises the ability to extend the medial aspect of the capsulotomy to expose the true acetabulum despite performing an iliopsoas tenotomy over the pelvic brim. The iliopsoas tendon is recessed just proximal to the musculotendinous junction. The surgeon should avoid transection of the femoral nerve, which lies just medial and anterior to the tendon. Great care is required to ensure an accurate capsulotomy, which should follow the line of the acetabulum, approximately 5 mm to 8 mm distal to its edge. A common error is to veer too inferiorly with the medial aspect of the capsulotomy, thus leaving a tight band of capsular tissue anteriorly, preventing clear visualization of the true acetabulum and even preventing concentric reduction of the femoral head. This can be avoided by using a Macdonald elevator to probe the anteromedial aspect of the acetabulum through the initial small anterior capsulotomy to guide the surgeon as to the correct medial extension of the capsulotomy. After opening the capsule, the ligamentum teres should be identified from its origin on the femoral head and traced down to its insertion at the fovea of the true acetabulum, which should now be clearly seen under direct vision. If it is not clearly seen, there is usually inadequate medial dissection and capsullotomy. The adjacent medial capsule and transverse acetabular ligament must be cut because these structures are always contracted in a hip that has been dislocated for a significant length of time.
- 2.
Excessive tension across the hip joint.
Adductor tenotomy and iliopsoas recession are integral steps to relieve tension across the joint. The actual reduction of the femoral head into the acetabulum should not be a forceful event. In most children over the age of 30 months, a femoral shortening osteotomy is necessary to bring the femoral head to the level of the acetabulum. It is important to remove sufficient bone (typically 1–2 cm) such that the femoral head may be reduced without too much tension. Doing so also reduces the likelihood of AVN. It is better, however, to err on the side of initially resecting too little bone and subsequently adjusting the tension by removing a little more as necessary.
- 3.
Inadequate tension across the hip joint to maintain stability.
There is a tendency to remove too long a segment of bone from the femur, thereby compromising the postoperative stability of the hip. It is often recommended to reduce the femoral head after the femoral osteotomy and then to remove the amount of bone that is overlapping. This maneuver often suggests resecting a larger segment of bone than is actually necessary. To avoid this catastrophic occurrence, moderate traction should be applied to the leg before determining the amount to be resected. It is rare that more than 2 cm of bone needs to be resected.
- 4.
Abnormal version of the proximal femur.
A marked increase in femoral anteversion is not universal in DDH after walking age. Bilateral, high, posterior dislocations may be associated with femoral retroversion. First, the associated abnormality of version must be assessed intraoperatively in each child, and, second, great care must be taken with the amount of correction (derotation) placed at the osteotomy site. The most common technical error is overcorrection, leaving the proximal femur retroverted, leading to posterior subluxation or dislocation postoperatively. A helpful rule is to never correct the anteversion to less than 20°. Dividing the estimated amount of anteversion present in half and then externally rotating the leg at the osteotomy by this amount best achieves this goal. The explanation for this is because of the windlass effect on the soft tissues with femoral rotation. After significant rotational realignment, the total arc of rotation at the hip is reduced by the increase in soft tissue tension generated. Failure to recognize and correct excessive femoral anteversion may lead to gradual subluxation of the hip after cast removal. The leg is typically internally rotated in the cast and when postimmobilization stiffness resolves and the leg externally rotates back to neutral, the hip may subluxate anteriorly.
- 5.
Failure to redirect the acetabulum into the proper position.
Inadequate correction of the acetabular dysplasia with an acetabuloplasty or a Salter innominate osteotomy may cause persistent instability and resubluxation in the cast. Overcorrection (more likely with a triple innominate osteotomy) may leave posterior acetabular wall deficiency and posterior dislocation that may not be recognized intraoperatively.
- 6.
Tying the sutures in the capsular repair before fixation of the femoral and/or pelvic osteotomies.
If performing a one-stage open reduction and osteotomy, tying the capsular repair should always be the last step of the operation, before wound closure, to ensure a secure reduction. Pelvic and femoral osteotomies result in an alteration of the morphology of the hip joint. A capsulorrhaphy performed before these osteotomies loses tension, leading to immediate loss of stability, and may subsequently lead to redislocation.
- 7.
Loss of control of the operated hip in the transition from end of the surgical procedure to the application of the hip spica cast.
The operating surgeon should be in complete control of the newly reduced hip at all times. This is particularly important when the superficial tissue layers are being closed and preparations are made to apply a hip spica cast. There can be a loss of concentration of the surgical team combined with the child being repositioned that may lead to an unidentified perioperative redislocation. The operating surgeon must maintain control of the leg throughout this period of transition to ensure reduction is held and to identify redislocation while coordinating the rest of the team to prepare the spica cast.
- 8.
Inadequate molding of the spica cast over the greater trochanter.
The hip spica cast is an important element of the comprehensive operative management of the dislocated hip. A spica cast can maintain reduction of a more unstable hip if expertly applied by the use of molding to support the hip. Using the thenar eminence, the cast should be molded carefully over the lateral and posterior aspect of the greater trochanter to ensure there is no dead space (as indicated by a gap between soft tissue and cast on postoperative imaging) that compromises the stability of the hip.
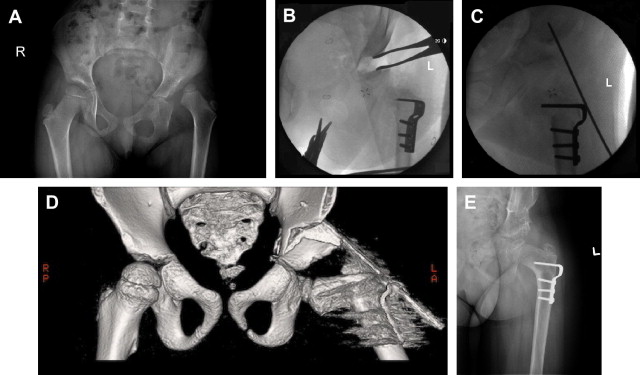
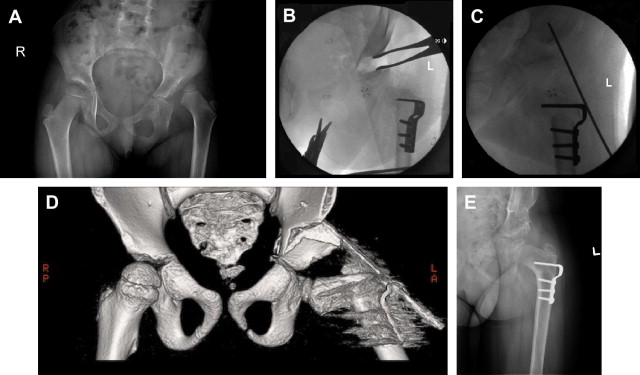
Dislocations in children with a poorly defined margin between the true acetabulum and false acetabulum and a high acetabular index may be difficult to completely stabilize using a standard menu of open reduction, capsulorrhaphy, and osteotomies ( Fig. 1 A). If there is still a tendency of the femoral head to slide proximally after fixation of the osteotomy(ies) and repair of the capsule even with the leg in a position of maximal stability, then it is occasionally necessary to use extra-articular fixation from the greater trochanter to the ilium proximal to the pelvic osteotomy. This is achieved using a large threaded Steinmann pin or Kirschner wire, which can be removed through a window in the spica cast at 4 to 6 weeks postoperatively (see Fig. 1 E).
Preventing redislocation of the hip after open reduction through an anterior approach
The following are the major reasons why a hip may redislocate postoperatively:
- 1.
Failure to identify and expose the true acetabulum and achieve a concentric reduction.
A thorough knowledge of the pathoanatomy of a child’s dislocated hip is crucial to successfully achieving adequate exposure of the true acetabulum and achieving a concentric reduction. The authors have found it helpful to use a surgical headlamp to assist with visualization during open reductions. Using a standard Smith-Peterson approach through a bikini line incision, the anterior aspect of the hip must be exposed to the medial aspect of the acetabulum and laterally to the level of the apex of the dislocated femoral head. After dividing the long head of rectus femoris just distal to its attachment to the anterior inferior iliac spine, the surgeon should spend time fully exposing the anterior aspect of the hip joint capsule. Unless excellent exposure of the hip joint capsule is achieved one cannot hope to perform a well-placed capsulotomy to visualize the true acetabulum. The exposure involves 2 key maneuvers. The first is to develop a plane of dissection superolaterally between the joint capsule and the hip abductors along the line of the reflected head of rectus femoris. This tissue plane can then be connected to the subperiosteal plane previously developed along the lateral aspect of the ilium using curved Mayo scissors. The second maneuver is to develop the tissue plane across the anterior aspect of the hip joint capsule. The iliopsoas tendon is firmly adherent to the anterior capsule at this point and it is critical to bluntly dissect this plane, such that a Langenbeck retractor or Hohmann retractor may be placed medial to the true acetabulum between the iliopsoas tendon and the anterior capsule. The authors find that the combination of a spade-shaped periosteal elevator and a large swab are ideal instruments to achieve this step in a safe and controlled manner. Failure to free the iliopsoas from the capsule at this point compromises the ability to extend the medial aspect of the capsulotomy to expose the true acetabulum despite performing an iliopsoas tenotomy over the pelvic brim. The iliopsoas tendon is recessed just proximal to the musculotendinous junction. The surgeon should avoid transection of the femoral nerve, which lies just medial and anterior to the tendon. Great care is required to ensure an accurate capsulotomy, which should follow the line of the acetabulum, approximately 5 mm to 8 mm distal to its edge. A common error is to veer too inferiorly with the medial aspect of the capsulotomy, thus leaving a tight band of capsular tissue anteriorly, preventing clear visualization of the true acetabulum and even preventing concentric reduction of the femoral head. This can be avoided by using a Macdonald elevator to probe the anteromedial aspect of the acetabulum through the initial small anterior capsulotomy to guide the surgeon as to the correct medial extension of the capsulotomy. After opening the capsule, the ligamentum teres should be identified from its origin on the femoral head and traced down to its insertion at the fovea of the true acetabulum, which should now be clearly seen under direct vision. If it is not clearly seen, there is usually inadequate medial dissection and capsullotomy. The adjacent medial capsule and transverse acetabular ligament must be cut because these structures are always contracted in a hip that has been dislocated for a significant length of time.
- 2.
Excessive tension across the hip joint.
Adductor tenotomy and iliopsoas recession are integral steps to relieve tension across the joint. The actual reduction of the femoral head into the acetabulum should not be a forceful event. In most children over the age of 30 months, a femoral shortening osteotomy is necessary to bring the femoral head to the level of the acetabulum. It is important to remove sufficient bone (typically 1–2 cm) such that the femoral head may be reduced without too much tension. Doing so also reduces the likelihood of AVN. It is better, however, to err on the side of initially resecting too little bone and subsequently adjusting the tension by removing a little more as necessary.
- 3.
Inadequate tension across the hip joint to maintain stability.
There is a tendency to remove too long a segment of bone from the femur, thereby compromising the postoperative stability of the hip. It is often recommended to reduce the femoral head after the femoral osteotomy and then to remove the amount of bone that is overlapping. This maneuver often suggests resecting a larger segment of bone than is actually necessary. To avoid this catastrophic occurrence, moderate traction should be applied to the leg before determining the amount to be resected. It is rare that more than 2 cm of bone needs to be resected.
- 4.
Abnormal version of the proximal femur.
A marked increase in femoral anteversion is not universal in DDH after walking age. Bilateral, high, posterior dislocations may be associated with femoral retroversion. First, the associated abnormality of version must be assessed intraoperatively in each child, and, second, great care must be taken with the amount of correction (derotation) placed at the osteotomy site. The most common technical error is overcorrection, leaving the proximal femur retroverted, leading to posterior subluxation or dislocation postoperatively. A helpful rule is to never correct the anteversion to less than 20°. Dividing the estimated amount of anteversion present in half and then externally rotating the leg at the osteotomy by this amount best achieves this goal. The explanation for this is because of the windlass effect on the soft tissues with femoral rotation. After significant rotational realignment, the total arc of rotation at the hip is reduced by the increase in soft tissue tension generated. Failure to recognize and correct excessive femoral anteversion may lead to gradual subluxation of the hip after cast removal. The leg is typically internally rotated in the cast and when postimmobilization stiffness resolves and the leg externally rotates back to neutral, the hip may subluxate anteriorly.
- 5.
Failure to redirect the acetabulum into the proper position.
Inadequate correction of the acetabular dysplasia with an acetabuloplasty or a Salter innominate osteotomy may cause persistent instability and resubluxation in the cast. Overcorrection (more likely with a triple innominate osteotomy) may leave posterior acetabular wall deficiency and posterior dislocation that may not be recognized intraoperatively.
- 6.
Tying the sutures in the capsular repair before fixation of the femoral and/or pelvic osteotomies.
If performing a one-stage open reduction and osteotomy, tying the capsular repair should always be the last step of the operation, before wound closure, to ensure a secure reduction. Pelvic and femoral osteotomies result in an alteration of the morphology of the hip joint. A capsulorrhaphy performed before these osteotomies loses tension, leading to immediate loss of stability, and may subsequently lead to redislocation.
- 7.
Loss of control of the operated hip in the transition from end of the surgical procedure to the application of the hip spica cast.
The operating surgeon should be in complete control of the newly reduced hip at all times. This is particularly important when the superficial tissue layers are being closed and preparations are made to apply a hip spica cast. There can be a loss of concentration of the surgical team combined with the child being repositioned that may lead to an unidentified perioperative redislocation. The operating surgeon must maintain control of the leg throughout this period of transition to ensure reduction is held and to identify redislocation while coordinating the rest of the team to prepare the spica cast.
- 8.
Inadequate molding of the spica cast over the greater trochanter.
The hip spica cast is an important element of the comprehensive operative management of the dislocated hip. A spica cast can maintain reduction of a more unstable hip if expertly applied by the use of molding to support the hip. Using the thenar eminence, the cast should be molded carefully over the lateral and posterior aspect of the greater trochanter to ensure there is no dead space (as indicated by a gap between soft tissue and cast on postoperative imaging) that compromises the stability of the hip.
Dislocations in children with a poorly defined margin between the true acetabulum and false acetabulum and a high acetabular index may be difficult to completely stabilize using a standard menu of open reduction, capsulorrhaphy, and osteotomies ( Fig. 1 A). If there is still a tendency of the femoral head to slide proximally after fixation of the osteotomy(ies) and repair of the capsule even with the leg in a position of maximal stability, then it is occasionally necessary to use extra-articular fixation from the greater trochanter to the ilium proximal to the pelvic osteotomy. This is achieved using a large threaded Steinmann pin or Kirschner wire, which can be removed through a window in the spica cast at 4 to 6 weeks postoperatively (see Fig. 1 E).