Stiffness Before and After Total Knee Arthroplasty
Among the goals of total knee arthroplasty (TKA) are relief of pain and restoration of function. Adequate range of motion is necessary for return to certain activities. For example, to walk normally on level ground, a person needs 70 degrees of knee flexion. Ninety degrees is necessary to ascend most stairs (depending on the height of the rise), and 100 degrees is needed to descend stairs and clear the trailing leg. One hundred five degrees is required to arise from a regular chair without using arm support. It is essential, therefore, for patients to achieve maximal potential motion.
Multiple causes for stiffness after TKA are possible. They are related to the patient’s diagnosis, preoperative range of motion, prosthetic geometry used, surgical technique, intraoperative range of motion after capsular closure, postoperative rehabilitation, and wound healing factors.
The diagnoses most often associated with stiffness include juvenile rheumatoid arthritis, rheumatoid arthritis in some adults, psoriatic arthritis, and posttraumatic arthritis (especially in the presence of multiple surgical procedures). Other patient factors include patient pain threshold, presence of patella baja, ipsilateral hip involvement, heterotopic ossification, and overzealous physical therapy.
Ipsilateral arthritic involvement of the hip is sometimes overlooked as a cause of preoperative knee pain. It is not unusual for a patient to consult me for treatment of a painful knee after TKA when, in fact, the pain is referred from the hip. These painful knees often have diminished range of motion. It is difficult to rehabilitate a knee after TKA when it is below a stiff, painful hip. This is one reason to replace the hip before the knee in a patient with ipsilateral hip and knee involvement (see Chapter 10). When a patient who has undergone TKA is evaluated postoperatively for pain and stiffness resulting from ipsilateral hip arthritis, a common clinical finding is that the patient’s affected leg lies in external rotation in the supine position. (This might also occur, of course, if the patient has a knee flexion contracture).
A radiograph of the pelvis is essential to avoid missing an arthritic hip preoperatively before replacement of the ipsilateral knee. For preoperative planning, I always obtain a long-standing film of the patient that includes hips, knees, and ankles. This allows me to screen for hip pathologic factors and any anatomic deformity of the femur. I also ask a simple screening question during the preoperative workup. I ask patients if they have any difficulty whatsoever reaching their feet to cut toenails or tie shoes. If these activities of daily living are normal, significant hip pathologic process is unlikely. If the patient reports a disability with these functions, hip pathology must be eliminated.
Exposing the Stiff Knee
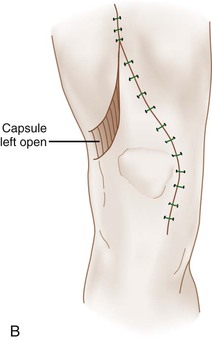
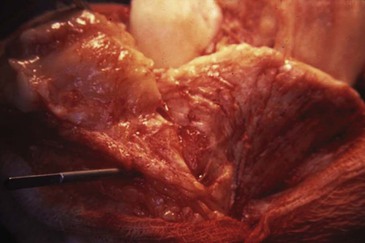
Exposure of the ankylosed knee can be difficult. Extreme care must be taken to avoid excessive stress on the patellar tendon insertion that might lead to patellar tendon avulsion. The two most common methods to facilitate exposure are a proximal release or a tibial tubercle osteotomy. I prefer the proximal release to avoid the potential morbidity of tubercle osteotomy, which includes wound-healing difficulties, problems with union of the osteotomy, and the potential for stress fracture at the osteotomy site. The classic proximal release is the so-called quadriceps snip initially described by Garvin and associates.1 I perform a modification of the snip in which the medial arthrotomy is taken to the top of the quadriceps tendon on the medial side and then brought distally along the lateral side of the tendon in an inverted V configuration (Figure 7-1).2 I prefer this release because it is easy to close and seal the joint to prevent leakage of the hematoma.
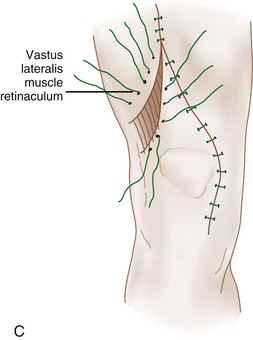
This procedure also can be extended to a formal V-Y quadricepsplasty to lengthen the quadriceps mechanism when appropriate. The proximal quadriceps release effectively takes tension off the patellar tendon and allows the patella to be turned rather like the page of a book. The surgeon then has access to lateral parapatellar scar tissue and the lateral retinaculum to perform a preliminary lateral release to further facilitate eversion and exposure. Despite these measures, I think it is advisable to place a smooth,  -inch pin into the tibial tubercle to further prevent the patellar tendon from avulsing or peeling off its insertion (Figure 7-2).
-inch pin into the tibial tubercle to further prevent the patellar tendon from avulsing or peeling off its insertion (Figure 7-2).
Exposing the Knee Ankylosed in Extension
When the knee is ankylosed in extension (the knee has limited potential to flex), I recommend the following sequence of maneuvers. An inverted V or quadriceps snip is performed upon initial exposure. Flexion of the knee is achieved by gentle manipulation. If the anterior cruciate ligament (ACL) is present, it is surgically released. In certain knees (in postseptic or juvenile rheumatoid arthritis), a joint line osteotomy using a saw or osteotomes may be required. A prophylactic tubercle pin is placed. During preparation of the femur, maximal trochlear resection is performed short of notching the anterior cortex. During preparation of the patella, maximal patellar resection is performed, leaving a remnant of as little as 10 mm in thickness. These two measures enhance flexion by increasing the quadriceps excursion. At the same time, the surgeon should avoid overstuffing the joint with too large a femoral component and too thick a patellar composite.
At the time of closure, flexion against gravity is measured with the capsule closed anatomically. If this range is deemed inadequate for the specific patient, consideration can be given to extending the inverted V quadriceps incision to a formal V-Y quadriceps lengthening (Figure 7-3).2 The disadvantage of V-Y quadriceps lengthening is the resultant extensor lag, which will depend on the amount of lengthening. The quadriceps usually will recover to an acceptable amount, but the patient may have to be braced during ambulation until active extension is −15 degrees or better.

< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


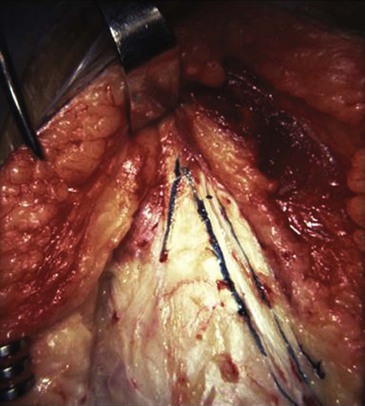
 -inch pin in the tibial tubercle protects the patellar tendon from avulsing.
-inch pin in the tibial tubercle protects the patellar tendon from avulsing.





