Sternoclavicular, Clavicular, and Acromioclavicular Injuries
Nicholas A. Bontempo
Augustus D. Mazzocca
INTRODUCTION
Injuries to the clavicle and its articulations are very common.
High-energy injuries have been seen in increasing frequency as more people participate in higher risk sports such as mountain biking and rollerblading.
Because man is an upper extremity-dependant animal, these injuries can lead to significant disabilities and limitations.
STERNOCLAVICULAR JOINT
Injury to the sternoclavicular (SC) joint is very uncommon. In one large study conducted by Rowe and Marble, out of 1,603 shoulder girdle injuries, there was only a 3% incidence of SC joint injuries (65). This is in comparison to an 85% incidence of glenohumeral injuries and 12% incidence of acromioclavicular (AC) dislocations. That being said, it has also been commented that SC joint dislocations are not as rare as posterior glenohumeral dislocations.
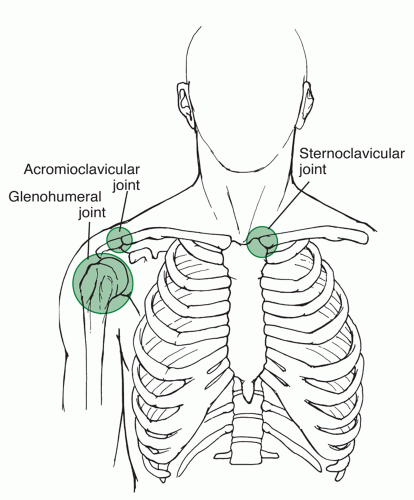
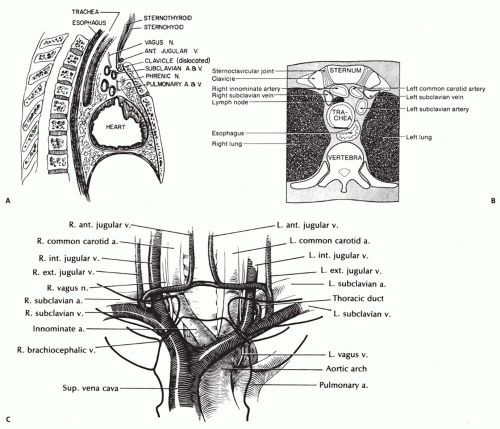
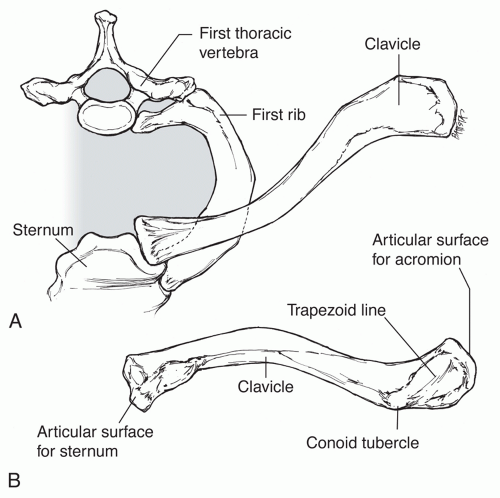
The SC joint is the only true joint connecting the axial skeleton to the shoulder girdle (Fig. 49.1).
Despite having such an important role, the SC joint lacks inherent bony stability and relies solely on ligamentous and capsular attachments.
Anatomy and Biomechanics
The SC joint represents the articulation of the proximal end of the clavicle with the sternum and is a diarthrodial joint.
Although the clavicle is the first long bone in the body to ossify during the fifth intrauterine week, the medial clavicular epiphysis is the last epiphysis to close. Closure of the medial clavicular epiphysis typically begins at age 18 and is usually fused to the clavicular shaft by age 25. It has even been documented in autopsy studies that complete union of the medial clavicular epiphysis may not occur until age 31(25).
Similar to the AC joint, the SC joint has an intra-articular disc, or meniscal homologue. Unlike the AC joint, however, the articular surface of the medial clavicle of the SC joint is covered with fibrocartilage.
The SC joint is incongruous as the medial clavicle is enlarged, bulbous, and saddle-shaped, whereas the clavicular notch of the sternum is concave. Because there is such a large discrepancy in shape and size of the clavicle with the sternum, there is relatively little to no bony stability of the joint. In fact, less than half of the medial clavicle actually articulates with the sternum. It has been shown that in 2.5% of patients, the inferior aspect of the medial clavicle actually articulates with the superior aspect of the first rib (42).
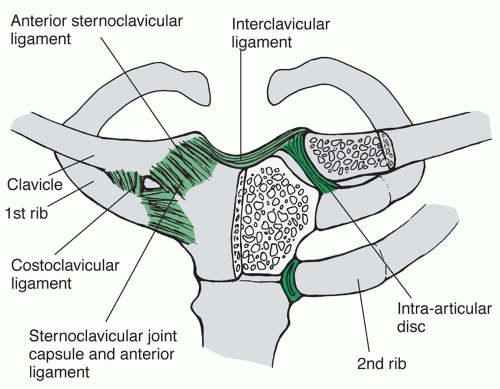
The SC joint articulation is held in place by the SC capsular ligaments, the costoclavicular ligaments, and the infraclavicular ligaments (Fig. 49.2).
There are two parts of the capsular ligament: the anterior and posterior portions. The capsular ligaments help to support and reinforce the anterosuperior and posterior SC joint. Of the ligaments surrounding the SC joint, the capsular ligament is the strongest and most important structure preventing upward displacement of the medial clavicle (62).
The intra-articular disc ligament arises from the junction of the sternum and first rib and attaches on the superior and posterior aspects of the medial clavicle, after passing directly through the SC joint. The fibers of the intra-articular disc ligament blend into the fibers of the capsular ligaments and help to separate the SC joint into medial and lateral compartments. It prevents medial displacement of the clavicle with compression.
The costoclavicular ligament consists of an anterior and posterior fasciculus with an interpositional bursa (62). The anterior and posterior fasciculi cross over one another, which helps to provide rotational stability of the SC joint during overhead elevation (67). The anterior fasciculus helps to resist upward rotation and lateral displacement of the medial clavicle. The fibers of the posterior fasciculus resist downward rotation and medial displacement of the medial clavicle.
Connecting the two clavicles is the interclavicular ligament, which connects the superomedial aspect of the clavicles and the
capsular ligaments. The purpose of this ligament is to maintain “shoulder poise,” by holding the clavicle and shoulder up (67).
Despite the presence of the ligaments and capsule stabilizing the SC joint, a relatively large amount of motion is still seen. There is approximately 30-35 degrees of upward elevation, 35 degrees of translation in the anterior to posterior plane, and 50 degrees of rotation around the longitudinal axis of the clavicle (12,20).
Classification
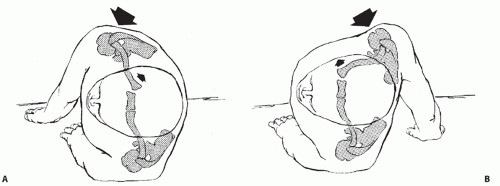
The SC joint can be dislocated anteriorly or posteriorly and be the result of traumatic or atraumatic injury (Fig. 49.3). Anterior and posterior dislocations are described based on the location of the medial clavicle with respect to the sternum. Of the 2 types of dislocations, anterior dislocations are far more common.
Atraumatic instability of the SC joint can either be acquired or congenital in etiology. The SC joint may subluxate or dislocate with overhead motion in patients who have systemic ligamentous laxity. Typically, atraumatic instability is not associated with pain.
Traumatic injury to the SC joint is the most common etiology. Motor vehicle collisions and sports participation are the top two causes of traumatic SC joint injury (43,44,45). Traumatic SC joint injuries have been classified into 3 types.
Type 1: mild sprain, SC joint is stable and ligaments are intact
Type 2: moderate sprain, SC joint subluxates and there is partial disruption of ligaments and capsule
Type 3: severe sprain, SC joint is dislocated and ligaments and capsule are completely disrupted
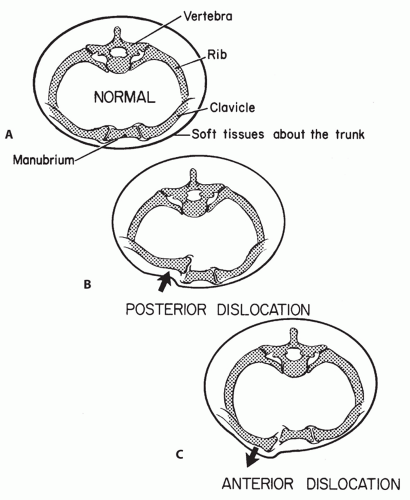
Figure 49.3: Cross sections through the thorax at the level of the SC joint. A: Normal anatomical relations. B: Posterior dislocation of the SC joint. C: Anterior dislocation of the SC joint.
Mechanism of Injury
Posterior dislocations of the SC joint typically occur as the result of a direct force to the anteromedial clavicle, as can happen during a motor vehicle collision, as a result of the steering wheel hitting the clavicle, or a direct kick to the chest (Figs. 49.4 and 49.5).
Anterior dislocations, on the other hand, rarely occur as a result of direct trauma. Instead, anterior dislocations can occur when an anterolateral force is applied to the clavicle and the shoulder is rolled backward. In three separate studies looking at SC joint dislocations, an indirect force was the most common mechanism of injury (9,26).
Rockwood describes a common mechanism of indirect SC joint dislocation — a pile-up during a football game (26). One player usually falls to the ground with the ball. Other players begin to jump and fall on top of the first player.
Physical Examination
Often with an acute dislocation, either anterior or posterior, palpable step-off at the SC junction can be appreciated (Fig. 49.6).
Posterior dislocations, although rare, have more significant symptoms and implications.
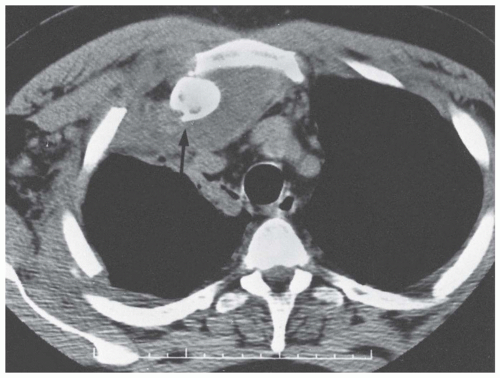
Posterior dislocations can be associated with venous congestion present in the neck or ipsilateral upper extremity from compression on the subclavian vessels (Fig. 49.7).
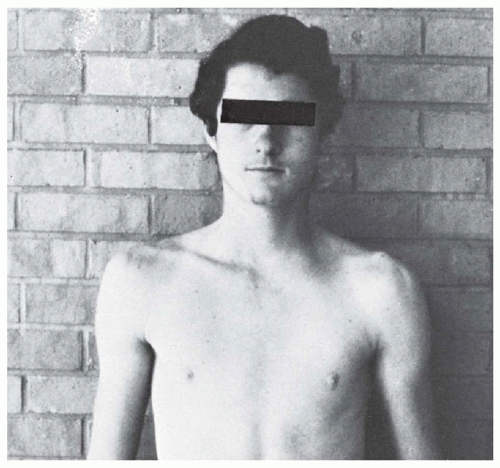
FIGURE 49.6: Clinical view of a patient with a left posterior SC joint dislocation. Notice the difference in appearance of the SC joint from the uninjured (right) side.
The posteriorly displaced clavicle can also compress the trachea or esophagus (Fig. 49.8).
As such, patients may complain of dyspnea, a choking sensation, difficulty swallowing, or a tight feeling in the throat.
In the most severe cases, the posterior dislocation can result in complete shock or a pneumothorax.
For patients with a type 1 injury (mild sprain), there is usually mild to moderate pain associated with movement of the upper extremity. Instability is usually absent, but the SC joint may be tender to palpation and slightly swollen. With this injury, the ligaments remain intact so the joint should not be unstable.
Type 2 injuries (moderate sprain) are associated with partial disruption of the ligaments. There may be some instability or subluxation when the joint is manually stressed, but it is not grossly dislocated or dislocatable. These patients usually have more swelling and pain than patients with type 1 injuries, and the SC joint is more tender to palpation.
Type 3 (severe sprain) injury results in complete dislocation, either anterior or posterior, of the SC joint. Patients with this injury present with severe pain that is exacerbated by any movement of the upper extremity. The ipsilateral shoulder may appear protracted in comparison to the contralateral uninjured shoulder. Patients will often hold the affected
arm across the chest in an adducted position and support it with the contralateral arm. The head may be tilted toward the side of the injured clavicle. Examination of the patient lying supine on the examining table will lead to a worsening of symptoms, and the involved shoulder will not lie flat on the table.
Radiologic Evaluation
A standard anteroposterior (AP) x-ray of the chest or SC joint may suggest an injury to the SC joint; however, this is not the best view for visualizing the joint.
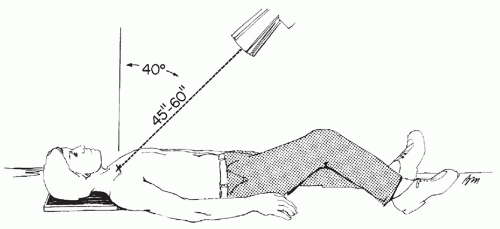
The serendipity view is the best view to visualize the SC joint. It is taken by tilting the x-ray tube 40 degrees cephalad and centered on the sternum (Fig. 49.9).
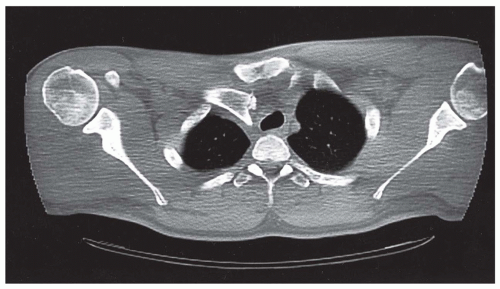
Computed tomography (CT) scan of the chest should include a special note to the radiology technician to do views of the bilateral SC joint for comparison. With a CT scan, axial sections can be viewed of both the injured and uninjured sides on one image. Subtle differences from side to side can be picked up more easily by the physician looking at the axial views.
Nonoperative Treatment
Type 1 and 2 injuries are often treated nonoperatively. Nonoperative treatment consists of a short period of immobilization in a sling, anti-inflammatory medication, and ice.
After a short period of immobilization, the patient can gradually return back to activities based on his or her own level of comfort.
As in type 2 injuries where the clavicle is subluxated, the joint can be reduced by retracting the shoulders in a figure-of-eight brace. This treatment modality can be incorporated whether the subluxation is anterior or posterior.
When the SC joint is completely dislocated, as seen in a type 3 injury, an attempt can be made at closed reduction.
For an anterior dislocation, the patient should be placed supine with a roll in the center of the back between the shoulder blades (Fig. 49.10).
This positioning allows the scapula to assume a retracted position and pull the clavicle laterally.
A gentle pressure can then be applied to the anteromedial clavicle in order to reduce.
Anterior dislocations are often easy to reduce; however, they are usually unstable and will dislocate once the pressure is released.
If, however, the SC joint maintains reduction after closed means, the patient should be immobilized in a soft figure-of-eight brace for a period of 6 weeks.
Prior to any attempt at closed reduction of posteriorly displaced clavicle, injury to local vessels, heart, and lung need to be ruled out.
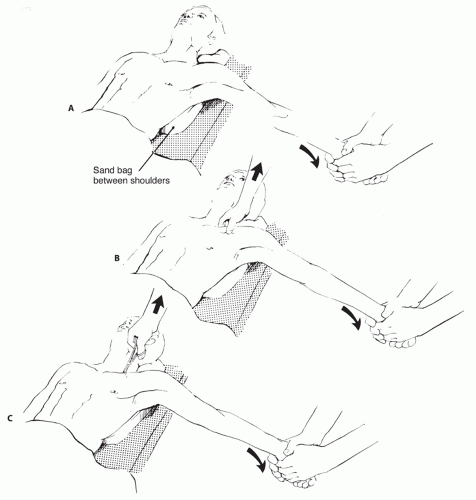
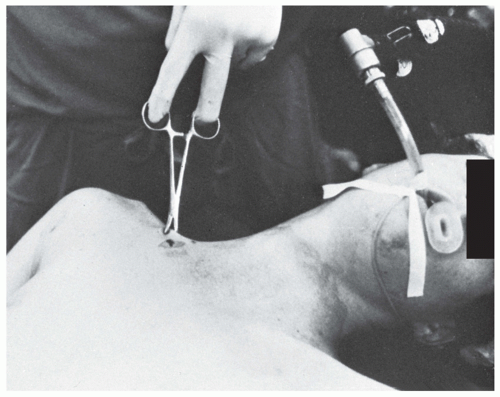
Closed reduction of a posterior dislocation should be done in the operating room with the patient under general anesthesia (Fig. 49.11).
Similar to an anterior dislocation, the patient should lay supine with a roll between the scapula.
Traction should then be applied to the abducted arm while it is slowly extended. Often the joint will reduce with this maneuver; if not, the clavicle can be manipulated with fingers or a towel clip.
The towel clip can be used to grasp the medial clavicle under sterile conditions and pull it anteriorly in order to achieve reduction.
Posterior dislocations are usually stable once reduced.
It is important to have a vascular surgeon available if the patient is taken to the operating room for an attempted closed reduction because of the potential complications that may arise as a result of the injury or the attempt at reduction.
The patient with a reduced SC joint should then be placed in a figure-of-eight brace for 4-6 weeks while the ligaments heal.
Operative Treatment
Most SC joint dislocations are best managed nonoperatively and either left unreduced or attempted to be closed reduced.
Surgical stabilization of the clavicle is not recommended by most authors (28,61). In most cases, the benefits of surgery are outweighed by the risks.
Numerous complications have been reported in the literature, including infection, recurrence, poor cosmesis, and hardware migration.
If patients develop symptomatic SC joint instability, then several surgical options exist.
Good long-term outcomes have been reported in patients who have medial clavicle excision or SC joint reconstruction for SC joint instability (50).
In a biomechanical analysis of reconstructions for SC joint instability, Spencer and Kuhn tested three SC joint fixation methods in a cadaveric study (68). They concluded that figure-of-eight semitendinosus reconstruction provided superior biomechanical properties to subclavius tendon reconstruction and intramedullary ligament reconstruction.
Cautiously recommended in the recent literature is a 2-stage approach for SC joint instability (77).
The first stage involves fixation of the medial clavicle to the sternum with a concomitant midclavicle osteotomy to offload the fixation at the SC joint.
The second stage, usually performed 4 months after the first, involves removal of the hardware at the SC joint and plate osteosynthesis at the osteotomy site.
Any surgery being performed for a posterior SC joint dislocation should be done with a cardiothoracic surgeon present due to risk of injury to surrounding structures.
CLAVICLE
The clavicle grows through intramembranous ossification like the skull and scapula.
Ossification begins at the fifth week of gestation, and it is the first bone to ossify.
It is also the last bone to finish growing as the medial physis closes at age 23-25 years.
Anatomy and Biomechanics
The clavicle is a subcutaneous double S-shaped bone that articulates with the sternum and the scapula via the SC and AC joints, respectively (Fig. 49.12).
The acromial end of the clavicle is more broad and flat than the sternal end.
The undersurface of the acromial end has bony projections called the conoid tubercle and trapezoid line. These projections mark the attachment sites of the conoid and trapezoid ligaments, respectively, of the coracoclavicular ligament complex.
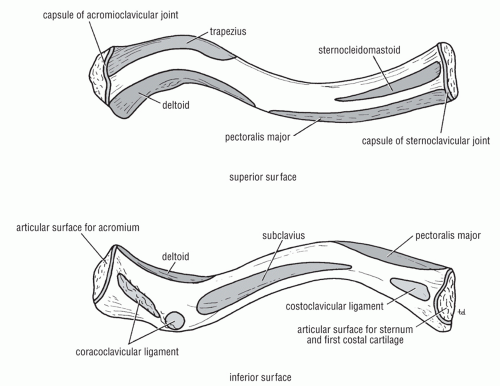
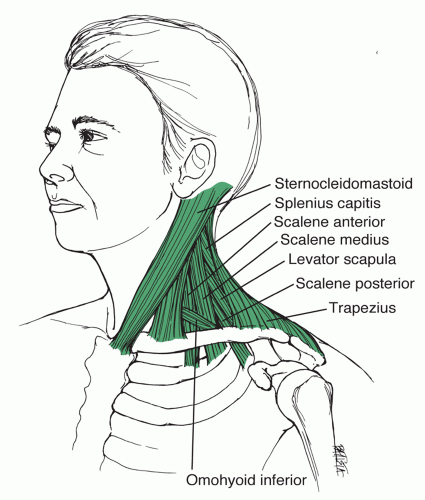
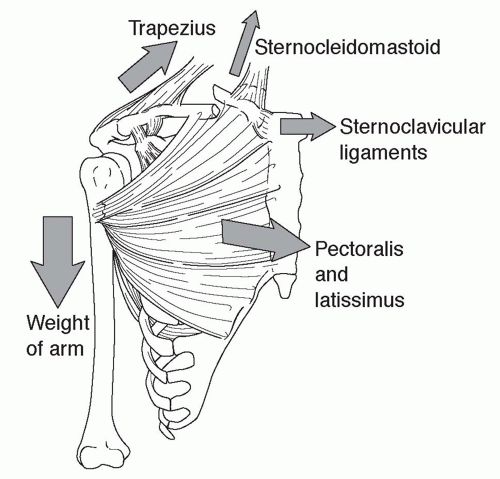
The trapezius, sternocleidomastoid, and sternohyoid muscles insert on the posterior-superior border of the clavicle (Figs. 49.13 and 49.14).
The deltoid, clavicular head of the pectoralis major, and subclavius muscles originate from the anterior inferior surface of the clavicle.
The clavicle acts as a strut that connects the upper limb to the trunk and allows the arm to hang freely.
The clavicle also functions to protect the neurovascular structures running from the neck to the arm.
Clavicle Fractures
Clavicle fractures are very common fractures, accounting for nearly 5%-15% of all fractures
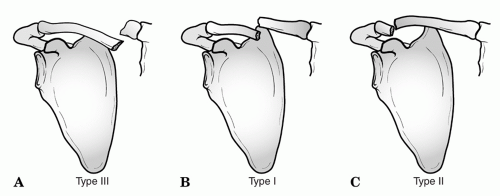
Classification
Allman (3) created the classification system that is still used today (Fig. 49.15).
□ Type I – middle third clavicle fractures
□ Type II – lateral third clavicle fractures
□ Type III – medial third clavicle fractures
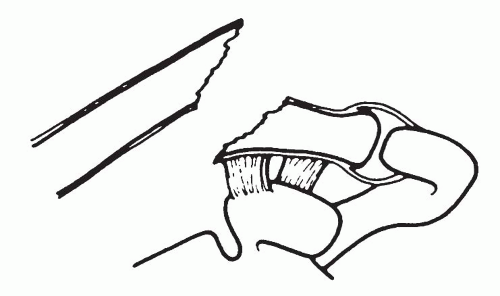
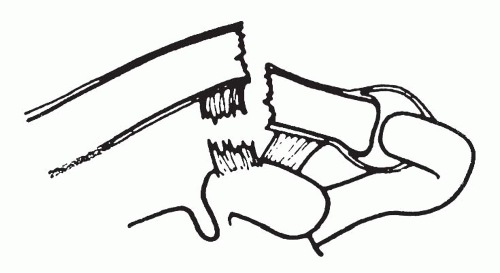
In 1968, Neer (54) further divided lateral clavicle fractures into three types.
□ Type I – lateral clavicle fracture with intact coracoclavicular ligaments (Fig. 49.16)
□ Type II – lateral clavicle fracture with torn coracoclavicular ligaments (Fig. 49.17)
□ Type III – intra-articular lateral clavicle fracture involving the AC joint, but coracoclavicular ligaments remain intact (Fig. 49.18)
Of all clavicle fractures, 80% involve the middle third of the clavicle, and 10%-15% involve the lateral third of the clavicle.
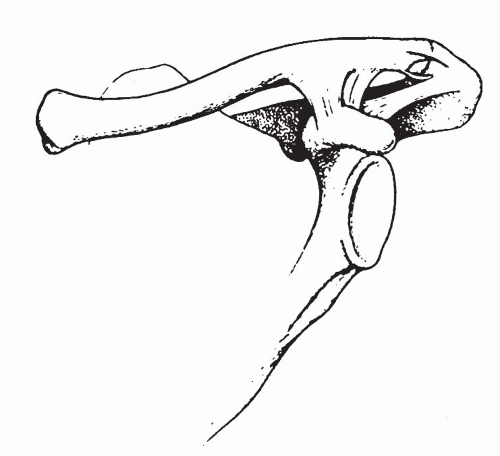
Clavicle fractures most commonly result from a fall on the lateral aspect of the shoulder, but can also result from a direct blow (Fig. 49.19).
Traditionally, clavicle fractures have been treated nonoperatively with a reported healing rate of 99% (53,70). More recent studies have shown that the clavicle fracture nonunion rate is actually higher than previously reported, at around 15%-25% (22,34,57,58).
With midshaft clavicle fractures, the medial fragment is displaced superomedially due to the pull of the sternocleidomastoid and sternohyoid muscles. The lateral fragment is displaced inferolaterally due to gravity and the pull of the deltoid, trapezius, and pectoralis major muscles (Fig. 49.20).
Physical Examination
Typically, patients present with a clear history of falling on the lateral aspect of their shoulder or having a direct blow to the clavicle.
It is important to assess the quality of the skin over the clavicle to make sure that the skin is not ischemic, open, or compromised in any way.
A complete neurovascular exam is important in order to ensure that there has been no injury to the subclavian vessels or brachial plexus.
Fractures of the clavicle may occur in isolation, but be sure to assess the scapula, humerus, and ribs for other fractures that may be concomitantly present.
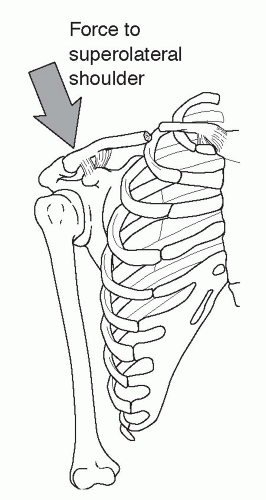 Figure 49.19: The most common mechanism of clavicle fracture is a fall on the superolateral shoulder. Since the SC ligaments are extremely strong, the force exits the clavicle in the midshaft. |
Radiologic Evaluation
Like other fractures, in order to unders and the displacement and angulation of the fracture, views in two different planes are needed (Fig. 49.21). Obtaining an AP of the clavicle and a 45-degree cephalic tilt AP usually suffice (8). Also a bilateral Zanca view can be helpful for side-to-side comparison (Fig 49.22).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree