Addressing Stage II Posterior Tibial Tendon Dysfunction
Biomechanically Repairing the Osseous Structures Without the Need of Performing the Flexor Digitorum Longus Transfer
Lawrence A. DiDomenico, DPMabc∗ld5353@aol.com, Zachary M. Thomas, DPMc and Ramy Fahim, DPM, AACFASa, aAnkle & Foot Care Centers, 8175 Market Street, Youngstown, OH 44512, USA; bSt. Elizabeth Hospital, Youngstown, Ohio; cHeritage Valley Hospital, Beaver, Pennsylvania, USA
The clinical presentation of adult flatfoot can range from a flexible deformity with normal joint integrity to a rigid, arthritic flat foot. Debate still exists regarding the surgical management of stage II deformities, especially in the presence of medial column instability. This article reviews and discusses various surgical options for the correction of stage II flatfoot reconstructive procedures. The authors discuss their opinion that is not always necessary to transfer the flexor digitorum longus tendon to provide relief and stability in this patient population. The anatomy, diagnosis, and current treatments of flexible flatfoot deformity are discussed.
Introduction
Adult acquired flatfoot deformity is characterized by collapse of the medial longitudinal arch and loss of the mechanical advantage of the posterior-medial soft-tissue structures, including the posterior tibial tendon. Key1 initially described a chronic partial rupture of the posterior tibial tendon in 1953.
Further literature confirmed an association with this abnormality and, in fact, “dysfunction” of this posterior tibial tendon with adult acquired flatfoot deformity. The clinical presentation of adult flatfoot can range from a flexible deformity with normal joint integrity to a rigid, arthritic flat foot. Conservative and surgical management of flatfoot deformity has been reviewed extensively in the literature, but debate still exists regarding the surgical management of stage II deformities, especially in the presence of medial column instability. Historically triple arthrodesis was a common surgical approach; however, the increased incidence and awareness of posterior tibial tendon dysfunction has stimulated a trend toward surgical interventions that involve joint preservation techniques.2,3
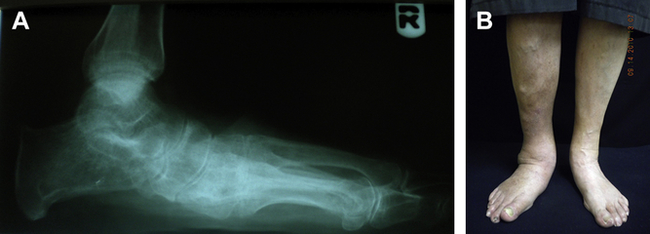
The purpose of this article is to review and discuss various surgical options for the correction of stage II flatfoot reconstructive procedures. The authors discuss their opinion that is not always necessary to transfer the flexor digitorum longus tendon to provide relief and stability in this patient population. The article focuses on the anatomy, diagnosis, and current treatments of flexible flatfoot deformity (Fig. 1).
Functional anatomy
The tibialis posterior arises from the posterior aspect of the tibia and is part of the deep posterior compartment. The tendon divides in the proximity to the navicular tuberosity into 3 slips: the anterior, middle, and posterior. The anterior slip is the largest of these, and also is the slip considered to be the continuation of the posterior tibial tendon proper. This slip inserts on to the navicular tuberosity, first cuneiform-navicular joint, and inferior first cuneiform. The middle tendon slip fans out like multiple tentacles that travel deep into the plantar vault of the foot inserting on the second and third cuneiform, lateral second metatarsal base, medial and lateral third metatarsal base, medial fourth metatarsal base, and cuboid. Occasionally there is a slip to the fifth metatarsal base. At the level of the midfoot this portion of tendon gives origin to the flexor hallucis brevis. The tendon also crosses deep to the peroneus longus and, in some instances, directly interacts with this tendon by tendinous attachment. The posterior component of the tibialis posterior travels lateral and posterior to insert on the sustentaculum tali.4 Ultrasonographic imaging of the tibialis posterior shows a mean width of 9.72 to 11.12 mm, thickness of 3.42 to 3.64 mm, and cross-sectional area of 2.66 to 3.07 mm2 based on 3 observers. Magnetic resonance imaging (MRI) shows measurements of 10.65 to 11.11 mm width, thickness of 3.95 to 4.18 mm, and cross-sectional area of 3.17 to 4.06 mm2.5
The flexor digitorum longus originates from the posterior tibia and interosseous membrane. The tendon courses under the sustentaculum tali as part of the deep posterior compartment. The tendon of the flexor digitorum longus traverses plantar to the flexor hallucis longus and travels anteriorly and laterally before it splits in to 4 slips, each inserting on their respective lesser digital distal phalanx. The tendon of the flexor digitorum longus also gives origin to the quadratus plantae.4 Ultrasonographic measurements of the flexor digitorum longus show a mean cross-sectional area of 1.59 to 176 mm2.6
The vascularity of the posterior tibial tendon originates from branches of the posterior tibial artery. Superior to the medial malleolus, the posterior tibial tendon has vessels in the synovial sheath, which come from muscle tissue. Distally the insertion receives its blood supply from the periosteal tissue. In between is a zone of hypovascularity, which often corresponds to the site of the diseased tendon.7
Pathology
Biomechanical imbalance can lead to chronic microtrauma in the posterior tibial tendon. In addition, advanced age lessens tendon elasticity because of changes in collagen structure that create tendon weakness.8 Poor blood supply may stimulate this disease process and may preclude healing of the tendon, leading to a chronic inflammatory state that creates tenosynovitis and tendinosis. Deland and colleagues9 demonstrated that medial calcaneonavicular ligaments and the interosseous ligament are often implicated in posterior tibial tendon dysfunction. Other causes include medical conditions such as ligamentous laxity and trauma to the posterior tibial tendon. More common are biomechanical conditions associated with posterior tibial dysfunction. This patient population typically presents with an equinus contracture, a medial column instability that can lead to a forefoot varus and a hindfoot valgus.
Classification
Johnson and Strom10 described 3 stages of posterior tibial tendon dysfunction, with Myerson and Bluman11 describing a fourth stage.
Stage II is characterized by an elongated posterior tibial tendon, medial pain, and a mobile hindfoot valgus that corrects to neutral on heel rise. A single-limb heel-rise test shows marked weakness. There is a positive “too many toes” sign. Stage II can also be subdivided into IIA (<30% uncovering of talar head), IIB (>30% uncovering of talar head), and IIC, which is stage II posterior tibial tendon dysfunction with associated forefoot varus (Fig. 2).

Stage III is rigid hindfoot valgus that does not correct on double-limb heel rise. The patient may not be able to perform a double-limb heel rise, and is unable to perform a single-limb heel rise. There is a positive “too many toes” sign. There may be significant rearfoot arthritis. Pain is noted medially, and also can be lateral, owing to impingement of lateral talar process.10 Extra-articular osteotomies may be attempted to treat this stage; however, serious consideration should be given to fusion of the talonavicular and/or subtalar joint (Fig. 3).
Stage IV deformities are a progression of stage III, with associated tibiotalar valgus and possible arthrosis as a result of the prolonged hindfoot valgus.11 The treatment of stage IV pes planovalgus is the same as for stage III; however, pain in the ankle joint must also be addressed by means of cautious monitoring, cartilage repair, fusion, or total ankle arthroplasty (Fig. 4).

Other classification systems that describe the disorders associated with the dysfunction of the posterior tibial tendon also exist, but are beyond the scope of this article. The reader is encouraged to consult the corresponding references for more detail.12,13
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree









