INTRODUCTION
The clinical field of sports medicine involves the care and treatment of those injured during sporting activities. Physiatrists were granted the ability to become subspecialty certified in sports medicine in 2006. In this chapter, common sport-specific injuries are discussed, with the injuries organized by sport rather than by body region (the more usual format). The chapter describes the most prevalent injuries in the most common sports, and while many of these injuries can occur among participants in various sports, to avoid repetition they are discussed once, under the most relevant sport.
CONTACT SPORTS
Contact sports are those in which participants strike or crash into one another with external force. Examples include football, rugby, and ice hockey. Athletes involved in collision sports are at a high risk for injury due to the violent nature of the competitions.
ESSENTIALS OF DIAGNOSIS
Direct or indirect force transmitted to the head.
Rapid onset of transient neurologic disturbance that resolves spontaneously.
Functional rather than structural impairment, with normal neuroimaging.
Concussions are considered mild traumatic brain injuries caused by biomechanical forces affecting the head, with symptoms improving spontaneously over time. All athletes suspected of having a concussion must be immediately removed from competition and evaluated onsite.
Immediate symptoms may include but are not limited to headaches, neck pain, dizziness, visual or auditory disturbances, loss of balance, post-traumatic or retrograde amnesia, confusion, drowsiness, difficulty concentrating, or fatigue. More objective measures, such as the Sport Concussion Assessment Tool 2 (SCAT2), aim to determine the presence of a concussion and its severity by compiling a number of acute measures.
Computed tomography (CT) imaging should be performed if loss of consciousness (LOC) lasts more than 60 seconds, with suspected skull fracture, or in the presence of any focal neurologic deficits to rule out acute subdural or epidural hematomas.
Managing concussion begins with baseline neurocognitive testing. The SCAT2 may be used to this end, though computer-based programs such as the Immediate Post-Concussion Assessment and Cognitive Testing (ImPACT) have been found to be valid and reliable and are popular on all levels of play. Once a concussion has been diagnosed, the player must be monitored for cognitive or functional decline. High school and college athletes who suffer a concussion are not allowed to return to game action on the same day; this applies to all athletes, not only football and rugby players. Physical and cognitive rest is the mainstay of initial postconcussive management. Athletes of all ages should refrain from activity until symptoms have cleared. Student athletes should refrain from activities that challenge cognition or concentration, such as texting, video game play, and test taking. ImPACT continues to be administered at predefined intervals until the athlete has returned to baseline.
There are no standardized return-to-play (RTP) guidelines. Following a period of rest and once all postconcussive symptoms have completely abated, athletes are placed under a five-phase RTP protocol; if each phase lasts the expected 24 hours, athletes can be game ready by the next weekend. However, progression may only occur if the athlete remains symptom-free. If not, he or she must return to the previous day’s activity until asymptomatic and may have to rest and begin the cycle again if symptoms persist. Phase 1 includes light aerobic activity, phase 2 entails sports-specific coordination exercises, phase 3 involves higher level training drills, phase 4 is when full-contact practice may ensue, and phase 5 is return to competition given that all previous days were free of any concussive symptoms.
ESSENTIALS OF DIAGNOSIS
Valgus stress to an externally rotated tibia (typically on a planted foot).
Positive Lachman test.
The typical mechanism of an anterior cruciate ligament (ACL) injury is a valgus force applied to an externally rotated femur on a planted foot. More than twice as many injuries occur during games than in practice and more take place on turf than on natural grass. In the English Professional Rugby Union, ACL injuries accounted for 29% of all days lost to knee injury. Women sustain ACL tears at a much higher rate than men, and their tears are more often due to noncontact injuries.
Players often hear a “pop” and suffer immediate pain with full-thickness tears. They may also complain of the knee “giving way.” Hemarthrosis usually forms within hours of the injury, so the optimal time to examine the injured knee is within the first hour postinjury or after swelling has somewhat abated and the athlete no longer guards the injured knee. The Lachman test is the most sensitive physical examination maneuver to assess the integrity of the ACL.
Plain radiographs should be taken to look for a Segond fracture, which is an avulsion of the lateral tibial plateau. Magnetic resonance imaging (MRI) can be used not only to evaluate the ACL itself, but also to determine the presence of concomitant injuries, which are common.
Initial management of ACL tears involves rest, ice, hinged bracing, crutch ambulation until weight bearing is tolerable, and early range of motion (ROM). Isometric strengthening exercises are important to prevent contracture and to lessen arthrogenic muscle inhibition of the quadriceps. In the athletic population, surgery is the suggested intervention. Grafts range from bone–patellar–bone and hamstring autografts to patellar tendon allografts. Aggressive rehabilitation has been advocated for all athletes before and after surgery. The most important aspect of the preoperative phase of rehabilitation is restoration of full extension to maximize long-term functional outcome.
In the immediate postoperative phase, from 0 to 2 weeks, athletes are transitioned to partial or full weight bearing, depending on the presence of additional injuries and repairs. Bracing is optional but generally used. In this initial phase, extension to 0 degrees is again critical, and leg strengthening should reach at least 4+/5 in the quadriceps and 5/5 in the hamstrings. Phase 2 lasts 2–12 weeks and should focus on knee hyperextension, flexion to 130 degrees, proprioception and balance control, and unhindered walking. Phase 3, from 3–6 months postsurgery, maximizes balance, flexibility, proprioception, and begins targeting running and sport-specific drills. The final phase is RTP. Athletes should not return to competition until they have reached 90% strength in the injured leg compared with the uninjured leg and can perform all full-speed and full-intensity maneuvers necessary for their position.
The most common complications of ACL reconstruction include quadriceps weakness, knee flexion contracture, and anterior knee pain due to patellofemoral instability. There is also a 5% risk of graft failure (Figure 29–1).
ESSENTIALS OF DIAGNOSIS
Medial Collateral Ligament Tear
Force to the lateral knee, usually when in flexion.
Pain on valgus stress test.
Lateral Collateral Ligament Tear
Force to the medial knee.
Pain on varus stress testing.
Tears to the medial collateral ligament (MCL) occur most often with a direct valgus blow to a flexed knee when the foot is planted. In the English Professional Rugby Union, 25% of all days lost to knee injury were a result of MCL tears. The lateral collateral ligament (LCL) of the knee is very rarely injured in isolation, and tears are more often associated with other structural damage.
Using the valgus stress test, the examiner elicits pain but finds no laxity in a grade I MCL injury; finds some laxity with a clear end point in grade II; and notes gapping of the medial joint without a clear end point (indicating complete disruption of the ligament) in grade III. LCL tears are graded similarly to those of the MCL, but diagnosis is made by testing for varus laxity.
Radiographs should be obtained to rule out epiphyseal or occult fractures. The use of MRI for evaluation of MCL sprain is only indicated when other injuries are suspected. However, in LCL sprains, an MRI scan is indicated for confirmation because an avulsion of the biceps femoris tendon or ACL tear can cloud the diagnosis.
Isolated MCL tears very rarely require surgery; rather, they are treated with a hinged brace for up to 6 weeks, depending on the grade. Conservative treatment for MCL injuries requires a stepwise, multiphase rehabilitation program over 4–6 weeks. It is imperative that all therapy be prescribed and tailored on an individual basis, as no universal algorithm can apply to all athletes.
Treatment of isolated LCL tears consists of conservative management in a manner similar to that for MCL injuries. Although high-level athletes may opt for early surgical repair, one cohort study of isolated grade III LCL tears in National Football League (NFL) players showed faster RTP and more optimal long-term outcomes in those treated nonoperatively. In LCL injuries, surgery is the treatment choice in athletes with multiligament or complex structural injury.
Flexion–extension braces can be worn during competition to help minimize the incidence of recurrent MCL and LCL sprains and tears; however, there is no evidence for their overall efficacy.
ESSENTIALS OF DIAGNOSIS
Rotational force against the knee, with the foot stationary.
Physical examination findings have low sensitivity.
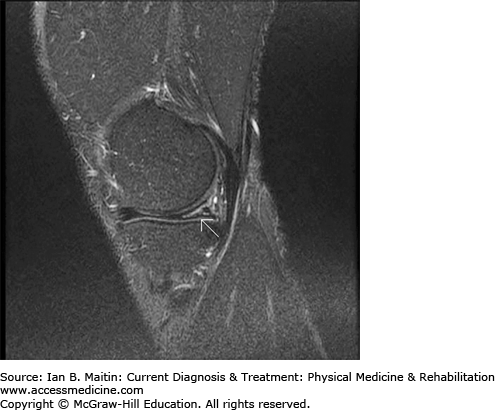
The menisci are most commonly injured in football players, acutely, when a rotational shear force is applied to a planted foot. Tears are also caused by long-term repetitive stress on the knee. In a study of NFL players, 17.3% of participants were found to have sustained a full-thickness meniscal tear (Figure 29–2). Further information regarding meniscal injuries can be found in Chapter 30.
ESSENTIALS OF DIAGNOSIS
Trauma to and pain over the iliac crest.
No evidence of injury on radiographs.
Any blow to the iliac crest or fall on a hard surface can cause a contusion to the bone, known as a “hip pointer.” The primary symptom is isolated pain over the iliac crest, with no evidence of osseous injury on radiographs. Rest, ice, nonsteroidal antiinflammatory drugs (NSAIDs), ROM exercises, and strengthening of the muscles of the hip and pelvic girdle are mainstays of treatment. Padding of the iliac crest and gluteus muscles during competition is the only preventative measure. RTP is allowed when the athlete can tolerate the discomfort and can perform all sport-specific activities under full competitive conditions.
ESSENTIALS OF DIAGNOSIS
Direct trauma to anterior thigh.
Pain and swelling over the quadriceps.
Quadriceps contusions can occur when a player sustains direct trauma to the anterior thigh, as occurs in blocking and full-contact collisions.
Pain and swelling over the anterior thigh and decreased ROM are the most common presenting symptoms of quadriceps contusion. Using the Jackson and Feigin classification, quadriceps contusions can be differentiated as mild, moderate, or severe based on ROM and gait patterns (Table 29–1). Imaging is not usually necessary.
Immediate management of a quadriceps contusion requires immobilization of the knee joint in flexion, with ice and compression for 24 hours postinjury to decrease hematoma formation. Functional rehabilitation begins once pain-free ROM has returned and can be advanced based on the athlete’s tolerance and overall improvement. RTP is dependent on the player attaining a fully functional knee with ROM to at least 120 degrees and the ability to perform all sport-specific activities. The use of NSAIDs has been advocated to help prevent myositis ossificans, which is a potential long-term complication of hematoma formation from a contusion.
ESSENTIALS OF DIAGNOSIS
Appropriate mechanism of injury (most commonly, collision with the shoulder abducted and externally rotated, fall on a hyperflexed arm, or blow to the shoulder in slight adduction).
Prominent humeral head and loss of normal shoulder contour.
The shoulder accounts for a large proportion of injuries, with dislocations being the most severe in terms of time missed from competition. Dislocations occur most often in the anterior direction (Table 29–2). Three mechanisms of anterior dislocation have been described in rugby and football players. The most prevalent mechanism involves a tackle with the shoulder abducted and externally rotated. Other mechanisms, in order of frequency, are a fall on a hyperflexed arm, and a blow to the shoulder in slight adduction.
| Direction of Dislocation | Mechanism of Injury | Clinical Findings | Associated Injuries |
|---|---|---|---|
| Anterior | Tackle or fall on an extended, abducted, and externally rotated arm Fall on a hyperflexed arm Blow to the shoulder with the arm in slight adduction | Loss of shoulder contour Prominent humeral head Sulcus below the acromion Possible loss of sensation over the lateral shoulder (axillary nerve) +/− Pain | Bankart lesion Bony Bankart lesion Hill–Sachs lesion |
| Posterior | Direct blow to or fall on an internally rotated and adducted arm | Pain with loss of external rotation Abnormal shoulder contour | Reverse Bankart lesion |
| Inferior | Fall on an abducted and externally rotated arm | Shoulder locked at 90 degrees of abduction Severe pain | Same as anterior dislocations |
Athletes who suffer traumatic anterior dislocations on the field instantly manifest loss of normal shoulder contour, a prominent humeral head, and a sulcus below the acromion. Pain may or may not be present. Testing of sensation to light touch over the lateral arm and of deltoid strength must be done immediately to check for injury to the axillary nerve, which is a potential serious complication. Radiographs of a dislocated shoulder should be obtained prior to reduction, as a fracture may be present and reduction could aggravate the break. However, given that most reductions occur on the field rather than in an emergency department setting, postreduction films are indicated.
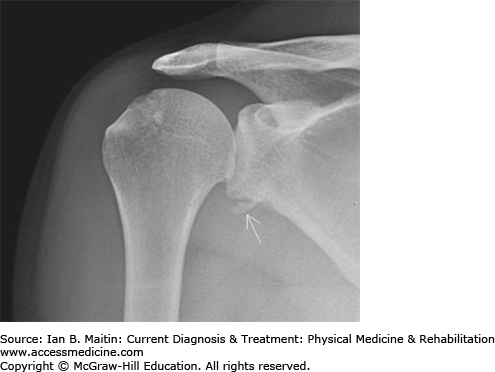
There is no standard technique for shoulder reduction. The athlete may be able to self-reduce; alternately, the medical staff may use counter-traction or weight-assisted reduction on the sideline or in the emergency department, with conscious sedation if needed. A postreduction sling can be used for patient comfort, if needed. Recent evidence supports primary surgical stabilization in players younger than 25 years of age owing to the high rate of recurrence. Prior to surgery, MRI is performed to evaluate the glenohumeral ligaments and for secondary associated injuries. Detachment of the labrum from the anterior glenoid margin, called a Bankart lesion, is normally repaired during arthroscopic stabilization of the shoulder (Figure 29–3). A fracture of the glenoid rim is termed a bony Bankart, and a Hill–Sachs lesion is a compression fracture of the posterior humeral head that occurs as it is displaced from the glenoid fossa. The most common surgical procedure is a labral Bankart repair. Full RTP can take up to 3 months.
ESSENTIALS OF DIAGNOSIS
Posterior dislocation: internal rotation and adduction of the shoulder.
Inferior dislocation: external rotation and abduction of the arm to 90 degrees.
Glenohumeral dislocations are much less common in the posterior direction than in the anterior direction, and inferior dislocations occur in only about 1% of all traumatic dislocations (see Table 29–2). A posterior dislocation results from a direct blow to or fall on an internally rotated and adducted arm. An inferior dislocation, also termed luxatio erecta, occurs with a fall on an abducted and externally rotated arm.
An athlete with a posterior dislocation has loss of contour of the anterior shoulder, with pain and loss of external rotation. An athlete with an inferior dislocation has extreme pain because the humeral head is locked beneath the glenoid, preventing both adduction and internal rotation. Radiographs should include anterior–posterior, lateral, Y, and axillary views, although the latter may not be possible because of patient discomfort.
Forward traction and pressure on the humerus is necessary to relocate posteriorly dislocated shoulders. Reduction of inferiorly dislocated shoulders is a two-step process that should be done in an emergency or clinical setting under conscious sedation because of severe pain during reduction. Guidelines for MRI and surgical management are similar to those for anterior glenohumeral dislocations (see earlier discussion).
ESSENTIALS OF DIAGNOSIS
Pain over the acromioclavicular joint.
Physical findings consistent with type I–VI injury, using the Rockwood classification.
The acromioclavicular joint (ACJ) is a synovial joint formed by the acromion of the scapula and the distal end of the clavicle. Injuries to the ACJ have been reported to account for 41% of shoulder injuries in football and 32% of shoulder injuries in rugby, the highest percentage of any shoulder pathology. The usual mechanism of injury during football or rugby is a direct hit from one player to another.
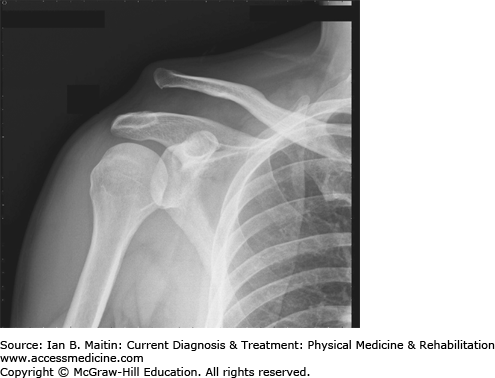
The joint has dynamic and static stabilizers, the most important in terms of separations being the joint capsule, the coracoclavicular (CC) ligament, and the acromioclavicular (AC) ligament. The Rockwood classification uses the disruption of these structures as the basis for six different types of ACJ injury. Type I involves sprain of the joint capsule and the AC ligament, with tenderness over the joint itself; type II involves complete tearing of the capsule and AC ligament, sprain of the CC ligament, and a palpable step-off from the clavicle to the acromion; type III involves complete tears of the capsule, AC ligament, and CC ligament and a visual step-off, with elevation of the clavicle up to 100%; type IV involves posterior dislocation of the clavicle; type V involves greater than 100% elevation of the clavicle; and type VI involves inferior dislocation of the clavicle (Figure 29–4). In one study of National Collegiate Association of America (NCAA) football players, 96.4% of ACJ injuries were type I or II. Weighted radiographs show the level of clavicular displacement and aid in grading of the injury.
Management depends on the type of injury and is described in detail in Chapter 30. Conservative treatment is indicated for type I, II, and III separations; and surgical repair for types IV, V, and VI, and type III separations that do not respond to therapy. The phases of therapy include acute, recovery, and RTP. Return to competition often occurs after 2–4 weeks for type I separations, 4–6 weeks for type II, and 6–8 weeks for type III.
ESSENTIALS OF DIAGNOSIS
Sudden forced flexion of an extended distal interphalangeal (DIP) joint.
Pain and swelling in the finger with inability to extend the DIP joint.
The terminal extensor mechanism of the finger crosses the dorsal aspect of the DIP joint and is essential for full active extension of the digit. In ball sports, the ball can strike and forcefully flex an extended fingertip, causing the extensor tendon to snap or an avulsion fracture of the tendinous attachment at the distal phalangeal base. This disruption of the extensor mechanism is called a “mallet finger.” In football, wide receivers are at particular risk for this injury when attempting to catch a pass.
Most mallet injuries involve the middle finger, although the injury can occur in any digit, including the thumb. Athletes present with pain and swelling, tenderness over the distal phalanx, and an inability to actively extend the DIP joint. Radiographs may show a small avulsion fracture, which is only significant if more than one third of the joint is involved.
Treatment consists of splinting of the injured digit in slight hyperextension for 6–8 weeks, and compliance is essential. Any flexion of the DIP joint will disrupt healing and put the athlete at risk for recurrent injury or longer absence from play. Rapid RTP is only possible if there is no risk of disrupting the splinted finger. However, because of the importance of all finger movements in football and rugby, especially among the skill positions and in tacklers, cessation of competition until full healing is achieved is often indicated. RTP may occur once pain-free active extension of the DIP joint has been achieved after a full course of splinting. The splint must continue to be worn during all sporting activity and at night for an additional 6–8 weeks. Throughout the course of treatment and RTP, the proximal interphalangeal joint should remain mobile, and skin breakdown should be prevented.
ESSENTIALS OF DIAGNOSIS
Pain and swelling in the finger with an inability to flex the DIP joint.
History of a tackling or grabbing injury.
When football or rugby players tackle or grab an opponent’s jersey, they are at risk for disruption of the flexor digitorum profundus from the distal phalangeal base, an injury termed a “jersey finger.” Seventy-five percent of these injuries involve the fourth digit. The athlete presents with pain and swelling over the volar aspect of the finger, often with the digit in extension. There may be tenderness over the full length of the flexor digitorum profundus, and the athlete will not be able to actively flex the DIP joint with isolation of the tendon. The flexor digitorum superficialis should also be evaluated.
Surgery is indicated to repair the disrupted flexor digitorum profundus tendon, and early intervention within 7–10 days improves outcome. Postoperative hand rehabilitation with a focus on flexor stretching to decrease long-term stiffness is essential for full recovery. Return to tackling sports is not usually allowed until at least 3 months after surgery.
ESSENTIALS OF DIAGNOSIS
Pain at the base of the first digit.
Radiographs may show a fracture.
Partial or complete ulnar collateral ligament (UCL) tears account for 86% of all traumatic thumb injuries. A fall on an outstretched arm with an abducted thumb or clutching a ball while falling to the ground may produce a disruption of the UCL of the thumb. This injury is also commonly seen in skiers who suffer a valgus stress to an abducted thumb while holding a pole during a fall.
The athlete presents with pain, swelling, and tenderness over the ulnar aspect of the base of the thumb and the first MCP joint. There may also be ulnar deviation or subluxation of the proximal phalanx. Radiographs must be obtained to determine whether an avulsion fracture is present, but should be obtained prior to physical examination to decrease the risk of worsening an unknown break. When no end point is felt on valgus testing, a complete tear is deemed present. If the UCL displaces proximally, the adductor aponeurosis of the adductor pollicis may slip between the torn ligament and the bone, thereby preventing healing. This abnormality, termed a Stener lesion, should be suspected in any athlete with a displaced avulsion fracture visible on plain radiographs.
Conservative management with a thumb spica splint or thermoplastic casting for 4 weeks is the treatment of choice for partial tears of the UCL. Complete tears with no end point on valgus stress or displaced avulsion fractures necessitate surgical repair. Regardless of management, athletes may return to competition if their position allows use of a splint or cast, such as offensive or defensive linemen in football. Once the thumb has regained full strength with normal pain-free ROM, athletes may return to full competition without splinting or casting. For partial tears this generally occurs after about 4 weeks; complete tears take about 3 months, regardless of whether surgery was performed.
Frequent accelerations and decelerations, changes in direction, and the overall force produced by full-body hitting and checking at high velocities place ice hockey players at a high risk for injury. Many of the injuries discussed earlier in the football and rugby section, particularly concussions, glenohumeral dislocations, and AC joint separation, are also prevalent in hockey. In this section, additional injuries not specific to but seen quite often in the sport are examined.
ESSENTIALS OF DIAGNOSIS
Nonspecific groin or lower abdominal pain, or both, with tenderness over the pubic tubercle.
Positive MRI findings involving the pubic bone and soft tissues.
The differential diagnosis for groin and lower abdominal pain is vast. It includes but is not limited to femoroacetabular impingement, arthritis, and labral tears; lumbar stenosis or disc herniation; adductor tendinopathy or rupture; muscle strains or contusions; osteitis pubis; pelvic stress fractures; iliopsoas tendinopathy; and athletic pubalgia, often referred to as a “sports hernia.”
Some physicians argue that athletic pubalgia is an umbrella term referring to myriad potential diagnoses, with sports hernia as only one subset. Meyers and colleagues characterized the injury as a hyperextension injury, which results when the pubis serves as a pivot point of insertion for the rectus abdominis and adductor longus muscles. The injury results in disruption of the conjoined tendon of the adductor longus and rectus abdominis, leading to degeneration arthropathy of the pubic symphysis.
For the purposes of this discussion we have opted to view athletic pubalgia and sports hernia as the same entity: a spectrum of potential muscular, fascial, tendinous, and aponeurotic disruptions—including those of the rectus abdominis and adductor longus aponeurosis and insertions, the external obliques, the interface between conjoined tendon and rectus abdominis, and the muscles that form the conjoined tendon (internal obliques and transversus abdominis)—that presents as nonspecific lower abdominal or groin pain, or both. Athletic pubalgia is seen most often in athletes who perform repetitive bending and twisting, such as soccer and hockey players (“hockey groin”), which leads to either one larger tear or many microtears in the structures listed.
Athletes present with lower abdominal and groin pain that worsens with exercise and improves with rest. Most players can pinpoint a specific inciting event, although onset is often insidious. The pain is typically, though not always, unilateral; may radiate to the perineum, thigh, or scrotum; and is worse with cutting, twisting, turning, kicking, sit-ups, and activities involving a sudden Valsalva maneuver.
Examination should include evaluation of adductor-, iliopsoas-, and abdominal muscle–related pain and strength at the pubic symphysis. Patients usually report tenderness at or above the pubic bone on or near the insertion of the rectus abdominis or adductor longus muscle. A subset of patients may have point tenderness at the external inguinal ring or a dilated superficial inguinal ring. Patients may also have pain at the pubic tubercle and symphysis. Unlike an abdominal or inguinal hernia, a sports hernia has no palpable defect or bulge on palpation.
Provocative testing with resisted sit-ups and resisted adduction with the hips in external rotation may reproduce groin pain. Additionally, the following five signs and symptoms have been identified as clues in diagnosing sports hernia: (1) deep groin or lower abdominal pain, (2) pain with activity such as kicking, (3) palpable tenderness over the pubic ramus at the insertion of the rectus abdominis and conjoined tendon, (4) pain with resisted hip adduction at 0, 45, or 90 degrees of hip flexion, and (5) pain with resisted abdominal curl-ups. The pain may be elicited with a resisted sit-up or resisted hip flexion when supine or with bending forward when standing. A full evaluation of the hip joint, lumbosacral spine, abdomen, adductor and iliopsoas tendons, and pelvis must be done to rule out other conditions.
Radiographs of the hip and pelvis are standard to rule out stress fractures, impingement, or other bony pathology. If a sports hernia is suspected, an MRI with a special protocol is indicated. MRI findings can diagnose sports hernia is 68% of cases. Findings can vary based on the injury, but there is typically tearing of the rectus abdominis–adductor aponeurosis and bony edema of the pubic symphysis. The presence of a T2 hyperintense area at the anterior subcortical region of the bone, 1–2 cm lateral to the symphysis, is indicative of rectus abdominis insertional pathology. Other findings on MRI may include a more intense and linear configuration, reflecting a stress response or early stress fracture 5–15 mm lateral to the pubic symphysis. Often a fluid or near-fluid signal is present within the pubic symphysis. The combination of these and previously mentioned findings represents injury at the lateral edge of the rectus abdominis and adductor aponeurosis. MRI findings can diagnose sports hernia is 68% of cases.
Dynamic ultrasound can also be used to visualize posterior inguinal wall deficiency. Ultrasound studies will show abnormal ballooning of the posterior wall when the patient is asked to strain.
Management for in-season athletes with a sports hernia begins with a period of rest, ice, NSAIDs, and possible corticosteroid or platelet-rich-plasma injections to the insertion of the rectus abdominis or adductor longus muscle. In some instances, the injury is self-limited.
After 4 weeks in which only closed-chain lower limb exercises are allowed, the athlete is put through a sport-specific functional assessment to determine whether pain-free RTP is possible. If the pain has not dissipated, the player is allowed to return to competition if he or she can tolerate the discomfort and perform at a high level. There is no evidence that competing through pain worsens the abdominal wall defect or surgical outcome. A full course of physical therapy is attempted prior to surgical referral, which is often sought many months after initial onset of symptoms.
If pain persists after a period of rest, surgical treatment should be considered; this consists of unilateral or bilateral reattachment of the rectus. Surgical techniques include both laparoscopic and open procedures and are dependent on the surgeon’s preference and on the exact nature of the MRI findings. Patient satisfaction after surgery ranges from 77% to 100%.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree