Chapter 15 Sports Medicine
Participation in athletics is both an enjoyable pastime and a part of keeping physically and mentally fit. Some individuals may only be interested in general conditioning and weight loss (Table 15-1). Others may want specific exercises for certain events. Regardless of the activity, risks are always involved, and today’s physician must be able to not only treat the various injuries that arise but also offer counsel on a wide range of other interrelated subjects, such as technique, training, and injury prevention. If the participants are children, other responsibilities are necessary. The physician should help make certain that realistic goals are set and that the activity is enjoyed by those who take part in it. Parents and coaches should be reminded that success is measured not necessarily just by winning but by the enjoyment and the amount of effort put forth. Whenever team sports are involved, all members should be allowed to play, and attempts should be made to match size and physical maturity as closely as possible. Children should learn how to play the various games as well as how to follow their rules. They should be properly supervised and should not be encouraged to play with pain. The role of the coach should be to instruct and supervise and not to give medical treatment or advice. Treating athletes is also somewhat different than treating other patients in that many of them, whether young or adult, are unwilling to simply give up playing when injuries arise. Many of them may accept a more physically tolerable substitute activity, however.
Table 15-1 Calories Expended in Common Activities*
| Activity | Calories per Hour |
|---|---|
| Light housework | 120 |
| Walking | 250–300 |
| Golf | 300 |
| Singles tennis | 480 |
| Bicycling | 450–500 |
| Jogging | 600 |
| Swimming | 650–700 |
* To be effective, an exercise should be performed three to five times per week for at least 30 to 60 minutes each time.
Prevention of Injuries
CONDITIONING
Proper conditioning means the development of strength, endurance, cardiovascular fitness, power, and flexibility. It also includes the development of proper body mechanics, form, and agility. The exact skill training depends on the specific sport involved, but lower extremity injuries can generally be lessened by strengthening exercises for individuals with loose joints to protect against ligament damage and stretching exercises for individuals with tight joints to avoid muscular strains. Staying in shape during the off-season may involve running stairs and jogging in place at home.
WARMING UP
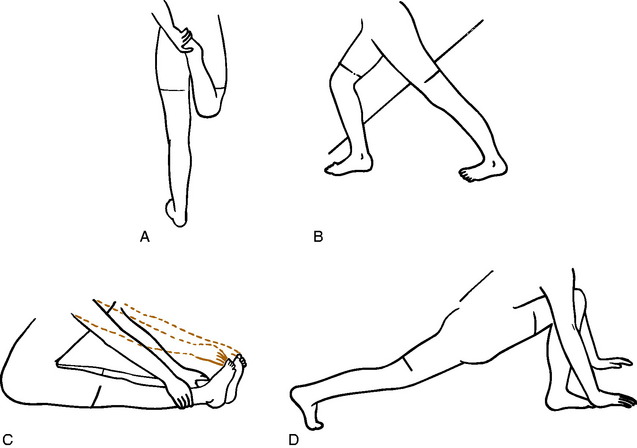
Beginning any activity gradually reduces the incidence of injury, especially injury to the muscle–tendon unit. Stretching is especially important to avoid strain. Flexibility is often diminished after a long period of inactivity, and stretching is particularly important when resuming a sport. The heel cord, hamstrings, and quadriceps should have special attention (Fig. 15-1). Tissue stretches better when warm. Therefore, stretching is best performed after slow jogging or walking for 5 minutes. Two types of stretching exercises may be performed. Static stretching is a slow, gradual stretching through full movement and holding at the position of maximum stretch for 10 to 20 seconds before relaxing. A pulling sensation, not pain, should be felt. Ballistic stretching, which involves rapid, repetitive movements, is also occasionally used but is generally less effective and may even cause minor muscular tears. It is usually not recommended.
Injuries to Muscles
MUSCULAR TEARS
Pain that develops acutely from violent activity is usually the result of a muscle tear. This may be partial or complete and may even involve the fascia. Muscles that cross two joints, such as the hamstrings, seem to be the most vulnerable. The diagnosis is usually not difficult, although it may not be easy to differentiate complete from incomplete ruptures. Sudden onset of pain, swelling, and marked local tenderness are characteristic. Pain is increased by stretching the affected muscle unit. Complete rupture may reveal a palpable defect on examination, but swelling often makes it difficult to diagnose a complete tear.
CONTUSIONS
Muscular bruises are common in all athletic events, even in the so-called noncontact sports. They are differentiated from ruptures and strains because function remains after the injury, and the contusion usually results from direct trauma. The thigh and upper portion of the arm are most commonly involved. The diagnosis is usually not difficult. Tenderness is present at the site of injury, and there is usually ecchymosis, although it may not appear until later. Treatment is directed at avoiding the complications of myositis ossificans and contractures and returning the athlete to full, pain-free competitive activity. This is accomplished by the rapid application of ice to the affected area to control bleeding and the removal of the athlete from further competition. Crutches may be necessary for the lower extremity injury, and complete bed rest with elevation of the extremity may even be indicated to control swelling and pain. A compression wrapping is helpful in early stages. After 24 to 48 hours, gentle isometric muscle contractions may be started, and active gentle range of motion is gradually added at the patient’s tolerance. Passive range of motion should be avoided. Any increase in pain or swelling is an indication to resume complete rest and application of ice. Full strength and complete flexibility are gradually restored by exercise. Reinjury is avoided by allowing complete healing to occur before returning to activities and by appropriately protecting the injured site. A return to athletics should follow only complete recovery.
MYOSITIS OSSIFICANS (OSSIFYING HEMATOMA)
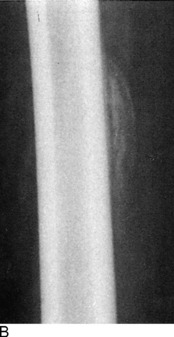
The roentgenographic diagnosis can usually be made 2 to 4 weeks after the contusion. Plain radiographs are usually sufficient. The initial appearance is that of a poorly defined opaque mass in the soft tissue adjacent to the bone (Fig. 15-2). As the mass matures, it becomes more clearly outlined and dense. The lesion usually stabilizes in 3 to 6 months and begins to resorb slowly, often without any disability. Eventually, it transforms itself into mature bone and is partially resorbed. Radiographic maturity is usually reached in about 6 months.
FASCIAL HERNIAS
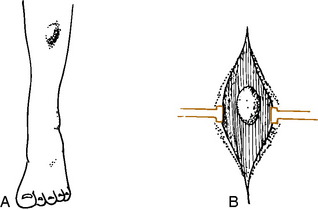
These hernias often develop as a result of a simple contusion or small puncture wound that causes a rent to develop in the fascia and aponeurosis that envelops all muscle. Often, however, there is no history of trauma. The defect may vary in size, the smallest being 1 cm. Hernias may also develop in weak fascial areas in patients with chronic compartmental syndromes as a result of increased pressure in the compartment. They are also seen where nerves emerge from the fascia. Examination will reveal a palpable “tumor” mass, especially when the muscle is relaxed (Fig. 15-3). Muscle contraction may cause the mass to disappear, and direct pressure also “reduces” the mass. There may be numbness in the foot if the hernia protrudes through a neural foramen.
Injuries to Runners
BIOMECHANICS
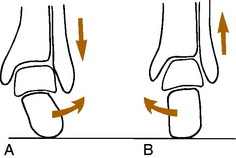
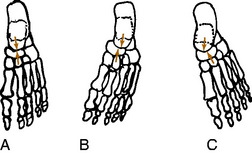
The running gait pattern is a repetitive movement that consists of a support phase, when the foot is on the ground, and a nonsupport phase. It is during the support phase that most injuries develop. Distance runners usually begin this phase by landing on the heel (sprinters usually land on the forefoot). As weight is taken on the heel, the calcaneus will begin to roll laterally (pronate, evert) under the talus at the subtalar joint (Fig. 15-4). This allows the heel to absorb shock and adapt to the underlying surface. The forefoot follows this motion by pronating, and at the same time, the tibia begins to rotate internally in proportion to the amount of heel pronation. As the weight moves forward, the calcaneus begins to supinate (invert) or roll back medially under the talus, and the tibia begins to externally rotate. This allows the foot to become more rigid and gives the heel cord a strong lever on which to act and transfer power. There are also a number of other coordinated motions that occur in the pelvis, hip, and other joints throughout the gait cycle, but understanding the subtalar joint mechanics is the most important.
EXAMINATION
In the supine position, the true leg lengths are measured between the anterior superior iliac spines and the medial malleoli. Discrepancies of 0.5 to 1.0 cm may be significant in the runner and require correction by a shoe lift. The range of motion of the hips is then determined. Internal and external rotation should be within 30 degrees of each other. Marked external rotation may cause an out-toed gait. The knee is closely examined, especially if patellar pain is present, and the Q angle is determined (Fig. 15-5). Patients with high Q angles may develop knee pain with running. The range of motion of the ankle is then determined with the knee extended. Fifteen degrees of dorsiflexion is normal. Any tightness of the heel cord is noted.
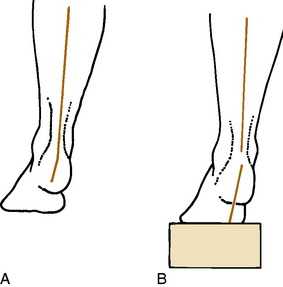
The patient then kneels on the examining table, and leg–heel and heel–forefoot alignments are determined. First, the neutral position of the subtalar joint is found by everting and inverting the foot and finding the point where the head of the talus is placed in the navicular and is no longer palpable (Fig. 15-6). This may require a little practice and is often only a rough estimate. Next, leg–heel alignment is determined by drawing lines posteriorly that bisect the lower portion of the leg and calcaneus (Fig. 15-7). The lines should be parallel or have no more than 2 to 3 degrees of varus. Heel–forefoot alignment is estimated by observing the relationship of the calcaneal line to the plane of the metatarsal heads. Normally, these lines should be perpendicular.
BACK, HIP, AND THIGH PAIN
Stress fractures occasionally occur in the pelvis and femur of the distance runner (Fig. 15-8). They should be ruled out in all cases of chronic pain that fail to respond to routine symptomatic management. The appropriate roentgenographic study should include a bone scan if the diagnosis is uncertain. As with other stress fractures, reduction of activity is usually curative, but fractures of the femoral neck may require internal fixation.
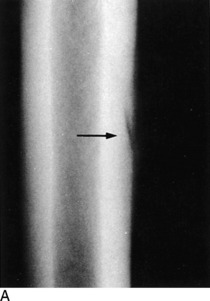
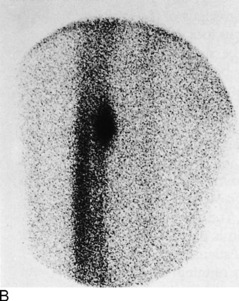
Fig. 15-8 Stress fracture of the femur (arrow). A, Plain anteroposterior (AP) roentgenogram. B, Bone scan.
Hamstring strains are a less common cause of disability in the distance runner than in the sprinter. They are treated as previously described. Stretching exercises are important not only because they can prevent local injuries but also because tight hamstrings may cause excessive lumbar lordosis that adds strain to the back when running. Rather than strain the hamstring, the sprinter whose apophyses are not closed may occasionally avulse the ischial tuberosity instead. If there is delay in assessment, the avulsed fragment may enlarge as it heals, causing a palpable fullness on clinical examination and bony enlargement on radiographic evaluation (Fig. 15-9). Unless the injury is acute and the athlete is highly competitive, treatment is symptomatic only. The fragment usually shrinks over time, but some of it may persist indefinitely.
KNEE PAIN
OVERUSE SYNDROMES
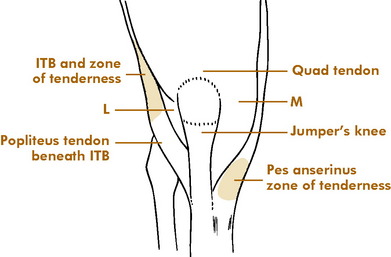
Major injuries of the meniscus or ligaments are uncommon in the knees of runners. More frequent are overuse disorders that develop because of the repetitive nature of running (Fig. 15-10). Several areas are commonly affected:
ANTERIOR KNEE PAIN SYNDROME (PATELLOFEMORAL PAIN SYNDROME)
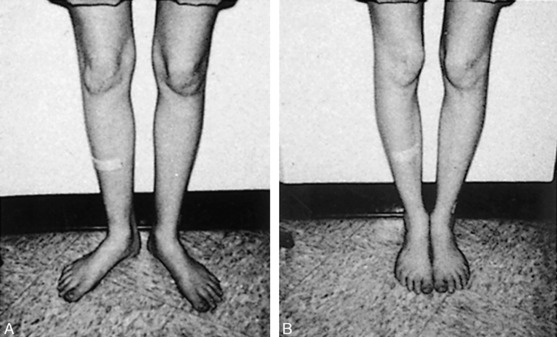
This is a condition in which pain develops beneath or, more commonly, around the patella (see Chapter 11). It is sometimes seen in conjunction with varying amounts of fibrillation and degeneration of its articular cartilage (chondromalacia), although the relationship of this to symptoms has not been established. The diagnosis is usually one of exclusion (e.g., meniscus injury, jumper’s knee). Anything that adversely affects the normal “tracking” of the patella in its femoral groove may lead to pain, often on the lateral side. The causes are frequently multifactorial: (1) an increased Q angle with a bowstringing effect; (2) tightness of the lateral retinaculum with relative weakness of the vastus medialis muscle; (3) patellofemoral malalignment, sometimes with subluxation; (4) direct trauma; (5) simple overuse; and (6) malalignment of the extremity (Fig. 15-11).
The wide variety of treatments used to manage this condition attests to the difficulty in curing it. Conservative measures such as rest, anti-inflammatory medication, local heat, stretching exercises, quadriceps exercises in extension, and avoiding the offending activity are useful. Many patients benefit from a referral to a physical therapist. Patellar straps or braces seem to be of only limited benefit. Although arthroscopically shaving the fibrillated articular cartilage has been a common surgical intervention, the results are often inconsistent, probably because the changes in the articular cartilage are not the source of pain. If a distal malalignment problem is present, an orthotic device in the shoe may occasionally be advised to help correct the tracking problem, mainly on empiric grounds. As a last resort, a surgical procedure to realign the patella sometimes eliminates the symptoms, but it would seem difficult to justify such a major operation simply to allow continued running. Despite the frustrating nature of the condition, however, most patients do well with a home exercise program.