Fig. 8.1
Sagittal and coronal computed tomography (CT) reformations of the thoracic spine. The arrows point to the severely injured T9–10 segment. Vertical distraction injury is present resulting in severe spinal instability

Fig. 8.2
STIR sequence (left) and T2-weighted (right) magnetic resonance imaging (MRI) pictures demonstrating severe damage to the T9–10 segment with complete compromise of the intervertebral disk (left arrow), the longitudinal ligaments, and the posterior ligamentous complex (PLC) (right arrow). Also note the spinal cord injury edema – this resulted in a complete neurological injury

Fig. 8.3
Vertical distraction injury at the occipitocervical junction. Coronal and left parasagittal computed tomography (CT) images demonstrate a vertical distraction injury. This represents a type 2B occipitocervical dissociation in which the connection between the atlantoaxial articulation is lost. The skull and atlas ring have migrated in a vertical fashion away from the axis bone. The arrows point to severe atlantoaxial facet joint diastasis. This represents a highly unstable craniocervical relationship
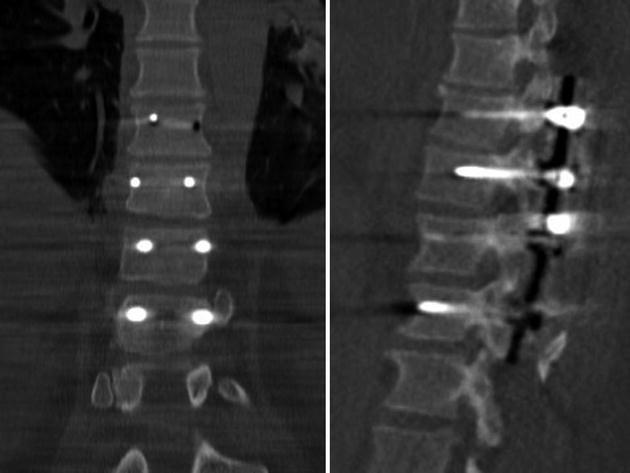
Fig. 8.4
Postoperative computed tomography (CT) images demonstrate T8–11 open reduction and internal fixation with instrumented posterior spinal fusion of the T9–10 fracture-dislocation
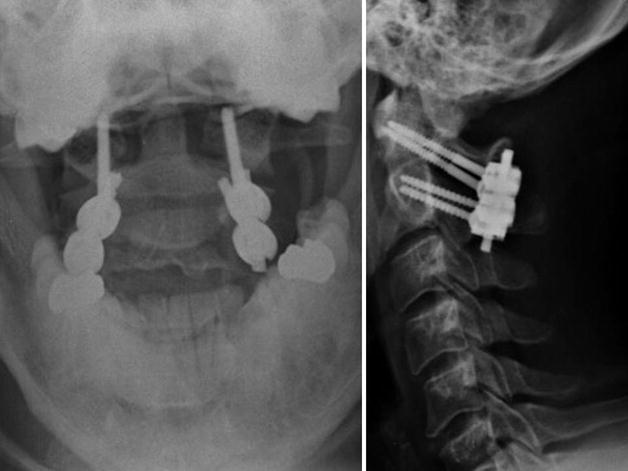
Fig. 8.5
Anteroposterior and lateral radiographs of the atlantoaxial open reduction and internal fixation with instrumented posterior C1–2 Harms-type spinal fusion. From both a cervical and thoracic standpoint, the patient garnered immediate stability which enabled instant mobilization without bracing. This facilitated easier therapy and nursing care in the surgical intensive care unit
Epidemiology
Spinal injury is common in polytrauma patients. Associated spinal cord injury (SCI) is arguably the most devastating survivable injury a patient can endure. SCI was formerly considered a death sentence, but modern medical care has enabled much improved quality of life and life span [1]. However, life expectancy is still foreshortened compared to the general population [2–4]. Incidence of SCI is approximately 429 cases per million person-years in the United States of America [5]. On a worldwide scale, the number is more difficult to calculate, but the incidence lies between 10 and 80 cases per million population [6]. Prevalence is increasing given the longer life expectancy of SCI survivors. As with most traumatic injuries in the United States of America, young white males are most affected. These patients are also more commonly single, uneducated laborers. Mechanism of injury includes motor vehicle accidents, falls from significant height, and gunshot wounds as the most common forms. Injuries usually occur in summer months and on weekends and are associated with other bodily injury at least half of the time. Injuries that accompany SCI most often include facial fractures, head injury, trunk injury, and long bone fractures [7]. Neurological injury level is most often cervical, followed by thoracic, and then lumbar. Patients affected by SCI suffer from pneumonia, thromboembolic events, and pressure sores and typically succumb to afflictions of the respiratory tract. Cost of SCI is a huge burden to patients, families, communities, and the total health-care system. Polytrauma patients that suffer severe spinal injuries with associated neurological compromise should be treated at institutions well versed in trauma and acute SCI care. Many tertiary care centers go to great lengths to develop comprehensive SCI protocols. These guidelines often include every detail regarding the care of these complex patients. Examples include directions about maintaining goals for mean arterial pressure [8] and specifics about skin care and bowel programs. Every detail of care is contained in these protocols in order to guide the caretakers. These protocols involve the interactions of innumerable health-care providers and are coordinated from the time these complex patients enter the trauma bay and continue throughout their hospital stays. These interdisciplinary efforts progress until patients are fully stabilized and ready for transport to the secondary rehabilitation center. These secondary centers are often specialized institutions that deal directly with the prolonged recovery and rehabilitation associated with spinal injury and neurological deficits that polytrauma patients can sustain.
Field Care
Emergency medical personnel must assume spinal injury is present when stabilizing and transporting polytrauma patients. Injured individuals are secured to spinal boards and further immobilized in cervical collars often with the addition of sandbags and sturdy tape. Log-rolling is essential when movement of injured patients is necessary. Field personnel prioritize treatment in the sequence of life, limb, and function. Injured athletes and motorcycle riders should have helmets and shoulder pads left intact until safe removal in the emergency department of the treating hospital. In-line immobilization of the head-neck unit (while aligned with the trunk) should occur while attempting to limit flexion and extension. Understanding that the head circumference of a child in proportion to the body size is larger than an adult is important during immobilization and transport. The torso of a child should be elevated with padding or a special child spine board should be utilized with a cutout for the occiput to protect against undue cervical flexion. Emergency personnel can also be extremely useful in communicating presence of neurological deficits to the treating specialists upon arrival at the trauma center. Furthermore, the emergency transport team can relay important details regarding the accident scene to the treating doctors during the hand-off in the trauma bay. This can provide useful information to care providers regarding injury mechanism and pattern-of-injury which may be significantly important during evaluation of complex polytrauma patients. Upon arrival to the emergency department, rapid assessment and evaluation needs to begin immediately in order to allow early removal of the spinal board and enable proper examination of the entire spinal column. It should also be noted that the “one-size-fits-most” cervical immobilizers applied in the field by emergency personnel are often not adequate for proper immobilization of the cervical spine in these highly injured patients. It should be a goal of the treating caretakers to rapidly assess if a cervical injury exists. If cervical injury is absent and the treating team can determine that the spine is “cleared,” then these field collars should be removed as soon as possible. If the treating team determines that a cervical injury is present, then a more properly fitted rigid cervical immobilizer should be applied and the spine surgeon should be contacted immediately for further evaluation.
Initial Assessment
Initial assessment of the polytrauma patient must start with acquiring and assimilating all available data related to the patient’s injury mechanism and circumstances. Special attention should be paid to the pattern-of-injury. A classic “injury pattern” is the presence of visceral injuries that may accompany a flexion-distraction “Chance” fracture in the setting of a motor vehicle crash where a patient has employed only a lap belt (Figs. 8.6, 8.7, and 8.8). Severe injuries can also occur to the large vessels when flexion-distraction moments are applied to the thoracolumbar spine [9]. Another example of a spinal “injury pattern” that must not be overlooked includes the presence of head and facial lacerations, abrasions, and fractures that may be coupled with an extension-compression cervical fracture mechanism. Extension-compression cervical injuries can also be associated with central cord syndrome especially when involving a spondylitic, stenotic spinal column (Figs. 8.9 and 8.10) [10]. This incomplete spinal cord injury syndrome typically manifests with greater deficits in the upper extremities compared to the lower extremities. Falls from significant height may show concomitant pelvis, acetabular, and lower extremity fractures coupled with lumbar and thoracolumbar axial-loading injuries [11]. Severe chest injuries may be linked to thoracic fractures and fracture-dislocations [12, 13]. All of these examples point to the importance of considering and understanding the pattern-of-injury that accompanies certain traumatic accident mechanisms. These patterns can often be deduced from an analysis of the patient’s complete list of injuries as well as discussing with emergency personnel the particular details of the injury scene along with eyewitness accounts. Prior to a thorough analysis of the injury pattern, treating teams should always adhere to ATLS protocol. Spinal evaluation can start concurrently with the primary survey and resuscitative measures through gross inspection. Secondary survey quickly follows with identification of neurological deficits, exposure and visualization of the entire spinal column, recognition of severely unstable injuries, as well as determining the presence of spinal and/or neurogenic shock. A detailed neurological examination is essential as the next step in evaluation. The ASIA classification can serve as a guide to proper neurological assessment (Fig. 8.11). Care providers need to understand the extreme importance of a proper and thorough rectal examination (Table 8.1). This examination can serve as a “window to the spinal cord” in obtunded patients. Spinal specialists should keep in mind the possibility of a “double-crush” phenomenon that may alter the rectal examination findings where two separate neurological insults exist in the same patient. This can lead to a drastically altered neurological exam that requires more diagnostic data usually in the form of MRI scan. Additionally, spinal specialists should be aware of conus medullaris level injuries that can lead to a mixture of upper and lower motor neuron signs. Injuries at this level can produce confusion in the early stages of spinal assessment. They can also terminally destroy the bulbocavernosus reflex arc. Following thorough examination, and once adequate physiological stability is provided, polytrauma patients can then receive appropriate radiological evaluation. Obtunded patients require total spinal imaging with CT scan. Injured spinal segments often require further analysis with MRI scan to evaluate the soft tissues and neural structures. With this information, spinal injuries can then be classified adequately, and appropriate treatment is then chosen by the spinal specialist.

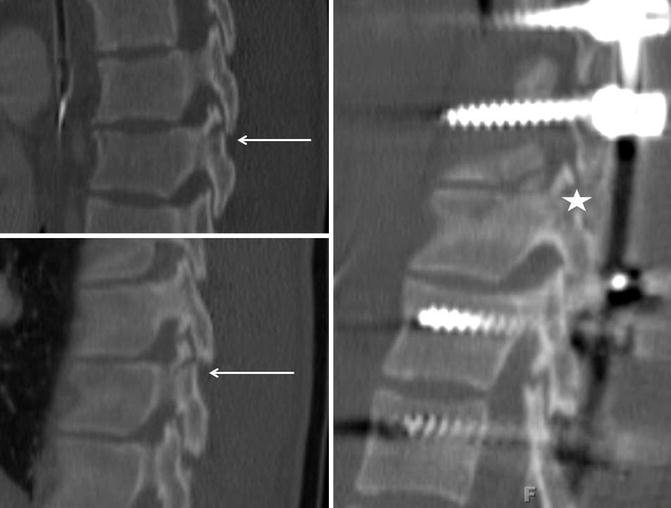
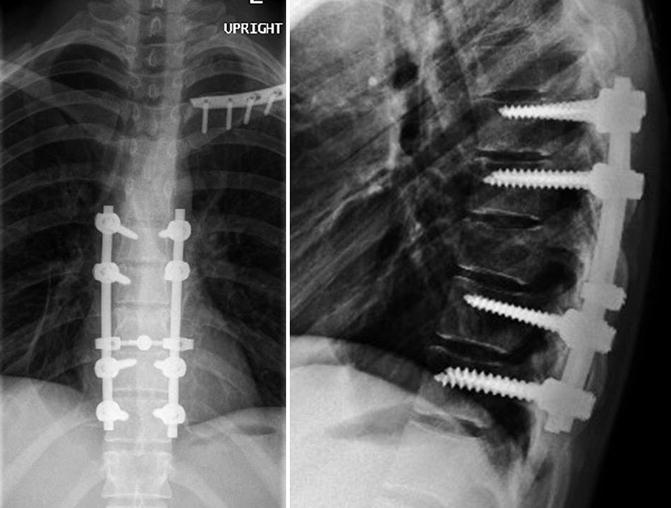
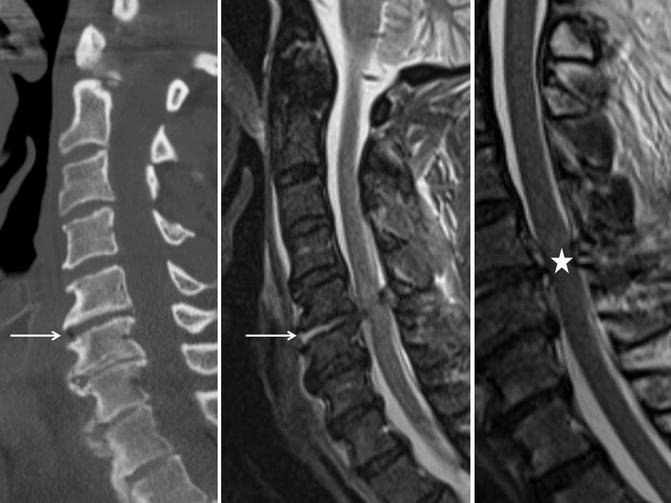
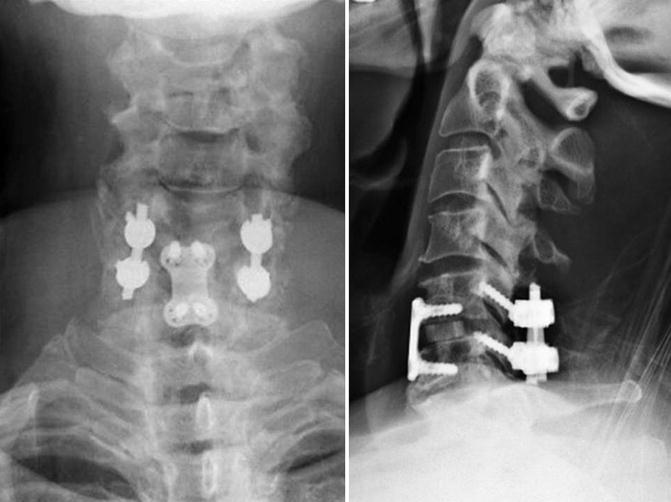
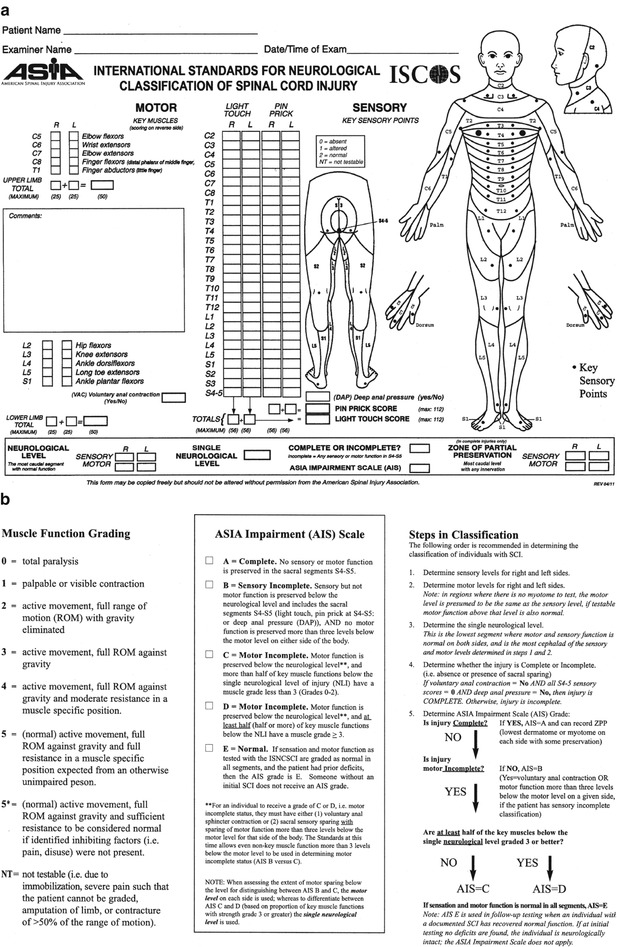

Fig. 8.6
Midsagittal computed tomography (CT) image and STIR MRI image depict a flexion-distraction injury to the thoracic spine. This poor young woman sustained severe abdominal injuries including splenic and liver rupture, pancreatic injury, and inferior vena cava laceration. These injuries often accompany lap belt-type spinal injuries (“Chance fractures”) that are the result of flexion-distraction mechanisms. This patient underwent emergent exploratory laparotomy with inferior vena cava repair, splenectomy, and liver packing. Once properly resuscitated and physiologically stabilized, the patient returned to the operating room 24 h later for an abdominal washout followed by closure. She was then rolled prone in the same setting and underwent operative spinal stabilization. The left arrow represents a small avulsion teardrop-type fracture that should alert the spinal surgeon to the possibility of a flexion-distraction fracture. The star is positioned about the posterior ligamentous complex rupture
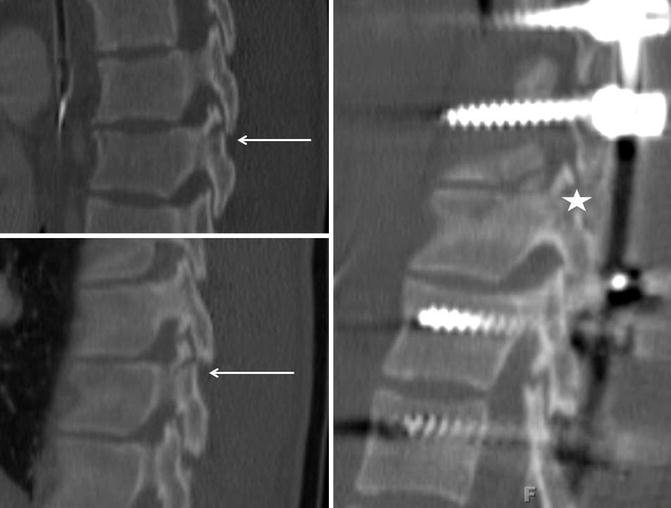
Fig. 8.7
Left and right parasagittal computed tomography (CT) images show bilateral pars/facet fracture-subluxations (arrow) which add to three-column spinal instability. The postoperative parasagittal image shows a nicely reduced and stabilized facet joint (star)
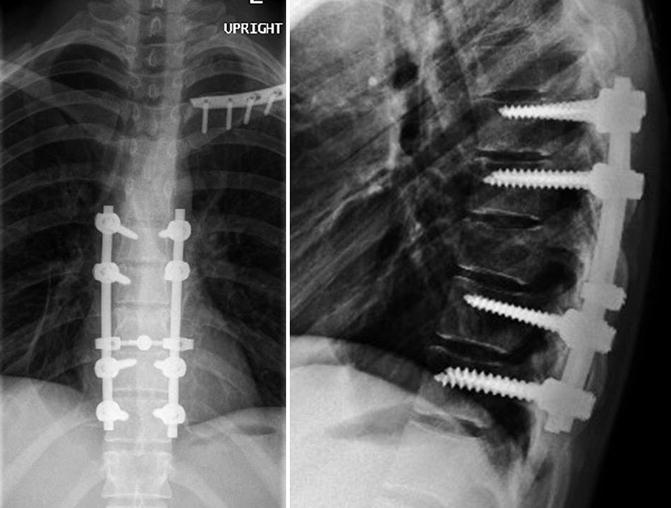
Fig. 8.8
Postoperative anteroposterior and lateral X-ray images of the thoracic spine showing T7–11 open reduction and internal fixation with instrumented posterior spinal fusion for the T9 “Chance fracture.” Notice the image is taken with the patient upright. The immediate spinal stability provided by the procedure enables early mobilization and proper nursing care. It also obviates the need for bracing, which could be quite detrimental to a patient with multiple abdominal injuries. Also, notice that the clavicle has been repaired. This reduction and fixation event was completed by the orthopedic traumatologist 2 days after spinal fixation. This demonstrates the multidisciplinary approach to polytrauma care that these complex patients demand
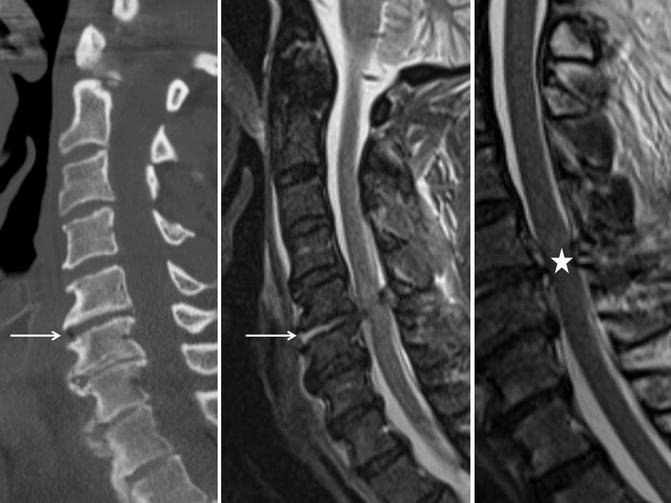
Fig. 8.9
Midsagittal computed tomography (CT) image (left image) of the cervical spine demonstrating maintained alignment and significant spondylosis. The only hint of an injury is the air diskogram at C5–6 (arrow). However, considering the “pattern-of-injury” in this patient, one develops much more concern. A fall from height with significant force impacting the facial region (multiple facial abrasions, lacerations, and a nasal bone fracture) coupled with a neurological exam showing mainly distal upper extremity deficits (consistent with central cord syndrome) led to an emergent MRI scan. Midsagittal STIR sequence and T2-weighted MRI cervical spine images (middle and right image) demonstrate C5–6 disk injury (arrow) along with stenosis, yellow-ligament buckling, and spinal cord injury edema (star)
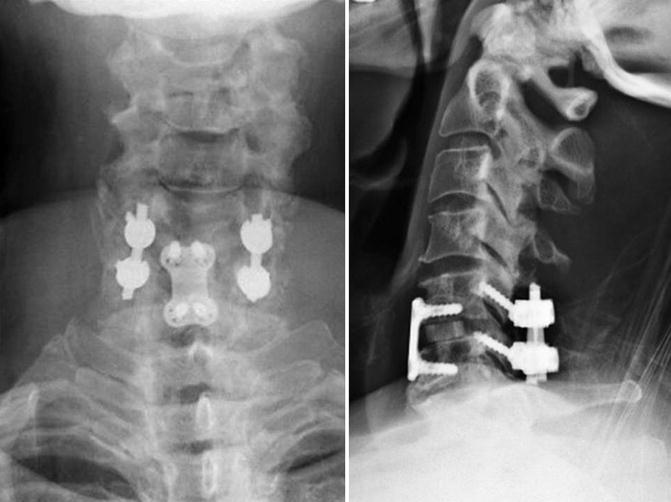
Fig. 8.10
Postoperative anteroposterior and lateral X-rays depicting C5–6 anterior cervical discectomy and instrumented fusion with insertion of machined, lordotic, allograft, interbody spacer coupled with instrumented posterior C5–6 fusion and decompression which includes C5 and C6 partial laminectomies and excision of the buckled ligamentum flavum with thorough decompression of the spinal cord. The X-rays are taken with the patient standing. This patient made a substantial postoperative neurological recovery
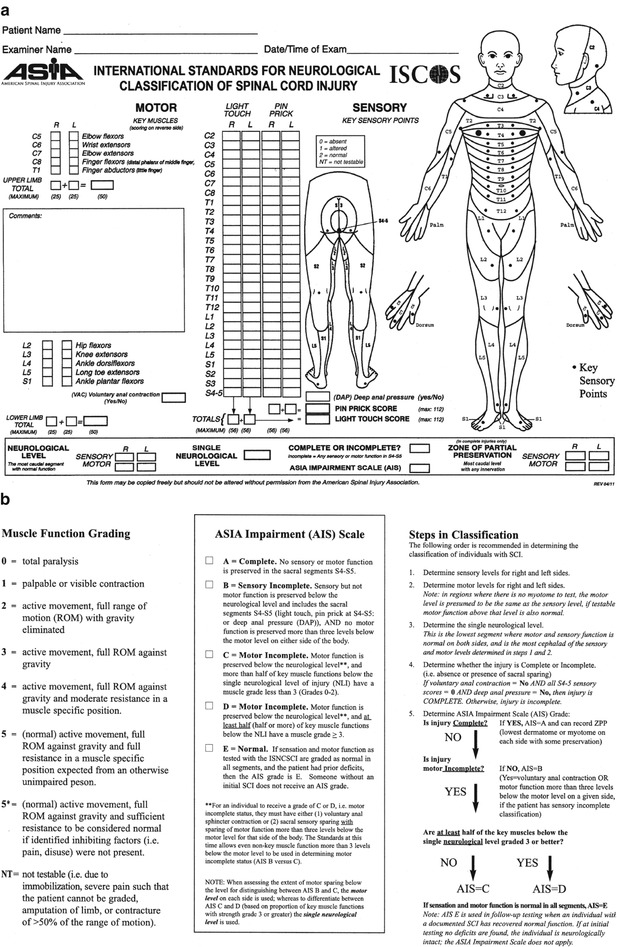
Fig. 8.11
American Spinal Injury Association (ASIA) standard neurological evaluation worksheet (a). ASIA Grading/Scale/Classification Tool (b). (Used with permission of the American Spinal Injury Association)
Table 8.1
A thorough and reliable rectal examination
1. Inspection |
Visualize the anus |
Presence of feces can signify incontinence |
2. Sensory evaluation |
Check perianal light touch |
Check perianal pin prick |
3. Reflex assessment |
Check anal wink reflex |
Check bulbocavernosus reflex (requires insertion of Foley catheter in women) |
4. Motor assessment* |
Check resting tone |
Check voluntary tone if possible |
Initial Management
Polytrauma patients with concomitant spinal injuries should be kept on log-roll precautions until definitive management strategies can be employed. Log-roll precautions include rigid cervical collar immobilization. The entire care team should understand the concepts and goals of log-roll precautions including frequent turning to avoid decubitus ulcer formation. Alternatively, a rotating frame bed may be utilized. The spine specialist should act quickly to determine an effective treatment plan that will enable mobilization of the patient and easier nursing care. More recent protocols recommend spinal stabilization within 24 h of injury to facilitate early mobilization and intensive care delivery [14]. This early interventional approach is a key component in reducing the incidence of complications in these multiply injured patients including reduced pulmonary, thrombotic, and integumentary adverse events. When early surgery cannot be employed due to a patient’s compromised physiological status, then alternative methods can be used. These methods include application of Gardner-Wells tongs traction, halo-ring traction, or halo-fixator application to reduce subluxations/dislocations in a closed manner. Halo-vest fixator application can also temporarily reduce and stabilize unstable occipitocervical and cervical injuries until internal fixation strategies can be employed. It can also be effective to utilize fluoroscopic analysis of injuries in the intensive care unit setting to ensure that alignment has been restored with these closed methods. This can eliminate the need to transport patients to the radiology suite and can also improve image quality compared to portable X-rays.
When the treating spinal specialist cannot employ closed means of stabilization such as halo-vest fixator placement or Gardner-Wells tongs traction and manipulation, it is important to relay the appropriate spinal precaution data to the primary caretakers. For instance, if a patient’s physiological status precludes definitive stabilizing surgery, but an unstable thoracic or lumbar spinal fracture exists, the care team should have specific instructions regarding the care, mobilization, and treatment of that patient from the spine perspective. Considerations include “head-of-bed” instructions/restrictions, frequency of neurological assessments, location and type of temporary brace fitting, delivery of medications, involvement of physical and occupational therapy (if indicated), and an explicit description of the definitive treatment plan. Once the entire care team understands the spinal treatment plan, patients can receive quicker and more appropriate interventions while awaiting the definitive spinal treatment solution.
Early care of polytrauma patients with spinal injuries also includes recognizing spinal shock and neurogenic shock and understanding the difference. Spinal shock is a transient syndrome of sensorimotor dysfunction. It is characterized by flaccid areflexic paralysis and anesthesia below the level of a spinal cord injury. The syndrome typically lasts between 24 and 72 h and has ended when reflexic activity resumes below the injury. The classical notion is that return of the bulbocavernosus reflex heralds the end of spinal shock. However, this topic is currently under debate by many physicians that routinely treat spinal cord injury [15]. The important message is that during the spinal shock phase which follows an SCI, the treating team cannot appropriately predict spinal injury level, spinal injury severity, or spinal recovery prognosis. Additionally, one should consider injuries directly to the conus medullaris where the bulbocavernosus reflex arc may be terminally destroyed. In contradistinction to spinal shock is the concept of neurogenic shock. This syndrome results from impaired sympathetic outflow tracts as a result of SCI and is accompanied by hypotension and bradycardia. It is diagnosed only after ruling out hemodynamic shock in the polytrauma patient. It is typically associated with more cephalad levels of spinal injury. Fluid resuscitation should proceed carefully while monitoring the markers of resuscitation including base deficit and lactate levels. Treatment of neurogenic shock should focus on increasing peripheral vascular resistance. Additionally, treatment should focus on definitive management of the spinal column injury with restoration of normal anatomical alignment and stabilization along with decompression of impinged neural elements as soon as patients can medically tolerate such procedures.
Not only do patients with neurogenic shock require careful blood pressure monitoring and pharmaceutical interventions to adjust for this potentially labile problem, but so too do patients with SCI even in the absence of neurogenic shock. There is increasing data to suggest that maintaining mean arterial blood pressure above 85–90 may be beneficial to SCI patients with regard to diminishing secondary injury [16]. The primary spinal cord injury occurs as a result of the physically deformed or compressed neural tissue usually as a result of fracture fragments, misalignment, ongoing compression from disk material, or a combination of factors. These offenders should be dealt with as soon as patient’s resuscitative status allows. Secondary injury to the spinal cord comes from diminished blood flow to the neural structures which can theoretically be benefited by maintaining adequate systemic blood pressure. Secondary injury can also be induced by vascular changes, endothelial damage, vascular clotting, hemorrhage, inflammation, production of free radicals, programmed cell death, electrolyte dysfunction, and release of neuroexcitatory transmitters that prove to be cytotoxic. To date, there is no single pharmaceutical medication that can heal the spinal cord. However, there are many potential interventions that can attack the problem at the level of the secondary injury. The future hopefully holds a strategy to successfully treat these spinal cord injuries. Restoring neural tissue and function is certainly one of medicine’s holy grails. One strategy that has been employed for many years for injured neural tissue is the administration of corticosteroids. Although it is still a topic of much debate, the delivery of high-dose steroid protocols has largely been abandoned at institutions that routinely treat spinal cord injured patients. The potential recovery of neural function is outweighed by the adverse effects on infection and pulmonary complications [17].
Many challenges exist with delivery of medications to labile polytrauma patients. This is certainly the case when concomitant spinal column and spinal cord injuries are present. However, even when those problems do not exist, patients can experience issues with the most simple treatment modalities. Polytrauma patients invariably arrive at the treating center in a rigid cervical field collar. It is important that protocols exist on the institutional level to rapidly assess the need for such devices as well as determine their adequacy. Providers must also appreciate that maintenance of a cervical immobilizer is not a benign measure. Respiratory compromise and skin ulcerations are just two of the problems that can accompany these items. This presents the concept of “cervical spinal clearance” (Fig. 8.12). Clearance protocols for the cervical spine are now essentially ubiquitous. Nonetheless, the treating team, and most importantly, the treating spinal specialist, needs to understand these concepts and be able to fully employ their directives. Spinal clearance can also be extrapolated from the neck to include the thoracic and lumbar spinal regions. “Clearance” implies that a thorough investigation of the spine has occurred and that no injury has been identified requiring treatment. Once that has been determined, all immobilization may be removed and log-roll precautions repealed. “Spinal clearance” is a challenging endeavor and may also be a time and labor-intensive process. It involves thorough history taking, complete physical examination, and thorough analysis of the radiological data. It may prove useful to divide the patients into four separate groups: asymptomatic, temporarily nonassessable, symptomatic, and obtunded. Once this is accomplished, the provider can easily run through the appropriate algorithm to determine the best course of treatment. Symptomatic patients require further radiographic assessment to determine diagnosis and treatment approaches. Asymptomatic, examinable patients without distracting injuries or intoxicated status can be clinically assessed and potentially cleared. Temporarily nonassessable patients require temporary rigid cervical immobilization until clearance of intoxicating substances, return of normal mentation, and/or stabilization of distracting injuries before they can be reliably assessed and potentially cleared. Obtunded patients require imaging to rule out spinal injuries. Polytrauma patients typically fit into the obtunded or temporarily nonassessable categories. Prolonged obtundation can present the treating spinal specialist with a dilemma regarding spinal clearance. Obviously, if an injury is identified, then a definitive treatment plan is determined and executed. If no injury is identified on CT scan, then the spinal specialist must decide whether to remove the rigid cervical collar. Some physicians believe that an MRI scan is mandatory in this situation. Others feel that monitored flexion and extension radiographs (or fluoroscopic analysis) are warranted. However, the incidence of occult unstable spinal injuries occurring in the presence of a normal CT scan is extremely low. Therefore, many institutions remove the cervical collar in obtunded patients that have no identified spinal injury on CT scan [18].