Spinal Fusion for Neuromuscular Scoliosis
Kirk W. Dabney
Freeman Miller
DEFINITION
Neuromuscular diseases are heterogeneous between and within diseases and are due to a vast number of pathologies involving the brain, spinal cord, peripheral nervous system, and muscle.
Neuromuscular spinal deformity is a result of neuromuscular disease which occurs during childhood, including cerebral palsy, muscular dystrophy, spinal muscular atrophy, etc. It may be related to a pathologic abnormality in muscle tone, motor control, weakness, or a combination.
Although neuromuscular scoliosis (coronal deformity) is the most common neuromuscular spinal deformity, sagittal plane deformity (hyperlordosis and hyperkyphosis) may also occur.
ANATOMY
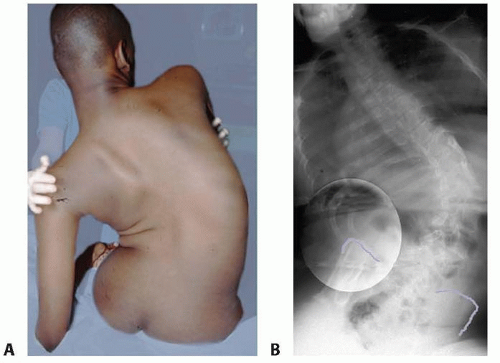
The curve patterns of neuromuscular scoliosis are most commonly lumbar and thoracolumbar with associated pelvic obliquity (FIG 1).
Because many children are nonambulatory, associated pelvic obliquity affects sitting balance.
Ambulatory neuromuscular patients often have decompensation, with the inability to center their head over the center sacral line.
PATHOGENESIS AND NATURAL HISTORY
The biologic basis of both scoliosis and sagittal plane spinal deformity in neuromuscular disorders differs depending on the specific neuromuscular disease. In general, however, most neuromuscular spinal deformities are largely due to muscle imbalance (high tone or low tone) and abnormal postural reflexes.
The natural history of neuromuscular scoliosis is typically that of progression, beginning with the development of a flexible scoliosis, often in middle childhood, and the more rapid progression to a more rigid scoliosis during the adolescent growth spurt. Some neuromuscular conditions are associated with a more progressive scoliosis than others.
The pathogenesis and natural history of some of the more common neuromuscular disorders associated with spinal deformity and the spinal deformity itself within the disease follow.
Cerebral Palsy
Cerebral palsy is a heterogeneous disorder that is characterized by a static lesion (eg, injury, congenital defect) to the immature motor cortex of the brain.
The natural history of neuromuscular scoliosis in cerebral palsy is relentless progression. Progression is most common in spastic quadriplegic cerebral palsy. The rate of progression can be severe in adolescent years (2 to 4 degrees per month).
Progression also occurs after skeletal maturity. In curves greater than 40 degrees, it may occur at a rate of 2 to 4 degrees per year.25
Curves in the 60- to 90-degree range begin to effect sitting balance, arm control, and head control. Further progression may prevent the child from sitting in an upright position.
Conservative treatment with chair modifications and bracing is only a temporary treatment and does not stop curve progression. Conservative treatment is especially helpful in the younger child with a flexible scoliosis to temporarily maintain upright sitting posture. This will allow the spine to grow to its maximum size (to achieve maximum sitting height) so that the resulting fusion can correct the spinal deformity without limiting growth.
Muscular Dystrophy
Duchenne muscular dystrophy is a sex-linked recessive disorder involving a defect on the Xp21.2 locus of the X chromosome resulting in a marked decrease or absence of the protein dystrophin.11
Affected children become progressively weaker with age, eventually becoming nonambulatory.
Death typically occurs in the second or third decade secondary to pulmonary or cardiac failure.
Scoliosis is almost universal when the child becomes nonambulatory, and curve progression correlates strongly with a decline in respiratory function.
In the past, the prevalence of scoliosis approached 100%.22 For this reason, surgery was previously recommended soon after the child became nonambulatory before an irreversible
decline in forced vital capacity occurred. Now with the advent of corticosteroids, the life expectancy of children with Duchenne muscular dystrophy is extended with a reported delay or prevention of the severity of scoliosis with long-standing use of corticosteroids.1, 13, 15 The risk of progression decreases if the scoliosis develops after 14 years of age.31 Pulmonary function decreases as the natural history of the disease and scoliosis magnitude progresses. Scoliosis surgery should be done before the forced vital capacity decreases to less than 30%.
Myelomeningocele
Myelomeningocele, a congenital malformation of the nervous system, is due to a neural tube defect and results in a spectrum of sensory and motor deficits.
Although the level of the spinal cord defect influences the clinical presentation of the condition, neurologic deterioration may occur at any age owing to hydrocephaly, hydrosyringomyelia, Arnold-Chiari deformity, and tethered cord syndrome.
In general, the higher the level of the defect, the higher the prevalence of scoliosis. Almost 100% of thoracic level paraplegic patients develop scoliosis.26
A long C-shaped curve is associated with a high level of paralysis and usually occurs at a young age.
Hydromyelia and tethered cord syndrome may also be associated with scoliosis and should be suspected if the scoliosis onset is more sudden and associated with other symptoms of acute neurologic deterioration.
Bracing in younger children can be attempted to slow progression, but it does not stop eventual progression.
Spinal Muscular Atrophy
Spinal muscular atrophy is an autosomal recessive disorder resulting in spinal cord anterior horn cell degeneration. Two genes on the chromosome 5q locus have been found to be associated with this disorder: survival motor neuron (SMN) gene and neuronal apoptosis inhibitory (NAIP) gene.24
Clinically, progressive muscular weakness occurs and eventual pulmonary compromise is common.
Three forms of the disease exist:
Type 1: early, acute Werdnig-Hoffman
Type 2: intermediate, chronic Werdnig-Hoffman
Type 3: late, Kugelberg-Welander type
Most children with the early form of the disease die at an early age and therefore do not require treatment.
Most children with the intermediate and late type who survive into adolescence develop a progressive spinal deformity. The curvature typically develops in the first decade. Thoracolumbar and thoracic patterns are most common.
One-third of patients have an associated kyphosis in the sagittal plane. Bracing is ineffective at preventing curve progression but may delay progression in the very young patient to allow further growth of the spine.2
Freidreich Ataxia
This autosomal recessive disorder results in a slowly progressive spinocerebellar degeneration. A defect on chromosome 9 has been identified.
The incidence of scoliosis is 100%, and progression is related to the age of disease onset. When disease onset is prior to age 10 years and scoliosis onset is before 15 years, scoliosis progression is usually greater than 60 degrees.
Progressive scoliosis requiring surgery occurs in about 50% of patients.14
Curve patterns are similar to idiopathic scoliosis: double major, single thoracic, and thoracolumbar.
Orthotic treatment may slow but usually does not prevent progression.
Rett Syndrome
This is an X-linked disorder that affects females almost exclusively. Some children have a mutation on the MECP2 gene.21 The child’s development is normal until 6 to 18 months of age, followed by rapid deterioration in cognitive and motor function.
After the initial deterioration in function, the neurologic picture may become relatively static for years. The clinical spectrum is variable, with some children remaining ambulatory and others becoming wheelchair bound.
Rett syndrome may be mistaken for cerebral palsy.
Scoliosis has been reported in up to 80% of patients.12
A long C-shaped thoracolumbar pattern is common. Bracing is usually ineffective, and curve progression is common. Surgical stabilization allows maintenance of sitting balance.
Spinal Cord Injury
Spinal cord injury in the skeletally immature child is associated with a nearly 100% incidence of scoliosis.7
The predominant curve type is a long C-shaped curvature. The younger the child, the higher the progression.
Prophylactic bracing may be effective in smaller curves (under 20 degrees). There are no data to support that bracing is effective in preventing progress in established curves greater than 20 degrees.
PATIENT HISTORY AND PHYSICAL FINDINGS
An accurate medical history is crucial for patients with neuromuscular disease.
In patients with cerebral palsy, the medical comorbidities strongly correlate with postoperative complications.17 This appears to also be true in patients with Duchenne muscular dystrophy, spinal muscular atrophy, and other neuromuscular disease.
Important historical information includes respiratory status, cardiac status, gastrointestinal status (eg, gastroesophageal reflux, nutritional intake), bone health (low bone density and history of fracture), and the presence of seizure disorder.
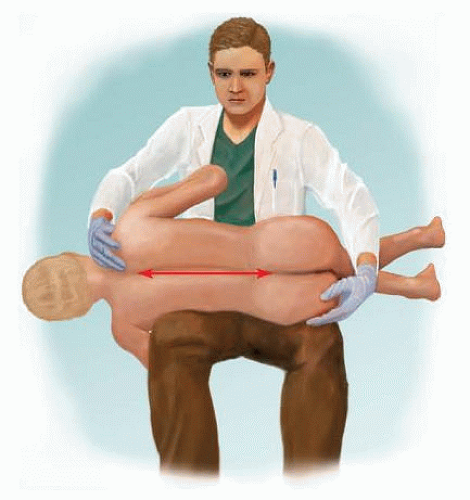
Physical examination should assess sitting or standing balance, the pelvic obliquity, curve magnitude, and stiffness (including the curve’s coronal, sagittal, and rotational components).
Coronal stiffness is best assessed by performing the side-bending test (FIG 2).
The physician should also assess for the possible coexistence of hip subluxation or dislocation, common in many neuromuscular diseases.
A complete neurologic examination should also be performed.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Anteroposterior (AP) and lateral radiographic views should be obtained to assess the Cobb angle and pelvic obliquity in the coronal plane and lumbar lordosis and thoracic kyphosis in the sagittal plane.
If intraspinal pathology is suspected, especially in the ambulatory patient, a preoperative magnetic resonance imaging (MRI) scan should be obtained.
If severe low bone density is suspected (history of multiple fractures), dual energy x-ray absorptiometry (DEXA) scan is recommended to assess bone density and potential need to treat.
DIFFERENTIAL DIAGNOSIS
Some neurologic diseases can look similar.
It is important to diagnose progressive neurodegenerative in which mortality from the disease is more rapid than the progression of the spinal deformity.
NONOPERATIVE MANAGEMENT
Although there was initially some historical enthusiasm for the treatment of neuromuscular scoliosis with casting or bracing, orthotic management is rarely able to halt progression of neuromuscular scoliosis.
Flexible curves in younger children may require seating modifications (hip guides and offset lateral seatback supports) or a sort thoracolumbar orthosis to maintain balanced seating until the child is at optimal sitting height.
SURGICAL MANAGEMENT
Indications
The indications for spinal fusion in neuromuscular scoliosis depend largely on the natural history of the specific neuromuscular disease and the natural history of the scoliosis within the specific disorder.
Examples of two neuromuscular diseases with different indications are Duchenne muscular dystrophy and cerebral palsy.
Duchenne Muscular Dystrophy
The major comorbidity in Duchenne muscular dystrophy is restrictive lung disease, with forced vital capacity dropping dramatically with scoliosis progression.
Due to the natural history, the indication for fusion is a scoliosis curvature greater than 25 degrees and forced vital capacity above 35%.
Cerebral Palsy
The indications for spinal fusion in children with cerebral palsy are a scoliosis curve magnitude approaching 60 degrees in the older child, especially if the curve is becoming stiff by physical examination.
Surgical correction is indicated when the child is not tolerating seating with a combination of either seating adjustments or a soft orthosis. This is usually done before the curvature reaches 70 degrees when the risk of complications increases.17
Less commonly, sagittal plane spinal deformity, hyperlordosis, and kyphosis will cause seating problems or back pain. Cerebral palsy patients with sagittal plane spinal deformity of 70 degrees or more causing seating difficulties or back pain can benefit from surgical correction.16
Typically during the middle part of adolescent growth, the scoliosis becomes much larger and begins to stiffen. Surgical instrumentation and fusion are recommended at this time.
Preoperative Planning
Technical Considerations
Three main technical preoperative considerations require careful consideration:
Is fusion to the pelvis necessary?
Is there a significant rotational component to the scoliosis that is contributing to difficulty in seating?
Is anterior release (discectomies around the stiff portion of the curve) necessary?
The only treatment that has made a definitive impact on neuromuscular spinal deformity is instrumentation and fusion.
The standard surgical procedure for neuromuscular scoliosis is a posterior spinal fusion with segmental instrumentation from T1 to T2 down to the pelvis if there is a significant pelvic obliquity.
Even if the pelvis is not involved in a severely involved nonambulatory patient or an ambulatory patient with a poor “righting reflex,” the surgeon should consider fusion to the pelvis to prevent the development of late pelvic obliquity. However, with modern pedicle screw instrumentation, complete correction of the lumbar spine to L5 may prevent subsequent development of pelvic obliquity or so that in the era sublaminar wire fixation.
The unit rod incorporates these concepts into one instrumentation system (FIG 3) as well as the concept of cantilever correction.3, 9, 18, 20
Newer methods of instrumentation allow modularization of the unit rod concept and cantilever correction by combining pelvic screws, precontoured rods, and a proximal connector (FIG 4).
Both the unit rod and the precontoured rods (in the modular unit rod construct) have prebent sagittal contour.
The unit rod comes in lengths from 250 to 450 mm.
Both 3/16- and 1/4-inch diameter rods are available. The 1/4-inch rod is used whenever possible, reserving the 3/16-inch rod for patients with a very thin gracile pelvis.
With the modular system, precontoured rods are connected with a proximal connector, in addition to pelvic screw with diameter (7 to 10 mm) and length (65 to 100 mm) that can be selected according to pelvic size.
Some surgeons are using pedicle screws instead of wires for segmental fixation, especially if there is a severe rotational
component to the curvature or pelvis. Caution should be taken when the bone is severely osteopenic, as the pedicle screws may pull out of the bone. Screws can be supplemented by wires or sublaminar cables as necessary.
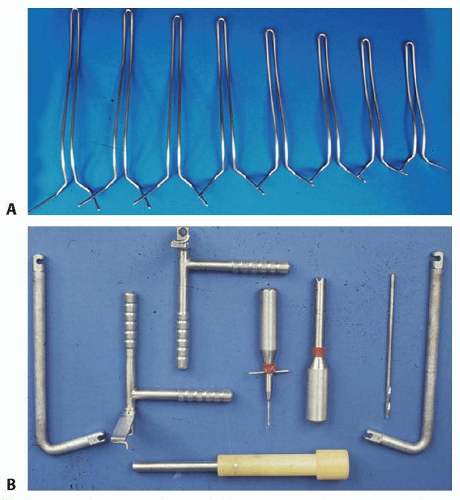
FIG 3 • A. The unit rod is available commercially in a range of sizes. B. Drill guides are provided for placement of the pelvic limbs as well as the impactor and pusher for the rod.
The unit rod (FIG 5A-C) and the modular unit rod (see FIG 4) are especially powerful as cantilevers to correct pelvic obliquity.
Anterior release for scoliosis is required for larger stiff curves that do not bend out on the bending test (generally >90 degrees) (FIG 5D).
Anterior release is also recommended for severe hyperlordotic and hyperkyphotic spinal deformities.16
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree