8 Spinal Disorders
Whiplash Injury: Treatment and Rehabilitation
Adriaan Louw, PT, MAppSc (Physio), CSMT
The Whiplash Epidemic
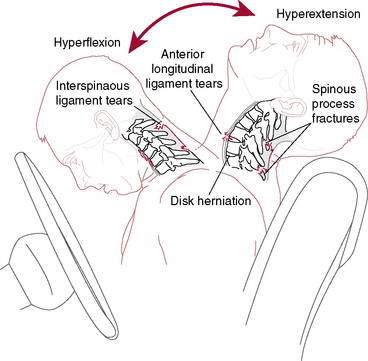
In 1928 Harold Crowe introduced the term “whiplash” to describe an injury mechanism of sudden hyperextension followed by hyperflexion of the neck. Although several other terms (e.g., necklash, hyperextension injury, and acceleration injury) have been suggested, the term whiplash has stood the test of time. Unfortunately, the term “whiplash,” which was used originally to graphically describe the manner in which the head was suddenly moved, has become a commonly used diagnostic label (Bogduk 2003). The biggest criticism associated with the labeling is the lack of information regarding the diagnosis, injury, prognosis, or treatment. Whiplash can best be described as a sudden acceleration and deceleration of the head in space (Fig. 8-1) (Bogduk 2003 and Spitzer et al. 1995). This describes the process of the sudden movement and slowing down of the head in space that can occur during a motor vehicle collision (MVC), sport, or activity of daily living (ADL) (Spitzer et al. 1995). Patients presenting for the treatment of signs and symptoms associated with the whiplash injury are said to have a whiplash-associated disorder (WAD) (Spitzer et al. 1995).
Whiplash injuries have been called the “disease of the century” with ever-increasing numbers of people diagnosed with WAD and seeking treatment (Bogduk 2003). Motor vehicle collisions are the leading cause of death among Americans 1 to 34 years old, and according to the U.S. Department of Transportation, the total societal cost of crashes exceeds $200 billion annually. With the increasing number of patients with WAD; little information available regarding the epidemiology; and nothing written on diagnosis, prognosis, and various interpretations of the treatments, therapists often describe whiplash as one of the most challenging and frustrating conditions to treat (Holm et al. 2007 and Spitzer et al. 1995). Adding to the frustration, several studies have shown that WAD leads to high rates of chronic pain and disability (Holm et al. 2007 and Sterling et al. 2006). It is now accepted that approximately one in four or even as many as one in three patients may develop pain lasting more than 2 years after an MVC (Bogduk 2003 and Spitzer et al. 1995). It is also interesting to note that no management approach treating acute whiplash has substantially reduced the incidence of transition to chronicity of this disorder (Spitzer et al. 1995).
Diagnosis
Before any attempt is made to treat WAD, consideration must be given to diagnosing the patient. Several authors have described this as a pivotal part in the development of persistent pain in patients with whiplash (Bogduk 2003 and Spitzer et al. 1995). Numerous studies have shown the high incidence of missed injuries, including fractures on standard imaging studies such as x-ray, magnetic resonance imaging (MRI), and computerized tomography (CT) (Bogduk 2003 and Spitzer et al. 1995). Because of the poor ability of these studies to truly identify tissue pathology, current Emergency Department (ED) guidelines do not routinely prescribe the use of imaging techniques such as x-ray, MRI, or CT scan. This creates a problem: A patient has significant pain and dysfunction, yet imaging tests are unable to “find a cause” of the pain. This has, unfortunately, also caused patients with WAD to be viewed as malingerers, dishonest, or even neurotic (Spitzer et al. 1995 and Sterling et al. 2006). Several studies have shown that a valid way to determine disability following whiplash is the taking of a thorough history and evaluation of the patient’s disability (Carroll et al. 2009 and Spitzer 1995). In fact, the neck disability index (NDI), which was originally designed for mechanical neck pain, was validated for use in patients with WAD. A high NDI indicates significant disability as a result of WAD, regardless of the results of the imaging tests. Therapists should realize that a thorough history and questions regarding function and/or the use of the NDI are currently the preferred tests to evaluate the effect of the WAD on the patient.
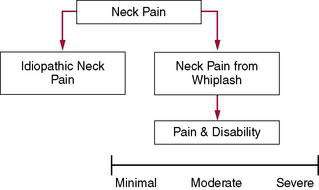
A second common fault in dealing with whiplash injuries is that patients with mechanical neck pain and traumatic neck pain (whiplash) often are grouped together (Jull et al. 2007). It is clear from the research that this is not only wrong, but also poses significant problems for patients and health care providers. The current research into whiplash injuries clearly shows that whiplash trauma is not biomechanically compatible with ADLs. Additionally, whiplash is not a homogeneous entity, with evidence from research indicating that WAD presents as a heterogeneous complaint in terms of the levels of pain and disability and changes in the sensory, motor, and psychological systems (Jull et al. 2007); however, such classification does little to direct physical therapy management. It is recommended therapists utilize two models: idiopathic neck pain and neck pain following trauma. Current research will most likely over time identify subclassifications of the WAD group (Fig. 8-2).
Treatment: Review of the Literature
In 1928 the term “whiplash” was introduced by Harold Crowe at a scientific meeting; for treatment of whiplash he suggested, “the less the treatment, the better it is.” In 1954 Gray and Abott advised bed rest during the first 24 to 72 hours and sedation as part of the medical approach and concluded that “constant use of a cervical collar resulted in atrophy and worsening of symptoms.” The first studies on exercise emerged in the 1960s, in which authors such as Barufaldi 1961) recommended traction and isometric exercises, followed by relaxation exercises. The first major study was published by Janes and Hooshmand (1965), who investigated 10,000 patients with whiplash between 1956 and 1963. They showed the following:
In the mid 1970s the controversies surrounding mobilization and manipulation started when authors began describing the benefits and precautions in applying mobilization and/or manipulation. When reviewing the literature on the use of cervical spine soft collars, it is interesting to note a variance between minimum periods of 2 weeks up to 1 year after MVC. Numerous early studies recommended the immediate start of therapeutic traction, with or without the application of heat. Clinical trials soon followed (1989). In 1986 Mealy et al. compared soft collars to Maitland mobilization techniques and showed greater improvement in the mobilized group in terms of range of motion (ROM) and pain ratings. In 1989 McKinney et al. compared rest, active physiotherapy, and self-care, showing no significant difference, and in 1990 Pennie and Agambar compared cervical traction, self-care, and neck and shoulder exercises, again showing no significant difference.
In 1995 a landmark study on whiplash was published—“The Quebec Task Force Study. (Spitzer et al. 1995).” The Task Force reviewed 10,382 articles published on whiplash over a 10-year period and found 62 studies relevant and meritorious. The Task Force summarized the results of the most commonly used treatments for whiplash (Table 8-1). This review, although dated, is still seen by many as the gold standard and is used as a template for treatment. The Task Force concluded that:
Table 8-1 Summary of the Quebec Task Force Findings on the Treatment of Whiplash-Associated Disorders (WAD)
| Treatment | Summary and Recommendation by the Task Force |
|---|---|
| Collars | Commonly prescribed; may delay recovery, causing increased pain, and decrease range of motion (ROM). Soft collars do not adequately immobilize the spine. |
| Rest | Commonly prescribed for the first few days. Should be limited to less than 4 days. Detrimental to recovery from WAD. |
| Cervical pillows | No studies |
| Manipulation | Single manipulation reduced asymmetry but showed the results lasted less than 48 hours. Comparing mobilization to manipulation, no clear benefit of one over the other in decreasing pain and increasing ROM. Long-term manipulation is not justified in the treatment of WAD. |
| Mobilization | Several studies. Maitland and McKenzie mobilization versus rest showed significantly greater improvement in pain and ROM for the mobilization groups. One study showed that patients given active exercises and advice recovered just as well as the mobilized group. Another study showed that mobilization was more effective than a combination of analgesics and education in the decrease of pain and increase of ROM. Mobilization appears to be beneficial in the short term, but the long-term benefits need to be established. Physical therapy should emphasize early return to usual activity and promote mobility. |
| Exercise | No independent effect of exercise has been evaluated. The evidence suggests exercise as part of a multimodal intervention may be beneficial (short- and long-term). |
| Traction | No independent effects of traction were found. One study tested different types of traction (static, intermittent, manual), but no significant differences were found on the different traction types. |
| Posture | No studies |
| Spray and stretch | No studies |
| Transcutaneous electrical stimulation (TENS) | No accepted studies |
| Electrical stimulation | No studies |
| Ultrasound | No studies |
| Laser, diathermy, heat, ice, massage | No independent studies. The modalities were part of the combination of passive modalities in different studies. |
| Surgery | No studies on surgery or nerve blocks |
| Injections Epidural Intrathecal Intra-articular | No studies. Not justified in the management of WAD patients. |
| Pharmacology Analgesics Anti-inflammatories | Shown to be effective with the use of physical modalities. |
| Muscle relaxants | No studies |
| Psychosocial | No studies |
| Acupuncture | No studies |
Treatment of Acute Whiplash (0–3 Weeks)
The first 3 weeks are chosen as the acute phase based on tissue healing time, clinical observation regarding referral to physical therapy, and important research related to timelines associated with whiplash (Sterling et al. 2003). This phase includes the immediate postwhiplash examination and treatment in the ED. After the ED visit patients typically are referred to their primary care physician for followup. Based on clinical observation, it is typical that injury, ED visit, physician followup, and subsequent referral to physical therapy occur around the third week. Based on the current best evidence into WAD treatment, some therapists may view this as inadequate and believe that therapy should start sooner. From a pain science perspective, it may be worthwhile to have a patient “rest” for a few days and psychologically “cope with the injury.” However, significant evidence suggests that early education and encouragement to move soon after the injury are of great value. This is different from aggressive early mobilization/manipulation. Several authors have questioned this approach because of the significant injuries associated with whiplash and the high incidence of missed fractures (Bogduk 2003). Two recent RCTs showed that patients who received educational videos in the ED regarding the pathology, self-help ideas, prognosis, plan of care, and goals performed much better than patients receiving “usual care”—ED waiting room, tests, medicine, and referral to their primary care physicians (Oliveira et al. 2006). Therefore, in the acute phase (0–3 weeks) therapists may consider the following:
Treatment of Subacute Whiplash (3 weeks–3 months)
Most patients seen in physical therapy after a whiplash injury are seen in the subacute phase. These patients follow the traditional model of injury: ED visit, referral to their primary care physician, and then referral to physical therapy approximately 3 weeks after the injury. These patients usually present with neck pain, scapular pain, headaches, decreased ROM, decreased function, and possible neurologic deficit (Bogduk 2003 and Spitzer et al. 1995). Treatment of the patient with subacute whiplash includes all of the acute whiplash principles and current best-evidence strategies.
Spinal stabilization exercises (Sterling et al. 2003). There is a large body of research regarding segmental spinal stabilization in the lumbar spine. Similar research is now emerging about the cervical spine (Jull et al. 2007 and Sterling et al. 2003). The cervical spine helps support and orient the head in relation to the thoracic spine and thus in essence provides two key elements: stability and mobility. Similar to the lumbar spine, the deeper muscles closer to the spine contribute to stability of the cervical spine, whereas the larger, superficial muscles that span multiple joints contribute more to movement. The deeper muscles have control strategies and proper morphology to stabilize the neck. In healthy individuals, the deep neck flexors provide a low-level, tonic contraction prior to movement of the extremities to protect the cervical spine. However, following injury, several changes occur to the deep cervical flexors:
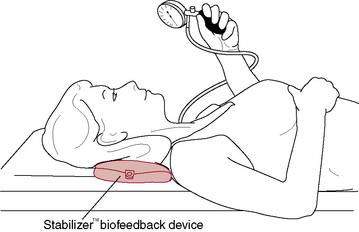
All of these changes indicate that patients with neck pain (i.e., WAD) will demonstrate limited endurance, greater fatigability, less strength, altered proprioception, and reorganization of motor control. The cranio-cervical flexion test (CCFT) is used to evaluate the ability of the deep cervical flexors to produce low-load tonic submaximal contractions (Fig. 8-3) (Jull et al. 2008). Therapists should concentrate part of the rehabilitation of the patient with whiplash to retraining the deep neck flexors of the cervical spine. These exercises should aim to provide protection to the cervical spine during ADLs. Once local stabilizers have been activated and retrained, therapists should have patients perform various forms of exercises incorporating weights and resistive bands while engaging the deep neck flexors. Stabilization exercises should aim to focus on low-load, tonic contractions, which should be progressed by increasing the time the patient contracts the deep neck flexors—endurance.
Manual Therapy (Spitzer et al. 1995). The Quebec Task Force study and subsequent systematic reviews and RCTs have shown that manual therapy techniques such as spinal mobilization and spinal manipulation may be of benefit to patients with subacute whiplash. Following a thorough examination, therapists are encouraged to carefully progress through the grades of movement/resistance to alleviate pain and dysfunction associated with specific physical dysfunction of specific joints/spinal levels. Manual therapy can be applied to both the cervical spine and thoracic spine. Evidence suggests that patients with neck pain respond favorably to manipulative therapy applied to the thoracic spine. Considering the concerns about missed fractures and significant tissue injury with whiplash, it is recommended that therapists perform skilled evaluations, continually reassess the patient, and adhere to a principle taught by manual therapy pioneer Geoffrey Maitland (2005) of “using the least amount of force to gain the desired outcome.” Qualitative studies have shown that patients want to receive hands-on treatment, and studies that compared hands-on to exercise-only interventions have found that hands-on treatment leads to better outcomes in the short term.
Consideration also should be given to strategies aimed at reducing the chance of a patient with subacute whiplash developing chronic WAD. Therapists who treat patients in the acute and subacute phases have a unique opportunity to help a patient progress through these phases and not move on to the chronic phase. Several factors have been identified in the development of chronicity, including factors associated with the accident (head position, signs and symptoms, the accident site, male/female, stationary car, etc.) and patient attributes (poor coping skills, extended rest, etc.) (Bogduk 2003, Jull et al. 2008, and Spitzer et al. 1995). Some factors can be positively affected by a therapist in the acute and subacute phases.
Treating Chronic Whiplash (3 Months and More)
Although patients with subacute whiplash may be the group most frequently presenting to physical therapy, patients with chronic whiplash are the most challenging. Three months is chosen specifically for the chronic phase because several studies have shown that patients who do not have significant decrease in their symptoms by 3 months postinjury have a very high likelihood of developing chronic pain associated with the whiplash injury (Spitzer et al. 1995, Sterling et al. 2003, and Sterling et al. 2006). This population also includes patients with whiplash who show up months or even years after injury seeking help for the pain and disability.
Education has been discussed in detail. Recent research has evaluated the use of neuroscience education in decreasing pain and disability among patients with chronic pain. It is recommended that therapists educate patients more regarding their pain as opposed to only using anatomy models. Additionally, neuroscience education has been shown to decrease fear and change a patient’s perception of his or her pain (Oliveira et al. 2006).
Therapeutic Exercise for the Cervical Spine
Christopher J. Durall, PT, DPT, MS, SCS, LAT, CSCS
Neck pain affects most adults at some point in their lives, and nearly 20% of the population suffers from persistent or recurrent symptoms (Croft et al. 2001, Binder 2006). Individuals with neck pain may have deficits in coordination (Falla et al. 2004a, Chui et al. 2005), strength, endurance (O’Leary et al. 2007c), repositioning acuity (Kristjansson et al. 2003, Sjolander et al. 2008), postural stability (Michaelson et al. 2003), or oculomotor control (Treleaven et al. 2005a). Patients with neck pain may also have mobility deficits in the cervical and/or upper thoracic regions (Childs et al. 2008). Therapeutic exercise has shown considerable promise as an intervention for individuals with neck pain (Kay et al. 2005, Gross et al. 2007), despite a lack of consensus among clinicians and researchers on optimal exercises or guidelines. In this section, exercises intended to correct deficits are discussed, with the objectives of reducing symptoms, improving function, and preventing recurrence.
Exercises to Improve Muscular Coordination, Endurance, or Strength
Deficits in cervical muscle performance may occur rapidly following the onset of neck pain and may persist despite symptom reduction or resolution (Sterling et al. 2003). Research has shown that exercises to improve coordination, endurance, or strength can aid neck symptom resolution (Sarig-Bahat 2003). This is logical given that the neck musculature provides nearly 80% of the mechanical stability of the cervical spine (Panjabi et al. 1998).
The deep cervical flexor (DCF) muscles (longus capitus and colli, rectus capitus anterior and lateralis, hyoid muscles) and deep cervical extensor (DCE) muscles (semispinalis cervicis, multifidus, rectus capitus posterior major and minor), in particular, appear prone to impairment in patients with neck pain (Sterling et al. 2003). These muscles have a high density of type I fibers and muscle spindles and are vulnerable to pain inhibition (Boyd-Clark et al. 2002). Reduced control and capacity of the deeper neck muscles can result in unwanted segmental motion or buckling during contraction of the multisegmental superficial muscles (Winters & Peles 1990). Thus the initial rehabilitation emphasis should be toward improving performance or coordination of the deeper cervical muscles.
Exercises to Improve Muscular Coordination
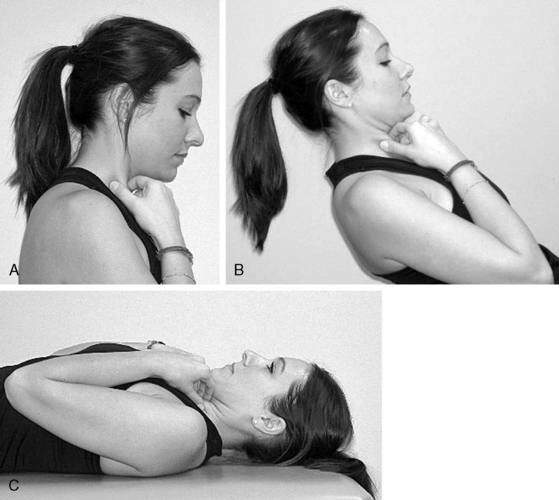
Patients with neck pain tend to have impaired DCF activity and elevated superficial cervical flexor (SCF; sternocleidomastoid [SCM], anterior scalene) activity during craniocervical flexion (Falla et al. 2004a, Chui et al. 2005). One exercise reported to help reverse this aberrant neck flexor synergy uses a pressure device positioned inferior to the occiput to provide feedback (Fig. 8-4). For this exercise the patient attempts to flatten the cervical lordosis, which requires DCF contraction (Mayoux-Benhamou et al. 1994), while minimizing SCF activation. The contractile effort with this exercise should be low and the patient should focus on precise control of the movement. Low-load exercises (∼20% maximal voluntary contraction) have been shown to facilitate more selective activation of the deeper cervical flexor and extensor muscles, while minimizing activity in their more superficial synergists (O’Leary et al. 2007b). Gentle, low-load exercise has also been shown to produce a superior, immediate hypoalgesic effect relative to higher-load exercise and is more appropriate when pain is a primary concern. Exercising above the pain threshold can impair neuromuscular control (Falla et al. 2007).
The pressure device–assisted craniocervical flexion exercise was reported to be as effective at increasing cervical flexion strength as an endurance exercise program in patients with chronic neck pain (Falla et al. 2006). Moreover, the perception that the exercise program was beneficial was roughly 10% greater in the group that performed craniocervical flexion with a pressure device. Of interest, this exercise was shown to improve repositioning acuity in people with neck pain to nearly the same extent as a proprioceptive training regimen (Jull et al. 2007b).
Controlled craniocervical flexion also can be done without a pressure device (Fig. 8-5). This exercise can be done sitting or standing initially to minimize gravity resistance and then reclined as tolerated to increase gravity resistance. Once the patient can nod while supine with minimal SCF activation, he or she can practice flexing the lower cervical spine while sustaining upper cervical flexion (Fig. 8-6). The SCMs are required to flex the lower cervical segments, so the patient does not need to palpate the SCMs during the combined movement. Inability to sustain upper cervical flexion during this exercise results in head protrusion (Fig. 8-7), which indicates that the exercise is too challenging and should be regressed. Krout and Anderson (1966) reported that 12 of 15 patients with nonspecific neck pain who performed controlled head/neck flexion while supine experienced good to complete recovery. This exercise, and the craniocervical flexion exercise described previously involving the pressure device, were shown to produce equivalent neck flexor strength gains following 6 weeks of twice-weekly training in a group of women with mild neck pain and disability (O’Leary et al. 2007b). Exercises for the DCFs can be particularly important for patients with cervicogenic headaches, who are prone to have poor DCF strength and endurance (Watson & Trott 1993, Jull et al. 1999) and weak cervical extensors (Placzek et al. 1999).
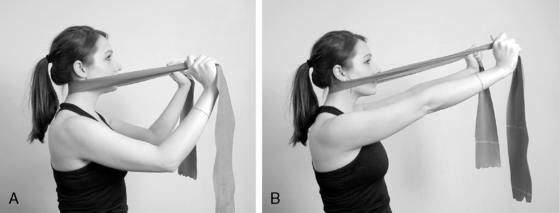
Compared to the DCF, evidence-based recommendations for facilitating selective activation of the DCE muscles are lacking. O’Leary and colleagues (2009) proposed that flexing and extending the lower cervical spine while maintaining a neutral craniocervical spine challenges the deep lower cervical extensors while minimizing activity of the more superficial extensors (Fig. 8-8). My preferred method for training the cervical extensors is shown in Figure 8-9. This exercise provides patient-controlled, progressive resistance to the cervical extensors. Whether this exercise selectively activates the DCE is unknown. Low-intensity isometric exercises for the cervical rotators also have been suggested to facilitate co-contraction of the neck flexors and extensors (Jull et al. 2007b).
Exercises to Improve Muscular Endurance or Strength
When an acceptable foundation of muscular coordination has been established, endurance and strength conditioning may be introduced. Previous studies have shown that endurance training and/or strength training can reduce pain and disability in patients with cervical strain, degenerative or herniated discs, and chronic or recurrent neck disorders. An endurance training approach utilizing low loads should be considered initially to avoid symptom aggravation. Of note, several investigators have found endurance training and strength training to be equally efficacious in reducing chronic neck pain, at least in women (Waling et al. 2000, Ylinen et al. 2006). Exercises to increase fatigue-resistance of cervical and upper thoracic muscles may be particularly useful for patients with neck pain associated with sustained postures. Patients with neck pain have been found to adopt a more forward-head posture and have difficulty maintaining an upright posture when seated (Szeto et al. 2002). Corrected posture in sitting significantly reduces cervical, upper thoracic, shoulder, and facial muscle activity compared to forward-head posture (McLean 2005).
Individuals with neck pain may also have impaired performance of the axioscapular muscles (levator scapulae, trapezius) (Falla et al. 2004). This phenomenon may be explained by the dual influence of the axioscapular muscles on the cervical spine and the shoulder girdle (Behrsin & Maquire 1986). Weakness of the trapezius muscles in particular has been reported to coincide with neck disorders (Andersen et al. 2008). Exercises known to elicit high levels of activation in the trapezius muscles are listed in Table 8-2 (Moseley et al. 1992, Ballantyne et al. 1993, Cools et al. 2007). Performing shoulder abduction while standing with the back against a wall (Fig. 8-10) may help correct deficits in trapezius performance and structural alignment simultaneously (Sahrmann 2002). Additional exercises for the axioscapular muscles have been used in various neck rehabilitation protocols (e.g., shoulder abduction, flexion, extension, scapular retraction, wall or floor push-ups, latissimus pull-downs, arm cycling), and associated pain reduction benefits have been reported (Randlov et al. 1998, Waling et al. 2000).
Table 8-2 Exercises with High Levels of Trapezius Electromyographic Activity
| Exercises with High Levels of Upper Trapezius EMG Activity |
| Exercises with High Levels of Middle Trapezius EMG Activity |
| Exercises with High Levels of Lower Trapezius EMG Activity |
EMG = electromyography; “T” = prone horizontal abduction, starting @ 90 degrees of abduction; ER = external rotation; empty-can = scaption w/ glenohumeral internal rotation; “Y” = prone horizontal abduction, starting ∼120 degrees of abduction.
It is worth noting that the cervical spine and head must be fixated during upper trapezius or levator scapulae activation for meaningful force transmission to the scapulae. During arm elevation, for instance, the head and cervical spine attachments of the upper trapezius must be fixed to enable the muscle to upwardly rotate the scapula. Inadequate fixation will result in craniocervical extension. Thus, in this example, the DCF muscles must be activated to stabilize the head and cervical spine by neutralizing the extension moment of the upper trapezius (Fig. 8-11) (Porterfield & DeRosa 1995). This reinforces the importance of creating a foundation of motor control/coordination in the deeper cervical muscles before higher-resistance training exercises are introduced.
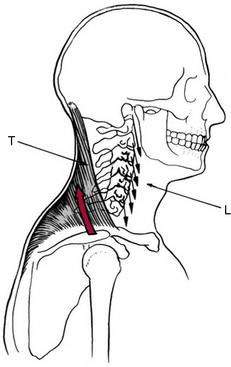
(From Porterfield JA, DeRosa C. Mechanical Neck Pain: Perspectives in Functional Anatomy. Philadelphia: WB Saunders Co. 1995. Fig. 3-6, p. 54)
Higher-resistance training of the cervical musculature may be necessary to significantly reduce pain and disability in individuals with chronic or recurrent neck disorders or to provide adequate muscular stabilization and force dissipation in select patients (e.g., wrestlers, football players). Ylinen and colleagues (2006) reported that the greatest strength gains and symptom reduction in women with chronic neck pain occurred during the first 2 months with strength training or endurance training. This suggests that a concerted effort may be required for at least 8 weeks to reap the benefits of endurance or strength training on neck pain. In another study, Ylinen et al. (2007a) reported that the gains in neck strength and motion achieved during a 12-month exercise program were largely maintained 3 years later. This suggests that patients should be encouraged to continue endurance and/or strength training, presumably with an independent “maintenance” program, for up to 1 year to prevent symptom recurrence.
Endurance and/or strength training can be particularly effective for women (Ylinen 2003, 2006, 2007). Women have a greater incidence of neck pain and higher prevalence of chronic neck pain than men (Hagen et al. 2000), which may be attributable to lower muscle strength (Vasavada et al. 2008). Maximal moments of the neck muscles are roughly 1.5 to 2.5 times lower in women than men, even when adjusted for body size (Jordan et al. 1999). Consequently the neck flexors and extensors are roughly 30% and 20% weaker, respectively, in healthy females than in males (Vasavada et al. 2008). This suggests that, in women, the mechanical demands on the neck muscles may be closer to their maximal moment-generating capacity. As a result, neck muscles may fatigue sooner in women, diminishing the muscles’ capacity to stabilize the cervical spine.
The intensity, volume (repetitions and sets), and frequency of endurance and strengthening exercises should be “titrated” to stimulate the desired adaptive changes without undesirable side effects such as symptom aggravation or poor adherence (Haskell 1994). Patients with high irritability may tolerate only brief bouts of very-low-intensity exercise through a limited arc, whereas patients with moderate or low irritability may be tolerant of longer and more intense exercise sessions.
Evidence suggests that the majority of strength gains occur in response to the first exercise set stimulus (Pollock et al. 1993, Durall et al. 2006). Accordingly, the American College of Sports Medicine (2002) recommends one set per exercise, with each set performed to volitional exhaustion. Pollock and colleagues (1993) reported that strength gains in the cervical extensors were not statistically different between healthy subjects who performed one set of 8 to 12 repetitions or two sets of 8 to 12 repetitions twice each week for 12 weeks. Randløv et al. (1998) found no difference in pain, ADLs, strength, or endurance outcomes between groups of patients who performed one set or five sets of cervical and shoulder exercises over 3 months.
Exercises to Improve Repositioning Acuity, Oculomotor Control, or Postural Stability
Research has shown that people with chronic or recurrent neck disorders or neck pain secondary to cervical spine trauma are prone to deficits in head/neck repositioning acuity (Kristjansson et al. 2003, Sjolander et al. 2008), postural stability (Michaelson et al. 2003, Treleaven et al. 2005b), and oculomotor control (Treleaven et al. 2005b)—apparently as a result of impaired afferentiation from cervical mechanoreceptors (Dejong et al. 1977). A growing body of evidence supports the use of exercises to ameliorate these deficits (Sarig-Bahat 2003).
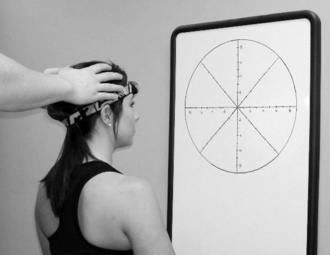
Repositioning acuity can be fostered by using a light source (e.g., focused-beam headlamp or laser pointer affixed to a headband) and a target (e.g., dart board, archery target) (Fig. 8-12). Relocation exercises, like the one demonstrated in Figure 8-12, are commonly performed sitting but also can be done standing. Labile surfaces (e.g., ball, dome, wobble board) can be used to increase the challenge.
< div class='tao-gold-member'>
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree