Spinal cord injury (SCI) results in multiorgan system dysfunction. Previously, SCI portended reduced survival and diminished quality of life. However, with increasing awareness and advances in the management of complications from SCI, individuals are living longer and more satisfying lives. This article summarizes major interventions and advances in the management of patients who have SCI. Fundamental principles of SCI are reviewed by organ system and key points are highlighted.
Spinal cord injury (SCI) results in multiorgan system dysfunction. In the past, SCI portended reduced survival and diminished quality of life. However, with increasing awareness and advances in the management of complications resulting from SCI, individuals are living longer and more satisfying lives. This article summarizes major interventions and advances in the management of patients who have SCI. Fundamental principles of SCI are reviewed by organ system and key points are highlighted.
Spinal cord injury epidemiology
The annual incidence of SCI in developed countries is estimated at 15 to 40 cases per million population . In the United States, approximately 12,000 new injuries occur per year, with 5000 of those injured dying before arrival at a hospital or during the hospitalization.
The prevalence of SCI is estimated to be 253,000 persons, ranging from 225,000 to 296,000 . Men sustain SCI approximately four times more often than women. Although this 4:1 gender ratio has remained constant over the past 3 decades, a slight trend has been seen toward more women having injuries, increasing from 18.2% in the 1970s to 21.8% in the 2000s . From 2000 to 2003, the average age of injury was 38 years . This increase is believed to be caused by the increasing age of the general population.
At 67.4%, Whites compromise the larger proportion of those injured, followed by African Americans making up 19.4%, Hispanic-Latino with 10.1%, and Other contributing 3.2% .
Motor vehicle crashes continue to be the most common cause of SCI (45.6%), followed by falls (19.6%), violence (17.8%), sports (10.7%), and other causes (6.3%) .
Since 2000, the most frequent neurologic category of injury is incomplete tetraplegia (34.1%), followed by complete paraplegia (23.0%), complete tetraplegia (18.3%), and incomplete paraplegia (18.5%) . In persons who have motor and sensory complete injuries, mortality rates are higher for those who have higher tetraplegia (C1-3) than for mid (C4-5) and low (C6-8) injuries. Those who have low tetraplegia have a higher mortality than individuals who have paraplegia.
Functional and clinical anatomy
The spinal cord serves as the relay tract that transfers motor information from the brain to the periphery, and receives sensory information distally and brings it centrally. It is protected and supported by meningeal coverings (the dura and pia mater), ligaments, and bony vertebrae (7 cervical, 12 thoracic, 5 lumbar, and 5 sacral). Blood supply to the spinal cord is provided by a single anterior spinal artery that supplies the anterior two thirds of cord, and two posterior spinal arteries that supply the posterior one third of the cord. Radicular arteries support the anterior and posterior spinal arteries. The artery of Adamkiewicz, a large lumbar radicular artery, supplies the midthoracic cord (T8-L1 vertebral level) and can be disrupted through injury to the thoracoabdominal aorta .
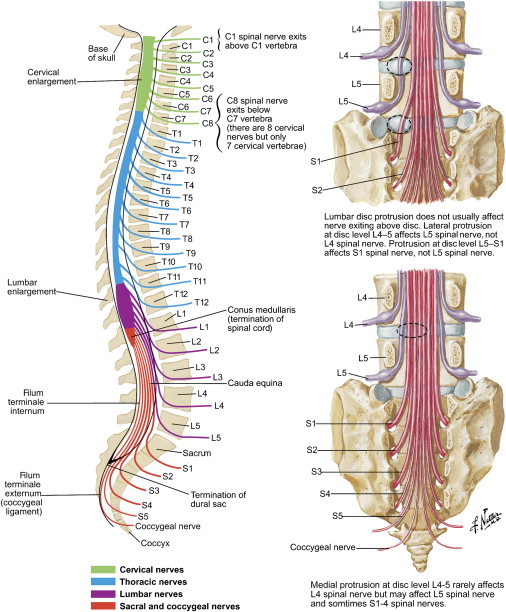
The spinal cord lies within the spinal canal of the vertebrae and is continuous with the medulla. It extends rostrally from the base of the foramen magnum to the distal L2 vertebra, where it ends as a conical structure known as the conus medullaris . Below the L2 level, nerve fibers of the cord continue as the cauda equina .
Thirty-one pairs of nerve roots extend from the spinal cord: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal. The nerves numbered 1 through 7 exit above the corresponding vertebrae, and the eighth cervical nerve slips between the seventh cervical and first thoracic vertebrae. For the thoracic and lumbar sections, each of the numbered nerves exits below the corresponding numbered vertebrae. Because the spinal cord is shorter than the spinal canal, the segments of the cord do not correspond below the cervical level. Therefore, the cervical vertebrae contain the cervical nerve segments, the thoracic vertebrae contain both the thoracic and lumbar nerve segments, and the top lumbar vertebrae contain the sacral nerve segments. For example, fractures at the T11-L1 vertebral level can affect the L1-S5 cord segments ( Fig. 1 ).
A cross-section of the cord reveals gray and white matter. The central gray matter may be divided into three horns: the posterior (dorsal) horn contains projections of cell bodies of sensory fibers from dorsal root ganglia, the lateral (intermediate) horn carries sympathetic neurons, and the anterior (ventral) horn contains motor neurons ( Fig. 2 ).
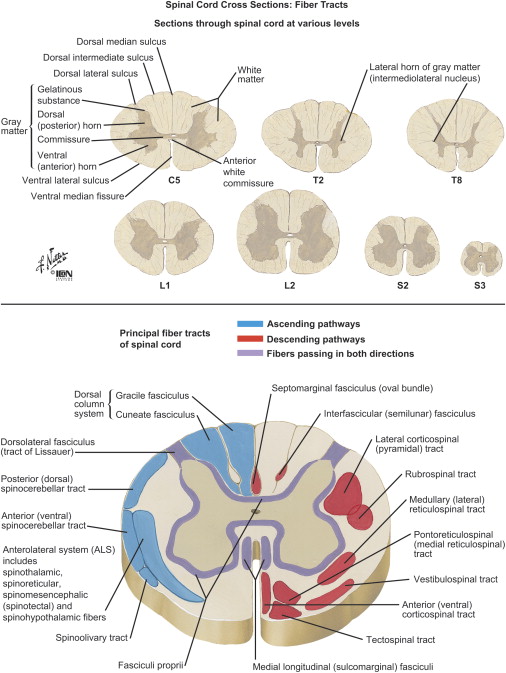
The surrounding white matter is divided into three main columns or tracts: posterior (dorsal) column carrying sensory information, lateral column relaying sensory and motor information, and anterior (ventral) column carrying primarily motor information (see Fig. 2 ).
Key tracts include (see Fig. 2 ) the dorsal columns (fasciculus gracilis and fasciculus cuneatus), which carry information for proprioception, vibration, and light touch; anterolateral spinothalamic tracts, which carry information for pain and temperature (lateral), and touch and pressure (anterior); and the corticospinal tract, which carries motor information.
Functional and clinical anatomy
The spinal cord serves as the relay tract that transfers motor information from the brain to the periphery, and receives sensory information distally and brings it centrally. It is protected and supported by meningeal coverings (the dura and pia mater), ligaments, and bony vertebrae (7 cervical, 12 thoracic, 5 lumbar, and 5 sacral). Blood supply to the spinal cord is provided by a single anterior spinal artery that supplies the anterior two thirds of cord, and two posterior spinal arteries that supply the posterior one third of the cord. Radicular arteries support the anterior and posterior spinal arteries. The artery of Adamkiewicz, a large lumbar radicular artery, supplies the midthoracic cord (T8-L1 vertebral level) and can be disrupted through injury to the thoracoabdominal aorta .
The spinal cord lies within the spinal canal of the vertebrae and is continuous with the medulla. It extends rostrally from the base of the foramen magnum to the distal L2 vertebra, where it ends as a conical structure known as the conus medullaris . Below the L2 level, nerve fibers of the cord continue as the cauda equina .
Thirty-one pairs of nerve roots extend from the spinal cord: 8 cervical, 12 thoracic, 5 lumbar, 5 sacral, and 1 coccygeal. The nerves numbered 1 through 7 exit above the corresponding vertebrae, and the eighth cervical nerve slips between the seventh cervical and first thoracic vertebrae. For the thoracic and lumbar sections, each of the numbered nerves exits below the corresponding numbered vertebrae. Because the spinal cord is shorter than the spinal canal, the segments of the cord do not correspond below the cervical level. Therefore, the cervical vertebrae contain the cervical nerve segments, the thoracic vertebrae contain both the thoracic and lumbar nerve segments, and the top lumbar vertebrae contain the sacral nerve segments. For example, fractures at the T11-L1 vertebral level can affect the L1-S5 cord segments ( Fig. 1 ).
A cross-section of the cord reveals gray and white matter. The central gray matter may be divided into three horns: the posterior (dorsal) horn contains projections of cell bodies of sensory fibers from dorsal root ganglia, the lateral (intermediate) horn carries sympathetic neurons, and the anterior (ventral) horn contains motor neurons ( Fig. 2 ).
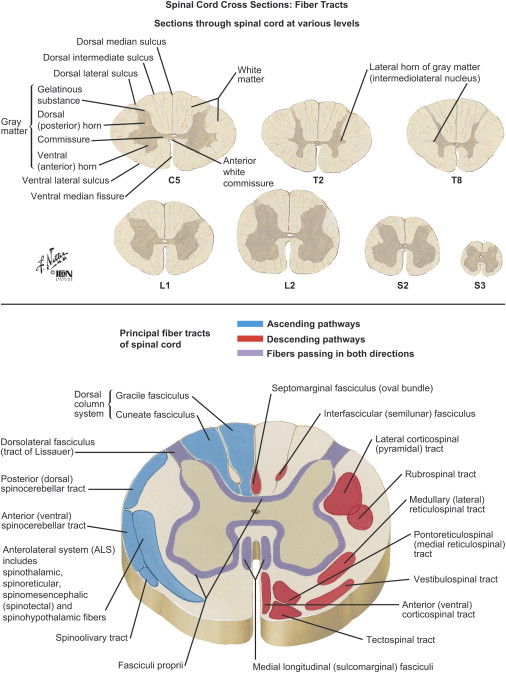
The surrounding white matter is divided into three main columns or tracts: posterior (dorsal) column carrying sensory information, lateral column relaying sensory and motor information, and anterior (ventral) column carrying primarily motor information (see Fig. 2 ).
Key tracts include (see Fig. 2 ) the dorsal columns (fasciculus gracilis and fasciculus cuneatus), which carry information for proprioception, vibration, and light touch; anterolateral spinothalamic tracts, which carry information for pain and temperature (lateral), and touch and pressure (anterior); and the corticospinal tract, which carries motor information.
Spinal cord injury examination
The International Standards for Neurological Classification of Spinal Cord Injury , guidelines created by the Neurological Standards Committee of the American Spinal Injury Association (ASIA) are widely used to classify spinal cord injuries. The Standards detail a neurologic examination testing 10 key muscle group (5 upper extremity and 5 lower extremity) sensations (light touch and pin prick) in 28 key dermatomes, and a rectal examination testing sensation and voluntary sphincter contraction (see Fig. 2 ).
Motor examination is performed by manual testing of 10 key muscle groups on the right and left sides of the body ( Table 1 ). Most muscles have multiple spinal segment innervation. The key muscles selected are innervated primarily by two segments, and the most rostral segment is assigned for every key muscle . With the patient in supine position, conventional muscle grading (0–5) is assigned to each muscle. The motor level of injury is defined by the lowest key muscle that has a grade of at least 3/5, provided that the key muscles above that level are graded 5/5 .
| Motor level | Muscles |
|---|---|
| C5 | Elbow flexors |
| C6 | Wrist extensors |
| C7 | Elbow extensors |
| C8 | Finger flexors |
| T1 | Finger abductors |
| L2 | Hip flexors |
| L3 | Knee extensors |
| L4 | Ankle dorsiflexors |
| L5 | Long toe extensors |
| S1 | Ankle dorsiflexors |
Sensation is tested for light touch and pinprick. Light touch is performed using a cotton wisp, with sensation graded on a scale of 0 to 2 (0 = absent; 1 = altered; 2 = normal). The face serves as normal. The examiner then tests each of the 26 dermatomes on both sides of the body and records the grade of sensation. Pinprick is tested using a safety pin, with sensation also graded on a scale of 0 to 2 (0 = absent or cannot distinguish sharp or dull; 1 = altered but can differentiate sharp from dull; 2 = normal). Similar to the light-touch portion of the examination, the face serves as a normal reference and each of the 28 key dermatomes on the right and left sides of the body are tested and recorded. The sensory level of injury is defined as the most caudal segment of the spinal cord, with normal sensory function on both right and left sides of the body. Muscles or sensory areas not able to be tested are recorded as “not tested.”
A neurologic level of injury is defined as the most caudal spinal cord segment with normal muscle testing and sensation. For dermatomes not covered by muscles (C1-C4, T2-L1, S1-S4-S5), the sensory level is used to identify the level of injury .
A rectal examination is performed to document the presence or absence of intact voluntary sphincter control and deep anal sensation. Results are recorded as “yes” or “no.” The presence of deep anal sensation may be the only indicator of an incomplete SCI.
A complete injury is defined as the absence of sensory and motor function in the lowest sacral segment. An incomplete injury is defined as partial preservation of sensory or motor function in the lowest sacral segments. The zone of partial preservation is used only with complete injuries and for documenting dermatomes and myotomes caudal to the neurologic level of injury that remain partially innervated. The zone of partial preservation is recorded for motor and sensation for the right and left sides.
The ASIA Impairment Scale (AIS) is used to grade the degree of impairment, and is defined as follows :
- •
Complete injury:
AIS A; absence of sensory and motor function at lowest sacral segment S4/5
- •
Incomplete injuries:
AIS B: sensory but no motor function below the neurologic level of injury, including the sacral segments S4/5
AIS C: Motor function is preserved below the neurologic level and more than half of key muscles graded show strength of less than 3/5
AIS D: Motor function is preserved below the neurologic level and more than half of the key muscles graded show strength greater than or equal to 3
AIS E: Normal sensory and motor strength
Acute spinal cord injury treatment
Comprehensive medical treatment for the person who sustains an SCI begins at the scene of the injury. Recognition of the potential for further cord injury has led to the widespread use of immediate spine immobilization for all SCIs or suspected SCIs. The main objectives of surgery are to decompress the spinal canal and achieve mechanical stability. An anterior or a posterior approach to decompression may be chosen. Instrumentation may be used to stabilize or augment a fusion. The surgeon determines the exact approach, which depends partly on the mechanism of injury. Flexion injuries may be associated with posterior spinal ligamentous disruption, which may not be apparent on plain radiographs but is with MRI . Imaging generally includes CT scans and plain films, and often MRI. Bone is better visualized with CT than MRI, but MRI is better for showing cord and ligamentous tissue damage. In SCI from gunshot wounds, surgical treatment is rarely indicated unless progressive neural injury is present.
The Jefferson fracture is a C1 (atlas) posterior ring burst fracture caused by axial load with hyperextension. C2 (axis) odontoid fractures are classified according to anatomic location of the fracture, and treatment depends on the type of injury. Subluxation of the axis on the C3 vertebra associated with a fracture is termed a Hangman’s Fracture . After surgical stabilization, most patients who have cervical injuries are immobilized with an orthosis for 8 to 12 weeks. In thoracolumbar injuries, a thoracic lumbar sacral orthosis (TLSO) is often used for 3 to 6 months according to surgeon recommendations. A recent report suggests that shorter periods of immobilization suffice after internal fixation .
Spinal orthoses
Cervical orthosis
The cervical spine has the most range of all the spine segments (eg, occiput/C1, flexion/extension; C1-C2 (atlantoaxial), rotation. Various orthoses are used in SCI. The Soft cervical collar is the most commonly used collar and is mainly used for cervical muscle strain relief. It is made of a firm foam material covered with cotton and causes minimal immobilization ( Fig. 3 ) . The Philadelphia collar is foam-reinforced and provides chin, occipital and upper chest support with minimal control of rotation and lateral bending. It is commonly used after cervical surgery and stable cervical fractures ( Fig. 4 ) . The Aspen collar is similar to the Philadelphia collar but offers slightly greater stability of lateral bending and rotation than a soft collar ( Fig. 5 ) . The Miami J collar is hard plastic with cloth pads and a tracheostomy cutout. It enables the best control of all movements . The Sternal Occipital Mandibular Immobilizer (SOMI) provides rigid chest support and has adjustable chin and occipital portions. It offers only moderate restraint of lateral bending and rotation, and is applied supine ( Fig. 6 ) . The Minerva brace is a cervical–thoracic brace with a chest plate and headband that provides immobilization from C1 to T1 ( Fig. 7 ) and the Halo vest is a cranial–thoracic brace with cranial fixation pins that provides maximal restriction of range of motion. Pin complications are common (eg, loosening, pain, infection, skin breakdown) ( Fig. 8 ) .
Thoracic, lumbar, and sacral orthoses
The lumbosacral corset has molded plastic or metal stays, and is used mainly for acute or chronic pain, with minimal immobilization ( Fig. 9 ) . The Taylor brace is a TLSO that is mainly used for counteracting kyphosis ( Fig. 10 ) . The Knight Taylor brace is a TLSO that provides moderate limitation of flexion/extension and lateral flexion and hyperextends the thoracic spine for bracing stable fractures and providing stability postsurgery (see Fig. 10 ) . The Jewett brace is a hyperextension TLSO that provides a three-point system to facilitate thoracic hyperextension, an anterior pad on the sternum and pubic symphysis, and a posterior pad on the thoracolumbar junction, and permits limited flexion ( Fig. 11 ) . The Cruciform Anterior Spinal Hyperextension (CASH) brace is also used for kyphosis. It consists of an anterior cross bar with pads at the four ends, and adjusts from the back. It is harder to use than the Jewett brace ( Fig. 12 ) . The Milwaukee brace is a cervical TLSO with lateral pads in noncircumferential arrangement. It is used mainly for idiopathic scoliosis and designed to cause active and passive forces to correct the curvatures ( Fig. 13 ) .







