Spinal Cord Injury
EPIDEMIOLOGY OF TRAUMATIC SCI
There are ≈12,000 new patients who survive SCI in the United States each year.1 Since 2005, the mean age at time of injury is 40.2 years.1 ♀:♂ = 4:1. Incomplete tetraplegia is the most common category, followed by complete paraplegia (22.9%), incomplete paraplegia (21.5%), and complete tetraplegia (16.9%).1
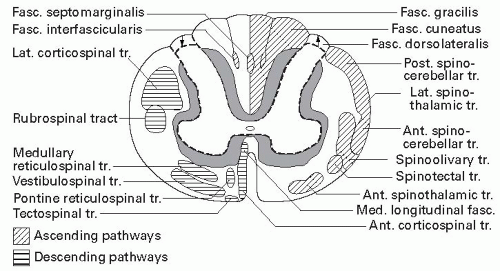
SELECTED TRACTS
The majority of descending corticospinal motor fibers cross at the medulla to become the lateral corticospinal tract (CST). A small number of CST fibers do not decussate at the medulla and descend via the anterior CST before crossing at the level of the anterior white commissure. Although often depicted in many representations of the spinal cord (see Fig. 21-1, right), the existence of a somatotopic organization of the lateral CST has been challenged.3
The ascending dorsal white columns cross in the medulla, via the medial lemniscus, then go on to the thalamus. These fibers carry joint position, vibration, and light touch (LT) sensation. The spinothalamic tracts, which carry pain, temperature, and nondiscriminative tactile sensations, cross to the contralateral side shortly after entry to the cord in the ventral white commissure of the spinal cord.
CLASSIFICATION OF SCI: INTERNATIONAL STANDARDS FOR THE NEUROLOGIC CLASSIFICATION OF SCI
1. Perform a supine sensory examination of the 28 dermatomes at the key sensory points for pin prick (PP) and LT, including rectal sensation. The sensory level is the most caudal level with intact (grade 2) sensation for both PP and LT.
Rectal sensory examination includes evaluation of deep rectal sensation as determined by the patient’s ability to feel the examiner’s finger during digital rectal examination.
2. Perform a supine motor examination of 10 key muscle groups and voluntary anal contraction. The motor level for each side is the most caudal level with grade ≥3, where all muscles rostral to it are grade 5.
3. Determine the single neurologic level, which is the most caudal level at which both sensory and motor modalities are intact bilaterally, as defined earlier.
4. Classify injury as complete or incomplete. Complete injuries have no motor or sensory function, including deep anal sensation, preserved in sacral segments S4-5. Somatosensory evoked potentials (SSEPs) may be useful in differentiating complete versus incomplete SCI in patients who are uncooperative or unconscious.
5. Categorize by American Spinal Injury Association (ASIA) Impairment Scale (AIS) A to E.
Determine the zone of partial preservation (ZPP) if ASIA A. ZPP is defined as preserved segments below the neurologic level of injury (NLOI) and used in complete injuries.
Important ASIA Key Sensory Points
C2 | Occipital protuberance | T1 | Medial epicondyle elbow | L3 | Medial anterior knee |
C3 | Supraclavicular fossa | T2 | Apex of the axilla | L4 | Medial malleolus |
C4 | Top of the AC joint | T4 | Medial to nipple | L5 | Web space between first and second toes |
C5 | Lateral antecubital fossa | T10 | Lateral to umbilicus | S1 | Lateral heel |
C6 | Dorsal proximal thumb | T12 | Inguinal ligament | S2 | Lateral popliteal fossa |
C7 | Dorsal proximal middle finger | L1 | Between T12 and L2 | S3 | Ischial tuberosity |
C8 | Dorsal proximal fifth finger | L2 | Medial anterior thigh | S4-5 | Anal mucocutaneous junction |
ASIA Key Muscles
C5 | Elbow flexors | T1 | Small finger abductors | L5 | Extensor hallucis longus |
C6 | Wrist extensors | L2 | Hip flexors | S1 | Ankle plantar flexors |
C7 | Elbow extensors | L3 | Knee extensors | ||
C8 | Flexor digitorum profundus of third digit | L4 | Ankle dorsiflexors |
Sensory levels are scored as 0 (absent), 1 (impaired, including hyperesthesia), 2 (normal), or not testable (NT). When scoring PP, inability to distinguish PP from LT is scored 0/2. Muscles are graded from 0 (total paralysis) to 5 (normal active movement with full ROM against full resistance), or NT.
ASIA Impairment Scale, Revised (2000)
A Complete – No sensory or motor function is preserved in the lowest sacral segments S4-5. The ZPP (only used in ASIA A) refers to the most caudal segment below the level of injury with partial sensory or motor function.
B Incomplete – Sensory but no motor function is preserved below the neurologic level and must include sacral segments S4-5.
C Incomplete – Motor function is preserved more than three levels below the neurologic level, and more than half of the key muscles below the neurologic level have a muscle grade <3.
D Incomplete – Motor function is preserved more than three levels below the neurologic level, and at least half of the key muscles below the neurologic level have a muscle grade ≥3.
E Normal – LT, PP, and motor function of the key muscles are normal.4
Note: For an individual to receive a grade of ASIA C or D, there must be sensory or motor S4-5 sparing. In addition, the individual must have either (1) voluntary anal sphincter contraction or (2) sparing of motor function more than three levels below the motor level.
SCI CLINICAL SYNDROMES
Central Cord – This incomplete syndrome is typically seen in older persons with cervical spondylosis who experience neck hyperextension injury, resulting in greater upper limb rather than lower limb impairment. Bowel, bladder, and sexual dysfunction are variable. The postulated mechanism of injury involves cord compression both anteriorly and posteriorly, with inward bulging of the ligamentum flavum during hyperextension in a stenotic spinal canal.5 Penrod6 retrospectively studied 51 patients with central cord syndrome and noted better overall recovery of ambulation, self-care, and bowel/bladder function in patients <50 years of age than their older counterparts at time of discharge from rehabilitation.
Brown-Séquard – Hemisection of the cord produces ipsilateral weakness and proprioceptive loss and contralateral loss of PP and temperature sense. The prognosis for ambulation is best among the incomplete SCI syndromes.
Anterior Cord – There is variable loss of motor and PP sensation, with relative preservation of proprioception and LT. Prognosis for motor recovery is generally considered poor. Typically, the anterior cord syndrome results from a vascular lesion in the territory of the anterior spinal artery, but it may also be seen resulting from retropulsed disks/vertebral fragments. Intraoperative SSEPs, which primarily monitor the posterior column pathways, may miss the development of an anterior cord syndrome.
Cauda Equina – Cauda equina injuries may be due to neural canal compression or fractures of the sacrum or spine at L2 or below. While the damage occurs within the spinal cord, the syndrome can be described as “multiple lumbosacral radiculopathies,” since the cauda is comprised
of lumbosacral nerve roots. Sequelae depend on the roots involved but usually involve impairment of bowel, bladder, and sexual function. Areflexia, saddle anesthesia, and lower limb weakness are also characteristic. Radicular neuropathic pain is common and can be severe. Recovery is possible because the nerve roots can recover. Consultation for possible early surgery is indicated.
of lumbosacral nerve roots. Sequelae depend on the roots involved but usually involve impairment of bowel, bladder, and sexual function. Areflexia, saddle anesthesia, and lower limb weakness are also characteristic. Radicular neuropathic pain is common and can be severe. Recovery is possible because the nerve roots can recover. Consultation for possible early surgery is indicated.
Conus Medullaris – A pure conus medullaris lesion (e.g., intramedullary tumor) results in saddle anesthesia and bladder, sphincter, and sexual dysfunction due to cord injury at the S2-4 segments. Anal cutaneous and bulbocavernosus (S2-4) and ankle deep tendon reflexes (S1,S2) may be either absent or preserved depending upon whether the lesion is “high” in the conus. Prognosis for recovery is poor. Conus lesions due to trauma (e.g., L1 vertebral body fracture) are typically accompanied by injury of some of the lumbosacral nerve roots, resulting in a variable degree of lower limb dysfunction.
BASIS FOR ACUTE INTERVENTIONS
High-dose steroids have been reported to be neuroprotective in acute SCI by inhibiting lipid peroxidation and scavenging free radicals. The use of IV methylprednisolone (MP) in acute nonpenetrating traumatic SCI is supported by the National Acute Spinal Cord Injury Studies (NASCIS).7,8 The results of the NASCIS trials, however, have been challenged by some authors and organizations.9,10
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree