Soft Tissue Coverage of Fingertip Amputations
Jennifer Etcheson
Jeffrey Yao
DEFINITION
A fingertip injury or amputation involves trauma to the finger distal to the distal interphalangeal (DIP) crease.
The fingertip is the most sensitive area of the hand.
Fingertip injuries are common, accounting for 45% of emergency room hand injuries.
ANATOMY
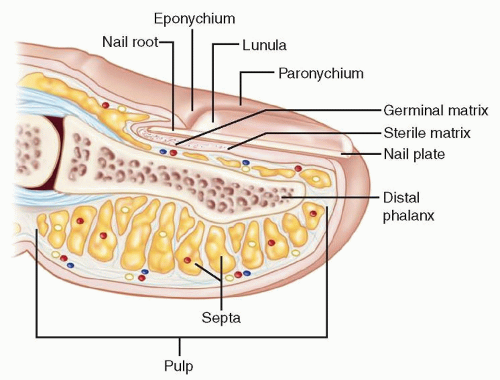
FIG 1 depicts the anatomy of the fingertip.
Eponychium: the cuticle or the thin membrane over the dorsum of the nail at the nail fold
Perionychium: the skin at the lateral nail margin
Hyponychium: the skin below the distal aspect of the nail plate, consisting of a mass of keratin with a high concentration of lymphocytes and polymorphonuclear cells; serves as a barrier to infection
Nail root: portion of the nail plate proximal to the eponychial fold
Lunula: the curved white opacity representing the distal, visible portion of the germinal matrix
Germinal matrix: produces 90% of the nail plate volume
Sterile matrix: contributes to nail plate adherence
Nail plate: consists of flattened sheets of anuclear keratinized epithelium
Nail bed: the floor of the nail plate, comprising proximal germinal matrix and distal sterile matrix
Distal phalanx: lies deep to the nail bed
Pulp: composed of fibrous septa
Fingertip Amputation Classification (Tamai)
Zone I: distal to lunula
Zone II: DIP joint to lunula
PATHOGENESIS
Various mechanisms of trauma
Avulsion
Crush
Compression
Sharp
Dull
NATURAL HISTORY
Fingertip injuries with no bone exposed will ultimately heal by secondary intention.
In the setting of wounds less than 1 cm2, secondary intention healing aided by daily dressing changes actually allows for increased recovery of sensation.
The use of secondary intention healing for larger injuries involves a prolonged period of dressing changes with associated risk of infection and unfavorable scarring.
PATIENT HISTORY AND PHYSICAL FINDINGS
Full history and physical examination
Mechanism of injury
Age
Handedness
Occupation
Level of cooperation and understanding
Injury assessment
Digit or digits involved: thumb versus finger
Transverse versus dorsal oblique-volar oblique versus radial-ulnar
Damage to nail or nail bed
Exposure of bone
Static and moving two-point discrimination: There is decreased density of innervation with increased two-point discrimination.
Terminal flexion and extension: Injury to tendons will require more significant flap coverage.
Vascularity: Prolonged capillary refill is suggestive of arterial injury.
IMAGING AND OTHER DIAGNOSTIC STUDIES
Plain radiographs in orthogonal planes (posteroanterior, lateral)
NONOPERATIVE MANAGEMENT
Most fingertip amputations may be treated at the bedside using sterile technique and employing a metacarpal block, finger tourniquet, and loupe magnification.
There should be a low threshold for operative management.
If no bone is exposed, options include healing by secondary intention, primary closure, or skin grafting.
Secondary intention healing aided by daily dressing changes provides the best recovery of sensation and is appropriate for wounds less than 1 cm2.
Primary closure is an option only if there is minimal skin loss.
Tight closures should be avoided. This can minimize function by causing joint contracture and distal tip tenderness due to poor soft tissue coverage of the bony prominences.
Sewing the volar skin tightly to the distal nail may result in a cosmetically displeasing hook nail.
If a nail bed laceration is suspected, the nail plate should be removed with a Freer elevator, allowing repair of the nail bed with either 6-0 or 7-0 simple interrupted absorbable sutures (chromic gut). Loupe magnification is extremely helpful.
The eponychial fold should be stented open with either trimmed and carefully cleansed nail or other material (eg, foil from a suture pack) to prevent abnormal growth of the future nail.
With amputations through the germinal matrix, any remaining unrepairable matrix should be removed to prevent formation of a painful nail remnant.
SURGICAL MANAGEMENT
The decision to take a patient with a fingertip injury to the operating room depends on the size of the defect, presence of exposed bone, angle of amputation, willingness of the patient to do dressing changes, and surgeon experience.
The goals are to preserve function and sensation and allow early return to activity.
In terms of functional outcome, healing by secondary intention provides equal or better results for defects less than 1 cm in diameter.
Full-thickness grafts are preferable to split-thickness grafts.
Split-thickness grafts should be used only on the ulnar side of the index, middle, and ring fingers.
Donor site options include the volar wrist skin (should be avoided, as it can mimic a suicide attempt laceration), antecubital skin, medial upper arm skin, and hypothenar skin.
These donor sites can be closed primarily.
If salvageable, the original skin from the amputated segment can be defatted and applied as a graft/biologic dressing.
If bone is exposed, options include bone shortening and primary closure and bone shortening and healing by secondary intention or fingertip flaps.
Preoperative Planning
Preliminary irrigation and débridement, exploration
Antibiotics
Patient comorbidities
Is the patient a diabetic? smoker? recreational drug user?
Is the tetanus status up-to-date?
Anesthesia assessment
Positioning
Supine with standard hand table. An arm, forearm, or digital tourniquet is used. The arm is placed in the center of the hand table for equal access by the surgeon and assistant.
Approach
Once the decision to perform a flap has been made, the angle of amputation, patient age, and patient gender determines whether an advancement or regional flap is appropriate.
TECHNIQUE
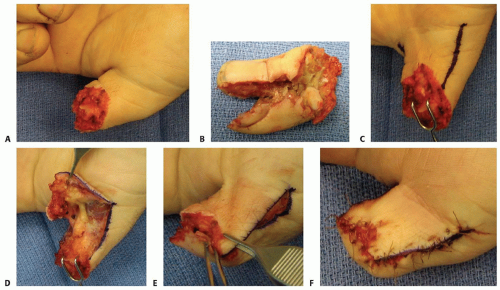
▪ Skin Grafting
Measure the size of the defect carefully and create a template.
This template is used to draw a corresponding defect on the donor site (TECH FIG 1A).
Harvest the full-thickness graft with a no. 15 blade. Take great care to defat the graft down to dermis (TECH FIG 1B,C).
Sew the graft into place and secure it using absorbable suture (TECH FIG 1D).
At four corners, the suture is left long so that later it may be tied over a bolster.
Cover the skin graft with Xeroform dressing and mineral oil-soaked sterile cotton balls.
Tie down the four long sutures over the cotton balls to create a bolster, placing gentle pressure on the graft to minimize shear.
The finger is padded with gauze and protected with a finger splint, leaving the proximal interphalangeal (PIP) joint free for 5 to 7 days.
After 5 to 7 days, the splint and dressing should be carefully removed, the graft inspected, and daily Xeroform dressing changes instituted until the graft is fully healed.
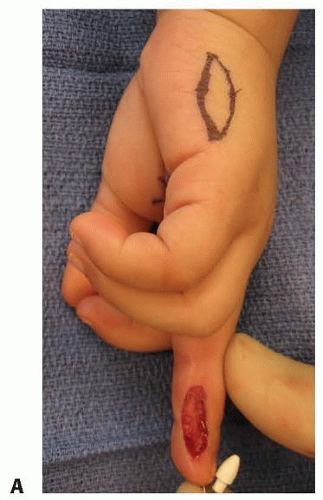 TECH FIG 1 • A. Ulnar defect of the long finger with the proposed hypothenar graft drawn out. (continued) |
▪ Moberg Advancement Flap
Indication: thumb tip amputation less than 1.5 cm; preserves sensation and length (TECH FIG 2A,B).
Not indicated for fingertip amputations.
Make a longitudinal incision just dorsal to the neurovascular bundles, based at the metacarpophalangeal joint flexion crease (TECH FIG 2C).
Elevate a flap elevated from the flexor sheath (TECH FIG 2D).
If the flap is difficult to advance, consider the following (TECH FIG 2E):
Flexing the interphalangeal joint
Extending the lateral incisions toward the palm with excision of skin at base to create an island flap; skin grafting of the secondary defect
Excise a triangle of skin at the bilateral flap base (ie, triangle of Burow).
Carefully preserve bridging vessels.
Close with permanent suture under minimal tension (TECH FIG 2F).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree