This article presents a concise description and literature review of the eLibra Dynamic Ligament Balancing Device in total knee arthroplasty. This device is a force sensor that allows surgeons to balance the medial and lateral collateral ligaments during total knee replacement. This instrument provides precise, quantitative, digital information in newtons during surgery that allows surgeons to accurately externally rotate the femoral component in order to balance the forces across the medial and lateral compartments. The device is highly accurate and simple to use. It relies on objective dynamic data to balance the knee rather than static landmarks or subjective tensiometers.
Key points
- •
The eLibra device uses quantitative real-time data to balance the knee as opposed to static landmarks for external rotation of the femoral component.
- •
The medial collateral ligament (MCL) and lateral collateral ligament (LCL) are balanced through bone cuts rather than ligament releases.
- •
The device is simple to use, highly accurate, and reproducible.
- •
Use of this device greatly reduces the need for ligament releases and confirms precise balance when used in combination with computer-assisted navigation, patient-specific cutting guides, or conventional arthroplasty.
Introduction
Total knee arthroplasty (TKA) remains one of the most successful surgical procedures in the world. It is a clinical fact that this procedure, properly performed, improves pain, increases range of motion, and improves the quality of life for patients undergoing this procedure. The success of TKA largely depends on restoration of the integrity of the articular surfaces of the knee joint as well as realignment of the entire lower extremity to a neutral or an anatomic mechanical axis.
The 2 critical elements of TKA, in terms of restoration of the joint surfaces and realignment of the limb, are the bone cuts and appropriate and reproducible soft tissue balancing, particularly in flexion. Initially, the procedure relied on rudimentary instruments to achieve appropriate osteotomies. Over the past 2 to 3 decades, there have been major advances in the instruments available to perform correct and reproducible bony cuts. Initially, intramedullary instrumentation was shown particularly accurate in terms of bony resurfacing. This led to the development of extramedullary guides to do the same.
Over the past 10 years, there have been enormous advances in bone preparation with the development of computer-assisted navigation and validation techniques as well as, recently, the advent of image-guided preoperative patient-specific instrumentation systems. These systems use preoperative MRI- or CT-based technology to rapidly produce a set of cutting jigs specifically designed to reproduce a patient’s normal knee anatomy, eliminating the need for intramedullary or extramedullary preparation and shown to be highly accurate and to reduce outliers.
Despite these advances in bone preparation, little has been done to assist surgeons in appropriate soft tissue balancing. Precise osteotomies ensure appropriate prosthetic fit but do little to ensure ligamentous stability and balance. Instability and improper balance have been shown to lead to condylar liftoff, flexion instability, accelerated prosthetic wear, aseptic loosening, patellar maltracking, anterior knee pain, and overall increase in mechanical failure.
Soft tissue balance remains largely technique driven and highly dependent on the discretion of the operative surgeon. Osteotomies are usually completed; then, the surgeon ensures appropriate range of motion and stability by individually testing the MCL, LCL, and anterior-to-posterior stability in extension, flexion, and throughout the range of motion. Balance is then achieved through ligamentous releases and/or repeat osteotomies. Typically, after years of experience and numerous procedures, a surgeon develops the ability to accurately assess stability in the varus/valgus and anterior/posterior planes.
This article discusses a new intraoperative device designed to assist surgeons with soft tissue balance primarily in flexion. The eLibra Dynamic Knee Balancing System (Zimmer, Warsaw, Indiana) provides a quantitative way to measure the compressive forces across the knee joint in the medial and lateral compartments in flexion and extension. The surgeon then reverses the traditional order of steps in the surgery, balancing the flexion space with the aid of the eLibra to externally rotate the trial component before the finishing femoral anteroposterior (AP) cuts are made. Rather than relying on the typical bone landmarks of 3° of posterior condylar rotation, Whiteside line, or the transepicondylar axis (TEA), flexion balanced is achieved by rotating the femoral trial to equalize compressive forces relative to the resected tibia on the force sensor.
This process takes into account 3 critical anatomic structures: the tibial osteotomy in terms of varus valgus alignment, the MCL, and the LCL. All have been shown of primary importance in soft tissue balancing.
After equalization of the compressive forces on both sides of the joint in 90° of flexion, the final femoral cuts are completed prior to any releases, eliminating or minimizing the need for soft tissue balancing after implantation of the trial or actual components. Dynamic balance is then achieved through a process termed, balanced resection , which is a combination of gap balancing and measured resection techniques.
This article describes the eLibra device and its application in terms of a quantitative measure of gap balancing. This device gives real-time objective data, similar to navigation data, with reference to the medial and lateral compressive forces across the joint.
In describing the device, 4 learning objectives are focused on:
- 1.
Description of the normal balancing forces across the knee joint in TKA, including traditional means of achieving balance
- 2.
Description of the design rationale and technical specifications of the eLibra Dynamic Knee Balancing System
- 3.
The use of the eLibra Dynamic Knee Balancing Knee System to balance the knee and obtain objective data regarding medial and lateral compressive forces across the knee joint in flexion and extension
- 4.
Early results using this device in the published literature
Knee joint stability and achieving balance
The knee joint is an inherently unstable articulation and relies on both static and dynamic stabilizers to achieve stability. Static stabilizers are the MCL, the LCL, the anterior and posterior cruciate ligaments, and the posterior capsule. Current total knee designs sacrifice the anterior and/or the posterior cruciate ligaments, relying on inherent prosthetic stability for anterior-to-posterior constraint with a dished tibial articular polyethylene or a post-and-cam mechanism. The medial lateral stability comprises the MCL and LCL and to some extent the posterior capsule in extension. Appropriate balance of these structures is critical to overall stability of the prosthetic joint, and imbalance of these structures can lead to instability, particularly in flexion; accelerated wear; and overall poor performance of the arthroplasty. Both the MCL and the LCL can be divided into anterior and posterior halves: the anterior half is maximally tight inflexion and the posterior half is tight in full extension. Many investigators have postulated that arthritis and joint destruction is a disease of not only the condylar surfaces but also the ligaments themselves. Thus TKA must address the ligaments as well. In the extreme, this process involves complete stripping of the entire posterior medial corner or the lateral structures in a tight valgus knee. The author believes that the amount of ligamentous release can be and should be dictated by the preexisting varus or valgus deformity and the ability to passively correct the deformity preoperatively. A passively correctible deformity requires little or no ligamentous releases and can usually be completely balanced through the bone cuts with the eLibra. A fixed varus or valgus deformity most likely requires some release to correct the deformity and balance the flexion and extension gaps.
There are also several dynamic stabilizers of the knee joint. The anterior structures include the quadriceps muscle and tendon, the patella, and the patellar ligament, collectively known as the extensor mechanism. The posterior structures include the medial and lateral hamstrings, which actively flex the joint, resist in extension, and provide some dynamic rotational stability. Also, the popliteus muscle assists in controlling internal rotation of the femur on the tibia.
It is the complex interplay between the static and dynamic stabilizers of the knee joint that is critical to the medial and lateral balance of the prosthetic knee joint. The interplay is so complex that individually measuring each component is impossible. This interplay is where the eLibra helps surgeons. Balance is achieved through bone cuts, not violation of the soft tissue. The balance is ensured prior to the osteotomies and confirmed with precise objective feedback.
Introduction
Total knee arthroplasty (TKA) remains one of the most successful surgical procedures in the world. It is a clinical fact that this procedure, properly performed, improves pain, increases range of motion, and improves the quality of life for patients undergoing this procedure. The success of TKA largely depends on restoration of the integrity of the articular surfaces of the knee joint as well as realignment of the entire lower extremity to a neutral or an anatomic mechanical axis.
The 2 critical elements of TKA, in terms of restoration of the joint surfaces and realignment of the limb, are the bone cuts and appropriate and reproducible soft tissue balancing, particularly in flexion. Initially, the procedure relied on rudimentary instruments to achieve appropriate osteotomies. Over the past 2 to 3 decades, there have been major advances in the instruments available to perform correct and reproducible bony cuts. Initially, intramedullary instrumentation was shown particularly accurate in terms of bony resurfacing. This led to the development of extramedullary guides to do the same.
Over the past 10 years, there have been enormous advances in bone preparation with the development of computer-assisted navigation and validation techniques as well as, recently, the advent of image-guided preoperative patient-specific instrumentation systems. These systems use preoperative MRI- or CT-based technology to rapidly produce a set of cutting jigs specifically designed to reproduce a patient’s normal knee anatomy, eliminating the need for intramedullary or extramedullary preparation and shown to be highly accurate and to reduce outliers.
Despite these advances in bone preparation, little has been done to assist surgeons in appropriate soft tissue balancing. Precise osteotomies ensure appropriate prosthetic fit but do little to ensure ligamentous stability and balance. Instability and improper balance have been shown to lead to condylar liftoff, flexion instability, accelerated prosthetic wear, aseptic loosening, patellar maltracking, anterior knee pain, and overall increase in mechanical failure.
Soft tissue balance remains largely technique driven and highly dependent on the discretion of the operative surgeon. Osteotomies are usually completed; then, the surgeon ensures appropriate range of motion and stability by individually testing the MCL, LCL, and anterior-to-posterior stability in extension, flexion, and throughout the range of motion. Balance is then achieved through ligamentous releases and/or repeat osteotomies. Typically, after years of experience and numerous procedures, a surgeon develops the ability to accurately assess stability in the varus/valgus and anterior/posterior planes.
This article discusses a new intraoperative device designed to assist surgeons with soft tissue balance primarily in flexion. The eLibra Dynamic Knee Balancing System (Zimmer, Warsaw, Indiana) provides a quantitative way to measure the compressive forces across the knee joint in the medial and lateral compartments in flexion and extension. The surgeon then reverses the traditional order of steps in the surgery, balancing the flexion space with the aid of the eLibra to externally rotate the trial component before the finishing femoral anteroposterior (AP) cuts are made. Rather than relying on the typical bone landmarks of 3° of posterior condylar rotation, Whiteside line, or the transepicondylar axis (TEA), flexion balanced is achieved by rotating the femoral trial to equalize compressive forces relative to the resected tibia on the force sensor.
This process takes into account 3 critical anatomic structures: the tibial osteotomy in terms of varus valgus alignment, the MCL, and the LCL. All have been shown of primary importance in soft tissue balancing.
After equalization of the compressive forces on both sides of the joint in 90° of flexion, the final femoral cuts are completed prior to any releases, eliminating or minimizing the need for soft tissue balancing after implantation of the trial or actual components. Dynamic balance is then achieved through a process termed, balanced resection , which is a combination of gap balancing and measured resection techniques.
This article describes the eLibra device and its application in terms of a quantitative measure of gap balancing. This device gives real-time objective data, similar to navigation data, with reference to the medial and lateral compressive forces across the joint.
In describing the device, 4 learning objectives are focused on:
- 1.
Description of the normal balancing forces across the knee joint in TKA, including traditional means of achieving balance
- 2.
Description of the design rationale and technical specifications of the eLibra Dynamic Knee Balancing System
- 3.
The use of the eLibra Dynamic Knee Balancing Knee System to balance the knee and obtain objective data regarding medial and lateral compressive forces across the knee joint in flexion and extension
- 4.
Early results using this device in the published literature
Knee joint stability and achieving balance
The knee joint is an inherently unstable articulation and relies on both static and dynamic stabilizers to achieve stability. Static stabilizers are the MCL, the LCL, the anterior and posterior cruciate ligaments, and the posterior capsule. Current total knee designs sacrifice the anterior and/or the posterior cruciate ligaments, relying on inherent prosthetic stability for anterior-to-posterior constraint with a dished tibial articular polyethylene or a post-and-cam mechanism. The medial lateral stability comprises the MCL and LCL and to some extent the posterior capsule in extension. Appropriate balance of these structures is critical to overall stability of the prosthetic joint, and imbalance of these structures can lead to instability, particularly in flexion; accelerated wear; and overall poor performance of the arthroplasty. Both the MCL and the LCL can be divided into anterior and posterior halves: the anterior half is maximally tight inflexion and the posterior half is tight in full extension. Many investigators have postulated that arthritis and joint destruction is a disease of not only the condylar surfaces but also the ligaments themselves. Thus TKA must address the ligaments as well. In the extreme, this process involves complete stripping of the entire posterior medial corner or the lateral structures in a tight valgus knee. The author believes that the amount of ligamentous release can be and should be dictated by the preexisting varus or valgus deformity and the ability to passively correct the deformity preoperatively. A passively correctible deformity requires little or no ligamentous releases and can usually be completely balanced through the bone cuts with the eLibra. A fixed varus or valgus deformity most likely requires some release to correct the deformity and balance the flexion and extension gaps.
There are also several dynamic stabilizers of the knee joint. The anterior structures include the quadriceps muscle and tendon, the patella, and the patellar ligament, collectively known as the extensor mechanism. The posterior structures include the medial and lateral hamstrings, which actively flex the joint, resist in extension, and provide some dynamic rotational stability. Also, the popliteus muscle assists in controlling internal rotation of the femur on the tibia.
It is the complex interplay between the static and dynamic stabilizers of the knee joint that is critical to the medial and lateral balance of the prosthetic knee joint. The interplay is so complex that individually measuring each component is impossible. This interplay is where the eLibra helps surgeons. Balance is achieved through bone cuts, not violation of the soft tissue. The balance is ensured prior to the osteotomies and confirmed with precise objective feedback.
Traditional balancing techniques
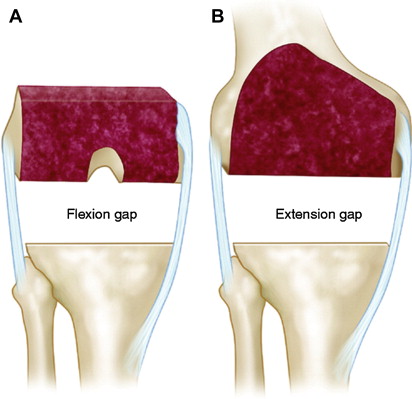
Soft tissue balance in knee arthroplasty has 2 schools of thought: measured resection versus gap balancing. Both methods are designed to create a symmetric flexion space by resection of the posterior condyles to match the symmetric extension space created by the distal femoral osteotomy.
The measured resection technique relies on 1 or all of 3 anatomic bony references to achieve resection:
- 1.
TEA
- 2.
Posterior femoral condyles
- 3.
Anterior posterior axis (Whiteside line)
Gap balancing relies on the femoral component positioned parallel to the resected proximal tibia with each collateral ligament equally tensioned in flexion. This typically requires the use of tensiometers or laminar spreaders and is inherently subjective, requires experience, and is difficult to master.
The eLibra device relies on ligament tensioning but in an objective clinically relevant manner ( Fig. 1 ).

Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree




