3 Shoulder Injuries
Background
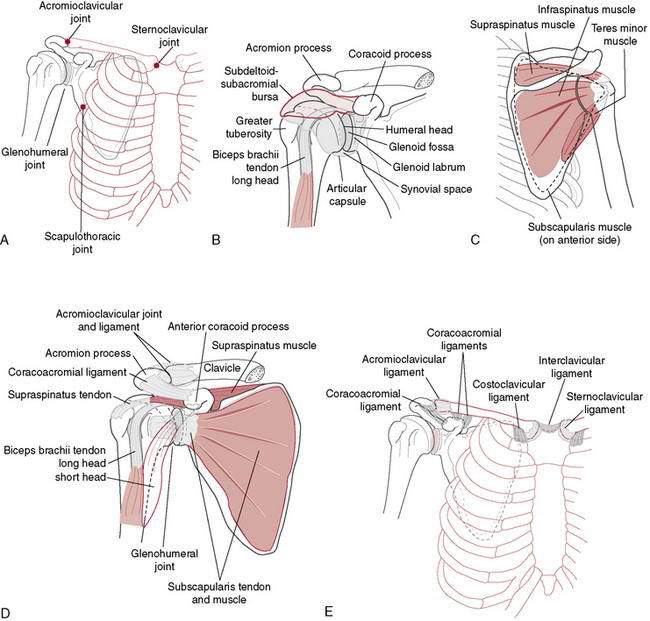
“Unrestricted” motion occurs at the GH joint as a result of its osseous configuration (Fig. 3-1). A large humeral head articulating with a small glenoid socket allows extremes of motion at the expense of the stability that is seen in other joints (Table 3-1). Similarly, the scapula is very mobile on the thoracic wall. This enables it to follow the humerus, positioning the glenoid appropriately while avoiding humeral impingement on the acromion. Osseous stability of the GH joint is enhanced by the fibrocartilaginous labrum, which functions to enlarge and deepen the socket while increasing the conformity of the articulating surfaces. However, the majority of the stability at the shoulder is determined by the soft tissue structures that cross it. The ligaments and capsule form the static stabilizers and function to limit translation and rotation of the humeral head on the glenoid. The superior GH ligament has been shown to be an important inferior stabilizer. The middle GH ligament imparts stability against anterior translation with the arm in external rotation and abduction less than 90 degrees. The inferior GH ligament is the most important anterior stabilizer with the shoulder in 90 degrees of abduction and external rotation, which represents the most unstable position of the shoulder (Fig. 3-2).
Table 3-1 Normal Joint Motions and Bony Positions Around the Shoulder Joint
| Scapula | |
| Rotation through arc of 65 degrees with shoulder abduction | |
| Translation on thorax up to 15 cm | |
| Glenohumeral Joint | |
| Abduction | 140 degrees |
| Internal/external rotation | 90 degrees/90 degrees |
| Translation | |
| Anterior–posterior | 5–10 mm |
| Inferior–superior | 4–5 mm |
| Total rotations | |
| Baseball | 185 degrees |
| Tennis | 165 degrees |
The muscles make up the dynamic stabilizers of the GH joint and impart stability in a variety of ways. During muscle contraction, they provide increased capsuloligamentous stiffness, which increases joint stability. They act as dynamic ligaments when their passive elements are put on stretch (Hill 1951). Most important, they make up the components of force couples that control the position of the humerus and scapula, helping to appropriately direct the forces crossing the GH joint (Poppen and Walker 1978) (Table 3-2).
Table 3-2 Forces and Loads on the Shoulder in Normal Athletic Activity
| Rotational Velocities | |
|---|---|
| Baseball | 7000 degrees/sec |
| Tennis serve | 1500 degrees/sec |
| Tennis forehand | 245 degrees/sec |
| Tennis backhand | 870 degrees/sec |
| Angular Velocities | |
| Baseball | 1150 degrees/sec |
| Acceleration Forces | |
| Internal rotation | 60 Nm |
| Horizontal adduction | 70 Nm |
| Anterior shear | 400 Nm |
| Deceleration Forces | |
| Horizontal abduction | 80 Nm |
| Posterior shear | 500 Nm |
| Compression | 70 Nm |
General Principles of Shoulder Rehabilitation
Designing a rehabilitation program should take several factors into account:
Importance of the History in the Diagnosis of Shoulder Pathology
Richard Romeyn, MD, and Robert C. Manske, PT, DPT, SCS, MEd, ATC, CSCS
When taking a history, the crucial elements about which one must inquire are as follows:
Scapulothoracic Dyskinesia, Core Stability Deficits, and Other Fitness or Technique-Related Provocations
General shoulder rehabilitation goals
Range of Motion
Once the intake evaluation is completed, the therapist should be more comfortable anticipating the patient’s response to the therapeutic regimen. One of the main keys to recovery is to normalize motion. Early professions relied on visual estimations or “quick” tests to assess shoulder motion. These tests include combined shoulder movements such as the Apley’s scratch test (Fig. 3-3), reaching across the body to the other shoulder (Fig. 3-4), or reaching behind the back to palpate the highest spinous process (Fig. 3-5). These quick tests are great to observe for overall asymmetry, but they cannot give an idea of isolated losses objectively.

Figure 3-5 Reaching behind the back to palpate the highest spinous process to determine range of motion.
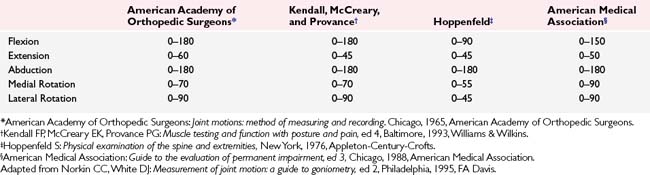
Even more important is regaining normal arthrokinematic motions at the shoulder. Active shoulder range of motion is always gathered before passive motions (Manske and Stovak 2006). Active shoulder ROM is seen in Table 3-3 (Manske and Stovak 2006). Many times, gross overall shoulder motion may only appear to be slightly limited, whereas arthrokinematic motion is drastically dysfunctional. For example, it is not uncommon for a patient to have full glenohumeral motion, yet impinge as a result of altered scapulohumeral motion from a restricted inferior or posterior shoulder capsule creating obligate humeral translations.
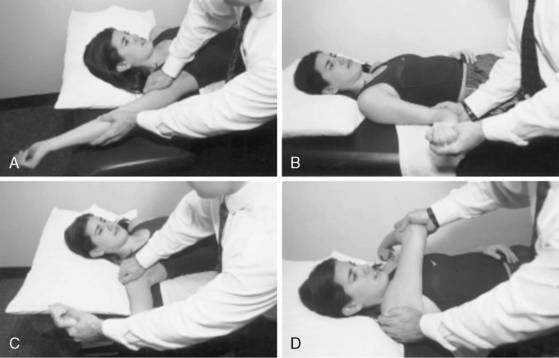
Therefore, it is imperative to also ensure evaluation of isolated glenohumeral motions is performed. One of the more common problematic limited motions with a variety of shoulder conditions is that of the posterior or inferior shoulder structures. Debate continues as to whether this is a result of capsular or other soft tissues. Regardless, it becomes an issue whenever elevation of the glenohumeral joint is required because it may increase the risk of impingement. Assessment of the posterior shoulder can be done by measuring isolated glenohumeral internal rotation. To perform this test the humerus is taken into passive internal rotation while the scapular is stabilized by grasping the coracoid process and the spine and monitoring for movement (Fig. 3-6). When passive slack from the posterior shoulder is taken up, the humerus will no longer internally rotate or resistance to movement will allow the scapula to tilt forward. When motion is detected or internal rotation has ceased, the examiner measures isolated glenohumeral internal rotation. Wilk et al. (2009) have shown this to be moderately reliable, whereas Manske et al. using the same technique have proved excellent test–retest reliability (Manske et al. 2010). This motion should be compared bilaterally to assess for a deficit between involved and uninvolved shoulders. A difference of greater than 20 degrees of internal rotation is thought to be a precursor to shoulder pathology. Loss of shoulder internal rotation is not always pathologic because some of this motion may be lost as a result of bony changes in the humerus. The concept of total shoulder rotation ROM should also be mentioned. By adding the two numbers of GH internal rotation and external rotation together, a composite of total shoulder motion can be obtained (Fig. 3-7). Ellenbecker et al. (2002), measuring bilateral total rotation range of motion in professional baseball and elite junior tennis players, found that although a dominant arm may show increased external rotation and less internal rotation, the total ROM was not significantly different when comparing the two shoulders. Therefore, one needs to not only address the internal rotation loss, but also should ensure that the total range of motion is not limited. Using normative data from population specific research can assist the therapist in interpreting normal range of motion patterns and identify when sport-specific adaptations or clinically significant adaptations are present (Ellenbecker 2004).

Figure 3-6 Assessment of the posterior shoulder performed by measuring isolated glenohumeral internal rotation.
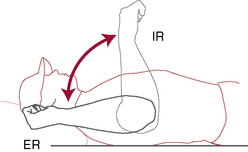
Figure 3-7 Total rotation range of motion concept.
(Redrawn from Ellenbecker TS. Clinical Examination of the Shoulder. Saunders, St. Louis, 2004, p. 54.)
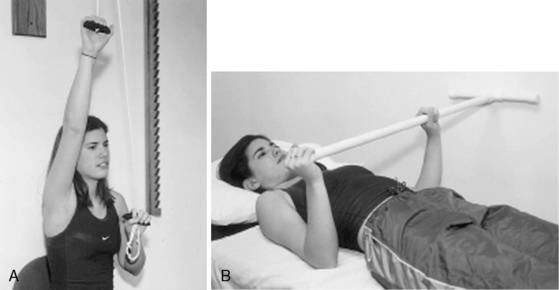
Once active motion can be initiated, the patient is encouraged to work early on pain-free ranges below 90 degrees of elevation. For most patients an early goal is 90 degrees of forward flexion and approximately 45 degrees of external rotation with the arm at the side. For surgical patients, it is the responsibility of the surgeon to obtain at least 90 degrees of stable elevation in the operating room for the therapist to be able to gain this same motion after surgery. At this point in rehabilitation, methods to gain motion include active-assisted range of motion with wands or pulleys, passive joint mobilization, and passive stretching exercises (Figs. 3-8 and 3-9).
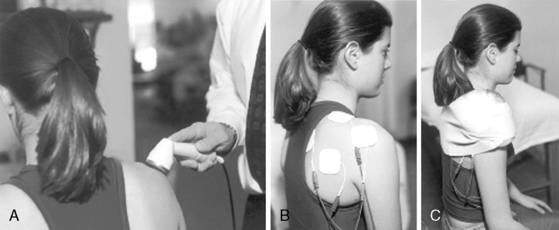
Pain Relief
Both shoulder motion and strength can be inhibited by pain and swelling, with pain being the major deterrent. Pain can be the result of the initial injury or from surgical procedures attempting to repair/replace the injured tissue. Pain relief can be achieved by a variety of modalities including rest, avoidance of painful motions (e.g., immobilization; Fig. 3-10), cryotherapy, ultrasound, galvanic stimulation, and oral or injectable medications (Fig 3-11). Previous literature substantiates that continuous cryotherapy following surgical procedures results in immediate and continued cooling of both subacromial space and glenohumeral joint temperatures (Osbahr et al. 2002) and decreases the severity and frequency of pain, which allows more normal sleep patterns and increases overall postoperative shoulder surgery comfort and satisfaction (Singh et al. 2001, Speer et al. 1996).
Muscle Strengthening
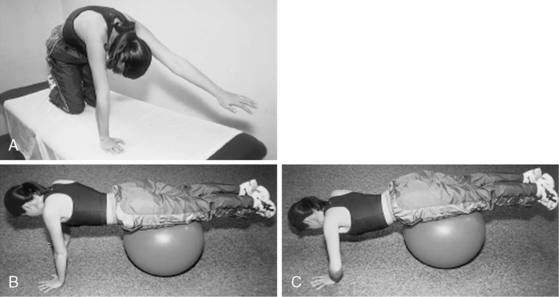
Appropriate timing for initiation of muscle strengthening exercises during shoulder rehabilitation is completely dependent on the diagnosis. A simple uncomplicated impingement syndrome may be able to commence strengthening exercises on day 1, whereas a postoperative rotator cuff repair may require up to 10 weeks before initiation of strengthening of the cuff, allowing the repaired tendon time to heal securely to bone of the greater tuberosity. Strengthening of the muscles around the shoulder can be accomplished through different exercises. Basic safe exercises include isometrics (Fig. 3-12), and closed kinetic chain exercises (Figs. 3-13 and 3-14). The advantage of closed chain exercises is a co-contraction of both the agonist and the antagonist muscle groups that help enhance stability of the glenohumeral joint. This co-contraction closely replicates normal physiologic motor patterns and function to help stabilize the shoulder and limit abnormal and potentially destructive shear forces crossing the glenohumeral joint. A closed chain exercise for the upper extremity is one in which the distal segment is stabilized against a fixed object. During shoulder exercises this stable object may be a wall, door, table, or floor. One example of a closed-kinetic-chain exercise used in an elevated, more functional position is the “clock” exercise in which the hand is stabilized against a wall or table (depending on the amount of elevation allowed) and the hand is rotated to different positions of the clock face (Fig. 3-13). This is done by creating an isometric contraction in the direction of the numbers around the clock face. Alternatively, the therapist can also give manual resistance in the same directions to the patient’s arm as they are stabilizing it by holding on to the wall (Fig. 3-14). These motions are thought to effectively stimulate rotator cuff activity. Initially, the maneuvers are done with the shoulder in less than 90 degrees of abduction or flexion. As healing tissues improve and motion is recovered, strengthening progresses to greater amounts of abduction and forward flexion.
Isometric exercises can also be performed in various ranges of shoulder elevation. It is easiest to do this with the patient in supine. The “balance position” is that of 90 to 100 degrees of forward flexion of the shoulder while supine (Fig. 3-15). This position requires little activation of the deltoid so that the rotator cuff can be worked without provoking a painful shoulder response. In this position a contraction from the deltoid will result in joint compression, helping to enhance joint stability. Rhythmic stabilization or alternating isometric exercises can be performed very comfortably in the supine position and can be done for both rotator cuff and shoulder muscles.

Figure 3-15 The “balance position” is that of 90 to 100 degrees of forward flexion of the shoulder while supine.
Strengthening of scapular stabilizers is important early on in the rehabilitation program. Scapular strengthening can begin in side lying with isometrics or isotonics or closed chain (Fig. 3-16) and progress to open-kinetic-chain exercises (Fig. 3-17).
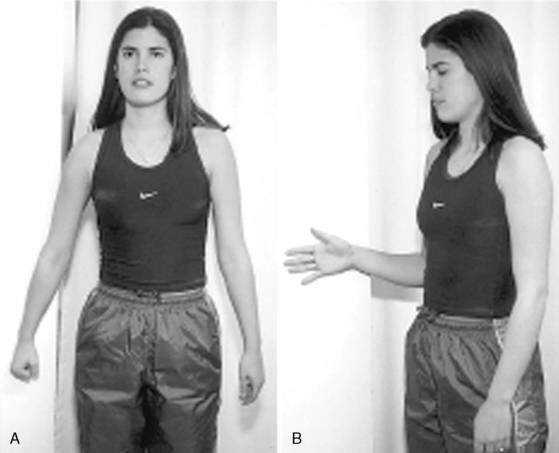
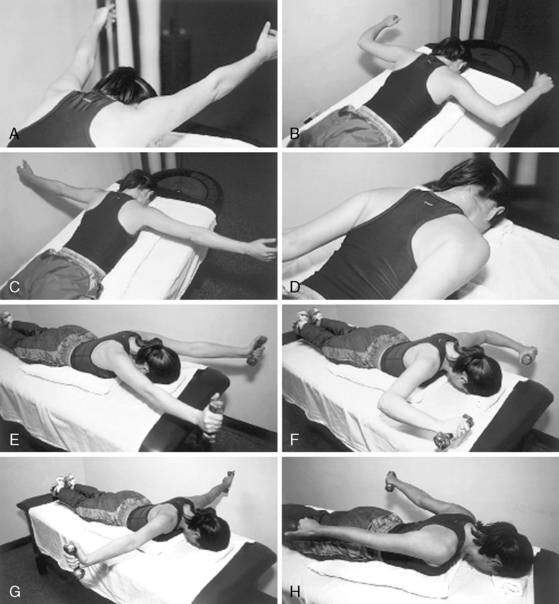
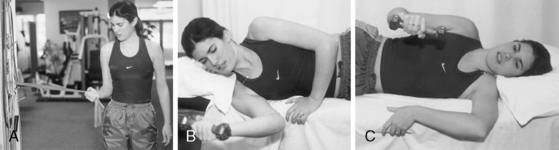
As the patient progresses, more aggressive strengthening can be instituted by moving from isometric and closed-chain exercises to those that are more isotonic and open chain in nature (Fig. 3-18). Open chain exercises are done with the distal end of the extremity no longer stabilized against a fixed object. This results in the potential for increased shear forces across the glenohumeral joint. Shoulder internal and external rotation exercises are done initially standing or seated with the shoulder in the scapular plane. The scapular plane position is recreated with the shoulder between 30 degrees and 60 degrees anterior to the frontal plane of the thorax, or halfway between directly in front (sagittal plane) and directly to the side (frontal plane). The scapular plane is a much more comfortable plane to exercise in because it puts less stress on the joint capsule and orients the shoulder in a position that more closely represents functional movement patterns. Rotational exercises should begin with the arm comfortably at the patient’s side and advance to 90 degrees based on the patient’s injury, level of discomfort, and stage of soft tissue healing. The variation in position positively stresses the dynamic stabilizers by altering the stability of the GH joint from maximum stability with the arm at the side to minimum stability with the arm in 90 degrees of abduction.
For those who participate in either competitive or recreational overhead sporting activities, the most functional of all open-chain exercises are plyometric exercises. Plyometric activities are defined by a stretch-shortening cycle of the muscle tendon unit. This is a component of almost all athletic activities. Initially the muscle is eccentrically stretched and loaded. Following the stretched position the shoulder/arm quickly performs a concentric contraction. These forms of exercises are higher level exercises that should only be included once the patient has developed an adequate strength base and achieved full ROM. Not all patients require plyometric training, and this should be discussed before their incorporation. Plyometric exercises are successful in development of strength and power. Theraband tubing, medicine ball training, or free weights are all acceptable plyometric devices for the shoulder (Fig. 3-19).
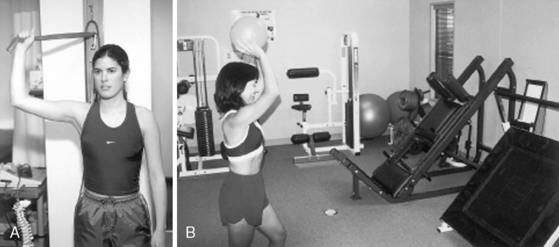
Figure 3-19 Plyometric shoulder strengthening exercises using Theraband tubing (A) and an exercise ball (B).
Rotator Cuff Tendinitis in the Overhead Athlete
Michael J. O’Brien, MD, and Felix H. Savoie III, MD
Anatomy and Biomechanics
The Throwing Cycle
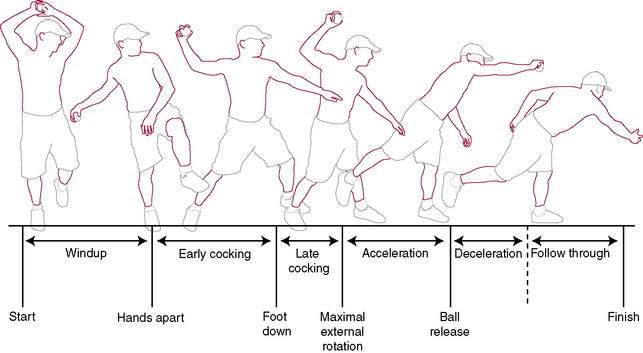
The baseball pitch serves as the biomechanical model for many overhead throwing motions. The throwing cycle is a kinetic chain that derives energy from the lower extremities, transfers it through the pelvis and trunk rotation, and releases that energy through the upper extremity. The arm positions and motions of the throwing cycle serve as a good model for examination of rotator cuff function in overhead athletes. The throwing motion and its biomechanics have been divided into six stages: wind-up, early-cocking, late-cocking, acceleration, deceleration, and follow-through (Fig. 3-20).
Pathogenesis
Injury to the shoulder during the throwing cycle is thought to occur during the late-cocking phase, when the shoulder is in extreme external rotation and horizontal abduction. Abnormal motion of the humeral head relative to the glenoid can injure the superior and posterosuperior labrum and glenoid and the undersurface of the rotator cuff. This phenomenon has been called internal impingement of the shoulder or posterior superior glenoid impingement (Burkhart et al. 2003, Fleising et al. 1995, Jobe 1995, Kelly and Leggin 1999). Several factors have been implicated in the development of internal impingement, including traction on the biceps tendon, laxity of the anterior band of the inferior glenohumeral ligament caused by excessive external rotation, posterior capsular tightness, and scapular dyskinesia.
Grossman et al. (2005) quantified glenohumeral motion following external rotation capsular stretch and subsequent posterior capsular shift to simulate a posterior capsular contracture in the thrower’s shoulder. In maximal external rotation in intact specimens, the humeral head moved in a posterior and inferior direction. A posterior capsular shift was performed to simulate posterior capsular contracture. Following posterior capsular shift, there was a trend toward a more superior position of the humeral head in maximal external rotation. Posterior capsular contracture causes a similar result as the head is pushed anterior–superior into the coracoacromial arch during flexion. Superior translation allows the head to migrate closer to the acromion, and an increase in the force transmitted to the rotator cuff results as the cuff is pressed between the humeral head and the overlying coracoacromial arch. The increased pressure on the cuff can lead to degradation and damage over time.
History and Physical Examination
Physical examination of the overhead athlete requires a global evaluation.
The physical examination of the shoulder and upper extremity should always begin with inspection.
Active and passive range of motion (PROM) should be assessed and compared to the contralateral side. The American Shoulder and Elbow Surgeons have recommended four functional ranges of motion that should be measured (Richards et al. 1994): forward elevation, internal rotation, and external rotation at the side and at 90 degrees of abduction are measured. Loss of the total arc of rotation, specifically with internal rotation, is a common finding in the glenohumeral joint of the injured pitcher (Burkhart et al. 2003). This loss is likely secondary to tightness of the posterior soft tissues, including the posterior rotator cuff and capsule.
Imaging
Radiographs
Magnetic Resonance Imaging
Management
Frequently, rotator cuff tendinitis in the overhead athlete can be successfully treated with a well-structured and carefully implemented nonoperative rehabilitation program (Rehabilitation Protocol 3-1). Rehabilitation follows a multiphase approach with emphasis on controlling inflammation, restoring muscle balance, improving soft tissue flexibility, enhancing proprioception and neuromuscular control, and efficiently returning the athlete to competitive throwing (Wilk et al. 2002). Treatment should focus on restoration of sound mechanics during the throwing cycle, core muscle strengthening of the trunk and lower extremities, and strengthening of periscapular stabilizers.
REHABILITATION PROTOCOL 3-1 Rehabilitation for Rotator Cuff Tendinitis in Overhead Athletes
Phase I
Phase II
Phase III
Phase IV
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree