CHAPTER 2 SHOULDER
A TENDON TESTS
Speed’s test
Clinical context
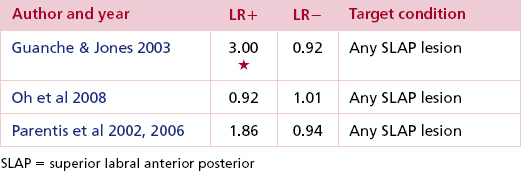
A number of studies (Bennett 1998, Guanche & Jones 2003, Parentis et al 2006) have evaluated the diagnostic accuracy of Speed’s test for biceps, general labral and SLAP lesions against a reference standard of arthroscopy in secondary and tertiary care populations with shoulder pain of mixed causes. None have found Speed’s test particularly useful at ruling biceps tendon pathology or unstable SLAP lesions either in or out (Table 2.1).
Clinical tip
| EXPERT OPINION | COMMENTS |
|---|---|
 | Speed’s test |
| Used regularly if either a biceps or SLAP lesion is suspected. |
Variations
The first written description of Speed’s test was by Crenshaw & Kilgore (1966), who cited as their source a personal communication with the test’s originator. Their description implied, but did not explicitly state, that the test should be performed isotonically against the tester’s resistance. The starting and finishing positions were not specified. Perhaps not surprisingly, interpretations have varied. The description used above mirrors that of Bennett (1998), which is clear and likely to be reproducible.
Yergason’s test
Technique
Positive test
Reproduction of the patient’s pain suggests the presence of a lesion of the long head of biceps or a SLAP lesion. If during the test the biceps tendon is felt to reproduce a ‘clicking’ sensation familiar to the patient, laxity or a tear of the transverse humeral ligament (that contains the tendon in the groove) should be suspected (see Fig. 2.2).
Clinical context
Yergason originally devised this manoeuvre for detecting bicipital tendinitis (Yergason 1931) but it is now apparent that all parts of the tendon complex are loaded and pain may emanate from a genuine tenosynovitis (as the tendon passes through the bicipital groove), tendinopathy or a SLAP lesion (as the long head of biceps attaches to its glenoid-labral origin). It also tests the ability of the transverse humeral ligament to maintain the tendon in the groove. The biceps tendon can be involved in an isolated overuse injury in the younger population although it is most commonly associated with rotator cuff disease in the older patient.
This test has found increasing acceptance in diagnosing SLAP lesions (see labral tests, p. 46). So much so, that studies exploring its diagnostic value have all measured its ability to detect labral injury rather than biceps pathology (Guanche & Jones 2003; Oh et al 2008; Parentis et al 2002, 2006; Table 2.2).
Clinical tip
As an alternative, providing the elbow is fixed adequately between the waist/hips of the examiner and patient, the free hand can palpate over the bicipital groove at the shoulder to detect any abnormal subluxation or ‘snapping’ during the test.
| EXPERT OPINION | COMMENTS |
|---|---|
 | Yergason’s test |
| Used if instability of the biceps tendon in the groove or a SLAP lesion is suspected. |
Related tests
Injury to the biceps insertion on the radial tuberosity can be detected by resisting elbow flexion with the forearm in a pronated position. Normally the biceps would assist brachialis in flexing the elbow and generate some supination of the forearm in the process – a feature known as Heuter’s sign. A biceps insertional tear will inhibit the extent of the flexion/supination contraction, leaving brachialis to generate the bulk of flexion power and resulting in an obvious absence of supination, i.e. a negative Heuter’s sign.
Empty/full can tests
Technique
Action
The shoulder is passively elevated to 90° in the scapular plane and taken into full internal rotation with the forearm in pronation so that the thumb is pointing to the floor (empty can test, Fig. 2.3). The clinician stabilizes the scapula with one hand and places the other on the upper surface of the patient’s forearm. Downward pressure is then applied to the arm while the patient maintains this position. The test is then repeated with the arm externally rotated so that the thumb points upwards (full can test, Fig. 2.4).
Clinical context
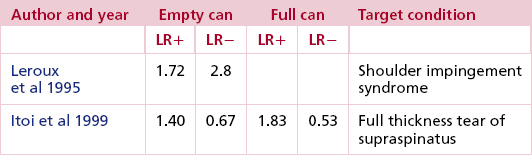
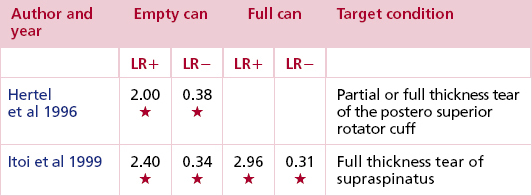
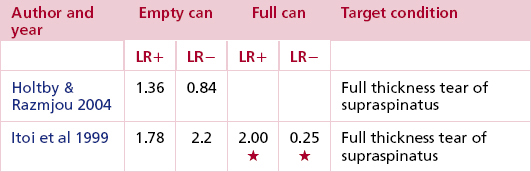
In an EMG study of normal subjects, the empty can and full can tests were shown to preferentially activate supraspinatus with the least co-activation of other muscles. The full can test was originally described in the context of strength assessment, not pain provocation (Kelly et al 1996). Itoi et al (1999) compared the tests’ accuracy in diagnosing full thickness tears of supraspinatus and found them to be broadly equivalent. For strength assessment, however, the full can test is probably preferable, because its position is less likely to cause painful impingement and consequent inhibition (Itoi et al 1999) (Tables 2.3–2.5).
Clinical tip
Weakness in the absence of any pain may result from a C5 palsy, suprascapular neuropathy or Parsonage–Turner syndrome, a viral neuritis affecting the brachial plexus.
| EXPERT OPINION | COMMENTS |
|---|---|
 | Empty/full can test |
| Gives a good indication of a cuff tear or impingement. |
Related tests
In his seminal book on the shoulder, Codman (1934) vaguely described a test which has since become known as Codman’s test or the drop arm test. If positive it is suggestive of a full thickness tear of the rotator cuff with the supraspinatus tendon the most likely culprit. Conventionally, the patient is asked to actively lower the arm, under control, from above 90° in the sagittal plane. He or she will be unable to do so if supraspinatus is completely ruptured; instead, the arm will drop.
External rotation lag sign
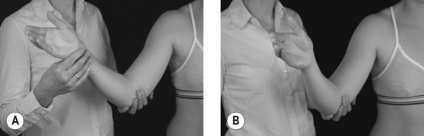
Technique
Patient position
Sitting or standing with the affected arm in a dependent position with the elbow flexed to 90°.
Clinician position
The clinician stands adjacent to the affected side, using one hand to support the patient’s elbow and the other to take hold of the patient’s arm just above the wrist. The shoulder is passively elevated 20° in the scapular plane, then taken to about 5° short of full external rotation (Fig. 2.5A).
Action
Still supporting the patient’s elbow, the tester asks the patient to maintain the external rotation, and then releases the wrist (Fig. 2.5B).
Clinical context
A lag of 5–10° may indicate a complete tear of infraspinatus or supraspinatus. A 10–15° lag is strongly suggestive of a tear of both tendons or may result from neuropathy. This sign is one of several lag signs used to identify and evaluate rotator cuff tears as opposed to painful tendinopathies (Hertel et al 1996).
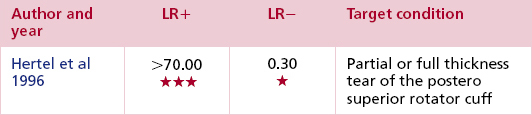
The diagnostic accuracy of the external rotation lag sign (ERLS) was evaluated in 87 patients with either a partial or complete rupture of supraspinatus, infraspinatus, a combination of both or a massive cuff tear (also involving the subscapularis) and a sensitivity of 70% and a specificity of 100% were reported (Hertel et al 1996; Table 2.6).
Clinical tip
According to the test’s originators, a lag as small as 5° may be detectable with practice, especially on the basis of a contralateral comparison. However, they caution against false positive and negative results due to reduced (e.g. capsular limitation) or increased (e.g. supraspinatus rupture) range of movement. Suprascapular palsy would also give a false positive result for cuff rupture.
| EXPERT OPINION | COMMENTS |
|---|---|
 | External rotation lag sign |
| Used regularly to assess the rotator cuff providing the patient has enough range of external rotation to adopt the start position without pain. |
Variations
The drop sign repeats the ERLS in 90° of abduction in the scapular plane (Hertel et al 1996). Again, an inability to maintain the position signifies an infraspinatus tear or neuropathy. This test is unsuitable for patients with stiff shoulders (Table 2.7).
The ‘signe de Clairon’ or Patte’s test is a variation of the drop sign and is intended to isolate lesions of the smaller external rotator of the shoulder, teres minor. The patient’s shoulder is placed in the same start position but the examiner, standing on the affected side and slightly behind the patient, stabilizes the flexed elbow and adds resistance to external rotation by placing the other hand on the posterior aspect of the lower forearm. A positive test, pain and/or weakness, is thought to indicate a tear of teres minor although, because infraspinatus is largely inseparable anatomically and functionally, an isolated tear is improbable.
Lift-off sign
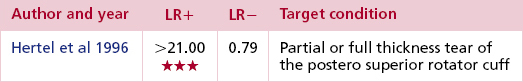
Clinical context
Kelly et al (1996) reported Gerber’s ‘lift-off’ position (Gerber & Krushell 1991) to be optimal for subscapularis contraction and this was supported by another study which demonstrated that the upper and lower subscapularis could produce a 70% maximal voluntary contraction when tested in this position while the other muscles (posterior deltoid, pectoralis major, infraspinatus, latissimus dorsi, teres major and serratus anterior) showed significantly lower levels of activity (P_0.05). The test performed with the hand in the mid-lumbar spine produced one third more EMG activity than with the hand over the sacrum. When resistance was added to the standard test (see Gerber push-off test below), there was an increase in the activity of all muscles, though only a small increase in the activity of the pectoralis major muscle (which was significantly more active during resisted internal rotation with the arm at the front of the body) (Greis et al 1996).
In contrast, however, EMG and nerve block analysis were used to evaluate the activity of the subscapularis tendon in four positions (of increasing degrees of internal rotation), although none of these tested positions were the same as that originally defined by Gerber. EMG activity was identified in latissimus dorsi, posterior deltoid, the rhomboids as well as subscapularis in what was described inaccurately as the conventional test position. With a subscapular nerve block in place the subjects were still able to perform the ‘lift-off’ sign, casting doubt over the validity of the test. The only tested position that could not be maintained with the nerve block in place was in maximum internal rotation, leading the authors to propose the maximum internal rotation lift-off test to be optimum for the detection of subscapularis tears (Stefko et al 1997). However, the original test position (with the hand at the mid-lumbar level) was not evaluated and, when taken alongside the fact that the maximum internal rotation position is unattainable for many patients, the clinician should be wary about discarding the original test in favour of this variant.
The original study that reported the lift-off sign demonstrated high levels of sensitivity and specificity although the authors conceded that the validity of the test is reliant on the existence of full passive internal rotation and that active range is not significantly limited by pain. An inability to ‘lift-off’, increased external rotation range and weakness of internal rotation were all reported to be indicative of a full thickness tear of subscapularis (Gerber & Krushell 1991). In contrast, an independent evaluation of its diagnostic accuracy in a larger population, reported lower levels of sensitivity and specificity (Kim et al 2003b). This highlights a tendency in the literature for originators of diagnostic tests to report higher levels of sensitivity and specificity than independent assessors; this may be due to various factors including differing levels of technical proficiency in applying and interpreting the test.
Clinical tip
A partial tear is denoted by a limited ability to maintain the lifted-off position, such that the arm drops back less than 5° (Gerber et al 1996, Hertel et al 1996).
| EXPERT OPINION | COMMENTS |
|---|---|
 | Lift-off sign |
| Gives a good indication of a subscapularis tear, particularly if there are only subtle signs on examination. However, many patients with impingement and cuff pathology find the degree of internal rotation painful, which limits its usefulness in patients with significant/acute pain or with limited shoulder range. |
Variations
The belly-press test or Napoleon test has the patient seated with the palm of the hand pressing against the abdomen while keeping the shoulder in full internal rotation. The test is positive if this position cannot be maintained and the elbow swings posteriorly as the patient attempts to compensate by pulling the hand against the abdomen (Gerber et al 1996). In a study of 25 patients listed for surgical repair of the subscapularis tendon, the findings of the belly-press test pre-operatively were compared with the findings in theatre (Burkhart & Tehrany 2002). Of nine patients with positive tests, eight had complete tears. Positive tests correlated with full thickness, full-width tears of the tendon while negative tests were recorded in patients whose tears only involved the upper half of the tendon. As a modification, the clinician interposes one hand between the patient’s hand and the abdomen so that the amount of pressure the patient is able to exert can be gauged, although its value is speculative. Some clinicians modify further by bringing the elbow forward into the scapular plane, thereby increasing the degree of internal rotation while ensuring the patient keeps the wrist in a neutral position.
The Gerber push-off test (Kelly et al 1996) may be used if the patient is able to maintain the ‘lift-off’ position. The patient is asked to maintain the lift-off position while the clinician applies an anteriorly directed force against the lower forearm (Fig. 2.7). This supplementary isometric action preferentially activates subscapularis (Kelly et al 1996) and is a pain-provocative manoeuvre.
B IMPINGEMENT TESTS
Neer’s sign
Technique
Clinician position
The clinician stands on the affected side and stabilizes the scapula with one hand and grasps the arm below the elbow with the other hand.
Clinical context
In a cadaveric study, Neer (1972) noted a potential for impingement between the acromion and supraspinatus, infraspinatus and the long head of biceps with the arm in the test position in approximately 10% of specimens. He cautioned that while his sign could signify impingement, there were many other conditions that could also provoke pain during the manoeuvre and that full elevation and external rotation range should be present to eliminate the presence of capsulitis and reduce the possibility of recording false positive findings (Neer 1983, Neer & Welsh 1977). Neer recommended that the sign was re-evaluated after subacromial injection of local anaesthetic and, if the pain was relieved (a positive Neer’s test), a diagnosis of subacromial impingement could be made.
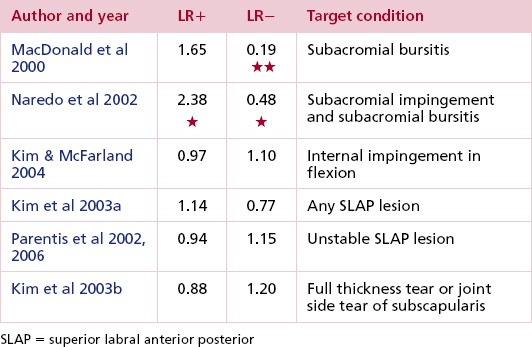
In a much more detailed cadaveric study (Valadie et al 2000), Neer’s manoeuvre was also shown to consistently bring the subacromial soft tissues, including the long head of biceps, into contact with the coraco-acromial arch (subacromial impingement) and the internal aspects of supraspinatus and infraspinatus into contact with the glenoid rim (internal impingement), a finding confirmed in a large arthroscopic study which identified internal impingement in 74% of shoulders that had tested positive to Neer’s sign (Kim & McFarland 2004). According to other cadaveric studies (Flatow et al 1994, Jobe 1997) and an MRI evaluation of normal subjects (Roberts et al 2002), performing Neer’s sign in the scapular plane appears to cause more internal impingement, although clinically no study has demonstrated higher levels of sensitivity or specificity in the diagnosis of subacromial impingement by altering the plane of elevation (Kim & McFarland 2004, Naredo et al 2002, Parentis et al 2002, 2006).
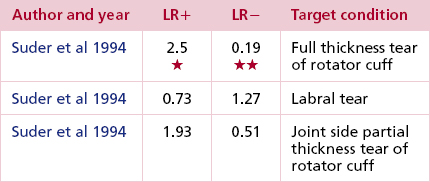
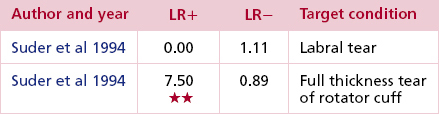
Neer himself regarded his eponymous sign as uninformative unless it was abolished by injection of local anaesthetic under the acromial arch. Several studies have evaluated the diagnostic accuracy of Neer’s sign (Kim & McFarland 2004, MacDonald et al 2000, Parentis et al 2002, 2006) for a range of shoulder pathology, overlooking its origin as an impingement test as well as failing to evaluate Neer’s confirmatory test. The work done by Suder et al (1994), however, allowed head to head comparison of both sign and test in the same sample of patients. For each target condition of interest, performing the test after the sign resulted in decreased sensitivity and increased specificity, however, it was only in relation to full thickness tears that a positive sign and test provided sufficiently strong evidence to rule in the diagnosis with some degree of confidence.
| Types of impingement (Magee 2008) | |
|---|---|
| Primary (outlet) | Intrinsic |
| Mechanical compression of the bursal/superior side of the rotator cuff mainly involving the supraspinatus tendon. Because the impingement occurs anteriorly around the supraspinatus outlet region, primary impingement is sometimes known as anterior or outlet impingement syndrome Neer described three stages of primary impingement characterised by: Stage I reversible oedema and haemorrhage of the rotator cuff often seen in the younger patient. Stage II fibrosis occurring as a result of the ageing and degenerative process, and, Stage III bone spur development tendon rupture | e.g. degeneration of the cuff |
| Extrinsic | |
| e.g. where the shape of the acromion negatively impacts on the ability of the greater tuberosity and cuff tendons to navigate under the coraco-acromial arch without impingement | |
| Secondary (outlet) | |
| Caused by weak or imbalanced muscles leading to instability of the scapulohumeral complex which in turn results in abnormal movement patterns and anterior impingement | |
| Internal (non-outlet) | |
| Results from injury to the undersurface of the rotator cuff or the glenoid labrum caused by impingement of the supraspinatus and infraspinatus tendons between the posterosuperior aspect of the glenoid rim and the humeral head. The impingement occurs posteriorly and is sometimes known as non-outlet impingement | |
Clinical tip
| EXPERT OPINION | COMMENTS |
|---|---|
 | Neer’s sign/test |
| This helps to form part of the total picture but is non-specific. If other tests, including ultrasonography, have been inconclusive, using local anaesthetic as a confirmatory test can be useful. |
Variations
Many clinicians modify Neer’s manoeuvre by maintaining internal rotation at the shoulder throughout elevation (flexion–internal rotation test). Although the intention is to position the insertions of both supraspinatus and infraspinatus so that they are more vulnerable to subacromial compression, an open MRI study of normal subjects showed that this position consistently resulted in internal rather than subacromial impingement (Jobe 1996).
Although speculative, further differential testing can be used to make a distinction between pain predominantly emanating from the cuff or bursa. Given their anatomical intimacy this is challenging, but pain arising from isometric testing of the supraspinatus and infraspinatus may lessen when the tests are repeated under distraction if the bursa is the main culprit due to the decompression effect in the subacromial area. For resisted abduction (supraspinatus) the patient is supine, distraction is applied in a neutral position, counterpressure applied on the opposite hip while resistance to isometric abduction of the shoulder is applied at the elbow (Fig. 2.9). For resisted external rotation (infraspinatus) the same principles are applied; the upper arm is wedged between the patient’s waist and the examiner’s thigh and the elbow flexed to 90°. The examiner then interlocks the elbow with the patient’s to apply the distraction, while the outer hand is placed on the lateral border of the lower forearm to provide resistance (Fig. 2.10).
Hawkins–Kennedy impingement test
Technique
Clinician position
Standing adjacent to the patient on the affected side, one hand is placed under the elbow, the other holds just above the wrist. The elbow is flexed to 90° and the shoulder taken passively into 90° of forward flexion.
Clinical context
MRI analysis shows that the Hawkins–Kennedy impingement test brings the rotator cuff insertions against the acromion (Roberts et al 2002) so the subacromial bursa, overlying the tendons, must also be compressed in this position. A cadaveric study also showed that the bursal side of the cuff is very likely to contact the acromion or coraco-acromial ligament. In two of four specimens the bursal side of the cuff contacted the acromion; in all four the bursal side of the cuff or the long head of biceps contacted the coraco-acromial ligament; and in one of the four, subscapularis was distorted by the coracoid (Valadie et al 2000).
The Hawkins–Kennedy test may also have a role in identifying internal impingement, as it has been shown to cause pinching of the internal aspect of the damaged rotator cuff (particularly subscapularis) against the glenoid labrum (Struhl 2002, Valadie et al 2000).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree