Acute shoulder injuries and chronic shoulder symptoms have become an increasing problem in recent years. Degenerative shoulder symptoms are exceeded only by degenerative back and knee disorders. Causes include sports, leisure activities, and occupational stresses overlaid on age-related degeneration. Decades of repetitive overhead movements in occupational, leisure, or domestic activities can cause stress syndromes. With increasing age, the incidence of degenerative changes of the shoulder approaches 100%.
Occupational shoulder complaints are not a new phenomenon. The galley slaves of ancient times were well acquainted with the effects of asymmetric stress from rowing. The modern physiologic equivalents of these galley slaves are world-class tennis players. Here, asymmetric stress and adaptation result in complex changes in the muscles, tendons, and bones referred to as “tennis shoulder.” While the shoulder complex is crucial to the coordinated movements of most sports, the force, flexibility, and endurance requirements of athletic activity often exceed physiologic limits. Repetitive overhead movements can induce attritional mechanisms with resulting pathologic changes to the rotator cuff. In the throwing athlete, forceful windup, cocking, and acceleration motions can produce anterior instability. Deceleration on follow-through can produce posterior instability. Eccentric loads can cause tenosynovitis. The adolescent athlete is faced with age-specific problems in the form of incomplete epiphyseal fusion, just as the older athlete must contend with degenerative changes to the tendon of the supraspinatus muscle.
1.2 Clinical Examination
Standard Examination
The patient is observed from the front. The sternoclavicular joint, clavicle, acromioclavicular joint, and the pectoralis major and biceps are evaluated. Posterior observation to evaluate for atrophy in the infraspinatus and supraspinatus follows. For the rest of the examination, stand behind the patient. After a preliminary examination of the cervical spine, palpate the sternoclavicular joint, clavicle, acromioclavicular joint, coracoid process, the long tendon of the biceps, and the supraspinatus tendon in internal rotation. Range-of-motion tests are then performed using the neutral-0 method (flexion/extension, abduction/ adduction, external rotation/internal rotation in a neutral position and abduction). The painful arc of motion can be assessed. Horizontal adduction may also reveal pain with cross-body compression. The apprehension test is also performed standing behind the patient, as is evaluation of the sulcus sign. Move to the front of the patient to conduct the Jobe test and to assess the strength and sensation of the upper extremities.
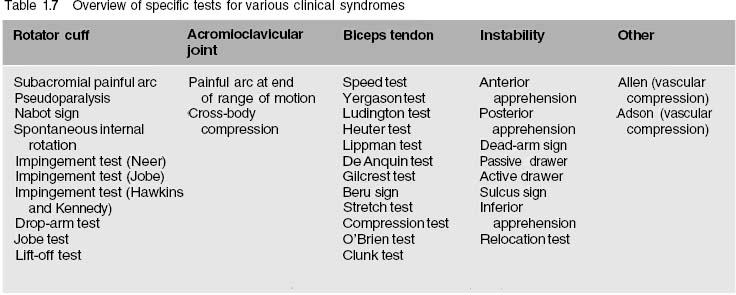
Depending on the working diagnosis, this standard examination is supplemented by various specific tests discussed in the following section.
Patient History
As in any medical encounter, the examination of the shoulder begins with taking the patient’s history. This forms the basis for the working diagnosis. The various disorders of the shoulder can be caused by acute trauma, repetitive microtrauma, age-related degeneration, or systemic disorders. In patients with acute injuries, the manner in which the accident occurred and observation of the cardinal symptoms (redness, warmth, swelling, loss of function, etc.) can provide sufficient information for a diagnosis. Chronic complaints require an extensive history. This requires a good memory on the part of the patient, an extensive review of medical records, and no small amount of detective work on the part of the physician to make the diagnosis and identify the cause.
Many of the systemic disorders that affect the shoulder are hereditary. If a hereditary disorder is suspected, a detailed family history must be explored.
The age of the patient is a critical factor in the overall evaluation of symptoms. Many disorders of the shoulder girdle occur more frequently within certain age-groups. For example, clavicular fractures and torticollis frequently occur in newborns and infants. Congenital deformities such as Sprengel deformity, Klippel–Feil syndrome, or cleidocranial dysostosis are first observed at this age. Septic arthritides or osteomyelitis can be the cause of fevers in infants (Table 1.1). Acute injuries predominate in adolescents and young adults. These include dislocated shoulders, injuries to the acromioclavicular joint, and clavicular fractures. After the age of 30, degenerative symptoms tend to predominate, primarily impingement syndrome, tears in the rotator cuff, and degenerative changes in the acromioclavicular joint. Impingement syndromes can occur in athletes, even at a young age. In this case, primary impingement syndrome must be carefully distinguished from impingement of instability. In the older population, degenerative changes in the rotator cuff and glenohumeral joint predominate.
| Newborn/infant | Adolescent/young adult | Older adult |
| Clavicular fracture | Traumatic instability | Partial tear of the rotator cuff |
| Torticollis | Acromioclavicular-joint separation | Complete tear of the rotator cuff |
| Septic arthritis | Clavicular fracture | Arthritis of the acromioclavicular joint |
| Osteomyelitis | Dislocation of the sternoclavicular joint | Fracture of the proximal humerus |
| Sprengel deformity | Tenosynovitis | Calcific tendinitis |
| Klippel–Feil syndrome | Atraumatic instability | Subacromial bursitis |
| Cleidocranial dysostosis | Subacromial bursitis |
Inquiring about occupational and athletic activity provides important information. Occupations that involve overhead work (such as painting) and sports that make similar demands (such as basketball, baseball, tennis, swimming, and volleyball) often lead to symptoms in the subacromial area. Degenerative changes may occur in the acromioclavicular joint. For possible occupational causes, carefully evaluate information on force, repetition, posture, duration of exposure, contact stress, vibration exposure, and low-temperature exposure. Confirm information provided by the patient with material such as formal position descriptions, workplace videos, or job-site analysis provided by a third party. Making a diagnosis of an occupational injury can have a profound negative response to treatment, as it appears that success rates in worker’s compensation situations is less than in other settings.
With athletes, taking a history requires knowledge of the specific sport. Only in this manner can characteristic patterns of injury for specific sports be identified. Often these patients do not suffer acute trauma, but repetitive microtrauma can occur with hyperextension at maximum abduction and external rotation in “overhead” sports. This can lead to instability of the shoulder. Often these patients will present with symptoms resembling impingement. Instability problems are less prominent in bodybuilders or competitive weight lifters. Be alert for degenerative changes in the acromioclavicular joint and rotator cuff.
| Occupation | Sport |
| Painting | Throwing sports |
| Drywalling | Tennis |
| Plastering | Weight lifting |
| Air-hammer operation | Racquetball |
| Swimming |
With precise knowledge of a particular sport, important information can be obtained by inquiring specifically when pain occurs. A baseball player whose primary symptoms occur during the early cocking phase (abduction and external rotation) may suffer from anterior instability as a result of chronic overloading of the anterior stabilizers of the joint. If complaints occur primarily during the follow-through phase of throwing motion (flexion and internal rotation), then the disorder could involve either posterior instability or tendonopathy. Other related activities exist that can cause symptoms if instability is present. These include reaching high overhead while rebounding in basketball, a running spike in volleyball with the shoulder hyperextended, or a hard stroke in tennis with the arm extended overhead.
Taking a detailed history can also provide important information about degenerative disorders or repetitive microtrauma. For example, a tennis player with supraspinatus tendinitis may complain of sharp pain during a backhand stroke, while a forehand stroke presents no problem at all. The same applies to the serve. A tennis player with supraspinatus tendinitis can have discomfort when the tendon is compressed between the greater tuberosity of the humerus and the acromion in the final phase of an overhead serve when there is maximum internal rotation on the follow-through. This internal rotation is avoided in a forehand serve that can be performed without any pain.
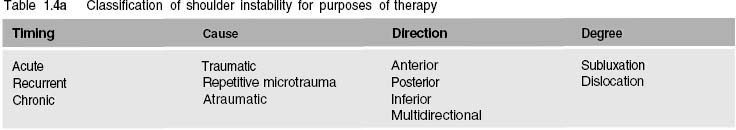
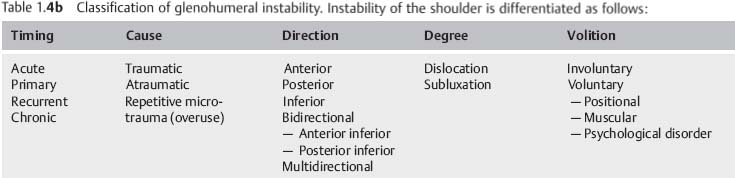
When the history reveals dysfunction following prior trauma, it is important to reconstruct the mechanism of injury as precisely as possible. The magnitude, direction, and point of impact of the forces acting on the joint are important in establishing whether a direct or indirect mechanism of injury was involved. This inquiry yields important diagnostic information about the type and extent of injury. Acute trauma with the arm abducted and externally rotated generally results in an anteroinferior dislocation of the shoulder. A typical example is the quarterback who is sacked by the defensive lineman in the midst of throwing. Internal rotation and adduction often causes posterior dislocation of the shoulder. A fall with the arm extended can cause dislocation if the player fails to tense his or her muscles in anticipation of the fall. A direct blow to the lateral aspect of the shoulder suggests acromioclavicular joint separation. A direct blow to the clavicle or a fall on the extended arm can cause a clavicular fracture. If the patient has a history of shoulder instability, then the question of whether the instability was triggered by acute trauma or a unique motion is important. It is also important to ask if reduction was necessary. Did reduction occur spontaneously, or did the patient position the arm to obtain reduction? Was reduction only possible in an emergency-room setting or only under anesthesia? Was reduction painful? In the case of recurrent instability, documenting the initial event is particularly important. Did trauma precede this dislocation? How old was the patient when the first dislocation occurred? All these questions are crucial for classifying the instability and determining appropriate therapy (Table 1.4a, b)
| Known association with shoulder complaints | Possible association with shoulder complaints | Rare association with shoulder complaints |
| Handball | Windsurfing | Cross-country skiing |
| Volleyball | Rowing | Cycling |
| Tennis | Waterskiing | Riding |
| Basketball | Dancing | Hockey |
| Squash | Ballet | Soccer |
| Swimming | Swimming | Roller skating |
| Butterfly, backstroke, crawl | Breaststroke | Ice skating |
| Badminton | Ice hockey | |
| Weight lifting | Archery | |
| Fencing | ||
| Boxing | ||
| Throwing sports | ||
| Baseball, shot put, javelin, discus, hammer | ||
| Martial arts | ||
| Judo, aikido, karate, teakwondo | ||
| Gymnastics | ||
| Floor exercises, horizontal bar, parallel bars, | ||
| uneven parallel bars, beam |
However, acute trauma is not always the cause of acute symptoms. In patients with previous tendon degeneration, even normal motion can lead to rupture of the supraspinatus tendon. For example, if a 40-year-old tennis player with a 4-year history of shoulder discomfort complains of a sudden stabbing pain during a serve, this would suggest a rotator-cuff tear. On the other hand, sudden pain during a tennis serve in a 20-year-old tennis player is more likely to be a sign of shoulder subluxation (dead-arm syndrome).
In the presence of chronic complaints, the type of pain should be quantified:
– When did the pain first occur?
– How long does the pain usually last?
– What type of pain is it, diffuse or stabbing?
– Where is the pain localized?
– Into which parts of the body does the pain radiate?
– Are there specific movements that provoke the pain?
– Does the pain occur before, during, or after exercise?
– Does the pain occur at night?
– Is the night pain intense enough to wake the patient?
The type of pain can suggest probable diagnoses to the experienced examiner. For example, the diffuse deep pain that occurs in disorders of the rotator cuff can be clearly differentiated by the patient’s history from the sharp localized pain of acute calcific bursitis. Even in degenerative shoulder disorders, the motion triggering the pain is a crucial piece of diagnostic information. Supraspinatus disorders often produce symptoms from 40° to 120° of abduction; a degenerative acromioclavicular joint will cause problems at the end of range of motion in abduction and when grasping the contralateral shoulder. Frequently, pain will manifest itself in two phases. For example, adhesive capsulitis can be divided into an initial painful phase (freezing phase), in which mobility still exists, and a second painless phase (frozen phase), in which the joint is immobile. The acute pain of a degenerative rotator-cuff tear is almost always preceded by an extended episode of diffuse shoulder pain, pain at night, and pain with the arms extended overhead.
Sometimes a patient will complain of weakness; he or she is no longer able to make certain movements or may notice changes in muscle contour. Atrophy of the supraspinatus or infraspinatus musculature is noticed far more than the conspicuous and typical changes in the contour of the upper arm after a tear in the long biceps tendon. The patient’s spouse, parents, coach, or tennis partner are more likely to notice compensatory movements than the patient.
Aside from the specific questions focusing primarily on the shoulder girdle, inquire about systematic diseases and other disease processes (Table 1.5). For example, angina often radiates into the shoulder and arm; the radiating pain does not always occur on the left side. Depending on variations in myocardial vascular anatomy, pain can radiate into the right upper extremity. Gallbladder and liver disorders can also produce pain in the right shoulder. The patient’s neurologic and endocrine status should be explored. Both rheumatoid arthritis and hyperuricemia manifest themselves in the shoulder. Patients with diabetes mellitus experience an above-average incidence of shoulder complaints.
Even in young patients the possibility of a neoplastic process cannot be ignored, particularly when the history is inconsistent with known primary shoulder disorders. One of the most frequent neoplastic causes for shoulder pain is a Pancoast tumor with a typical Horner syndrome. Other causes include primary osteogenic tumors in younger patients, and metastatic disease in older patients. A history of cold or numb fingers suggests a compressive neuropathy or vascular compromise.
To complete the history, document previous interventions. Inquire specifically about the number, type, and site of previous injections. It is also essential to elicit a history of other medications. Any indication of treatment with anabolic steroids is important, particularly in athletes, because these drugs significantly decrease the ability of muscle-tendon units to respond to exertion. Tears can occur in these weakened structures.
As in any physical examination, a systemic approach is the key to clinical examination of the shoulder. Such an approach can help to prevent important findings from being overlooked and can reduce the risk of inadequate documentation.
Every clinical examination consists of three parts: observation, palpation, and tests.
Observation
Observing the patient provides an initial insight into the diagnosis. This begins the moment the patient’s name is called in the waiting room. Note how the patient arises from the chair, his/her gait, and the motion of the contralateral upper extremity. Does the patient undress smoothly and symmetrically? A patient with a frozen shoulder will avoid any shoulder rotation and movements above horizontal when undressing. If acute calcific bursitis is present, the intense pain will cause the patient to anxiously hold the affected arm fixed to the side; often the patient will hold the affected arm with the other hand. Patients with a tear in the rotator cuff will often ask for help when undressing because they lack the strength to abduct the arm. An arm adducted and held in internal rotation (in the “porter’s tip” position) suggests Erb palsy (Fig. 1.1).
| Angina | Rheumatoid arthritis | Primary neoplasms |
| Myocardial infarcts | Hyperuricemia | Secondary neoplasms |
| Biliary disease | Hematologic disease (hemophilia, sickle cell) | Pancoast tumor |
| Liver diseases | Cervical spine syndrome | Neurovascular entrapment |
| Irritation of the diaphragm | Epicondylitis |
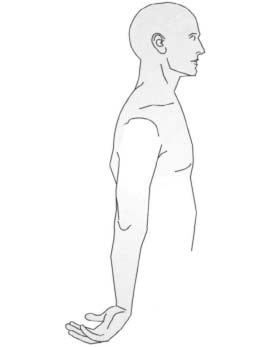
Fig. 1.1 Typical appearance of Erb palsy with the arm adducted and in internal rotation.
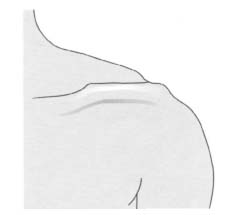
Fig. 1.2 Separation of the acromioclavicular joint showing the superiorly protruding lateral clavicle.
Always uncover both shoulders for the examination. Examination gowns that leave the shoulder girdle exposed may be helpful with female patients. Inspection begins anteriorly and proceeds posteriorly. Note any blisters, hematomas, scrapes, or other pathologic skin changes. Asymmetry, especially muscular atrophy, is best revealed by comparing one side with the other. A lateral tangential view is better for comparing the sides. This view will reveal minor differences between the sides in the sternoclavicular joints. These may be caused by subluxation or dislocation, or by degenerative changes in the joint. When observing and comparing the acromioclavicular joint from both sides, be alert to swelling or step-off resulting from acromioclavicular joint separation. The superiorly protruding clavicle with a “piano key” phenomenon is a diagnosis from observation (Fig. 1.2) like a tear of the long head of the biceps tendon with distal migration of the muscular belly (Fig. 1.3). The same applies to many congenital disorders such as Sprengel deformity (Fig. 1.4), Klippel–Feil syndrome, congenital torticollis, or a clavicular fracture frequently occurring in newborns and infants.
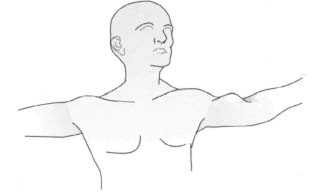
Fig. 1.3 Proximal tear of the long head of the biceps showing distal migration of the muscular belly.
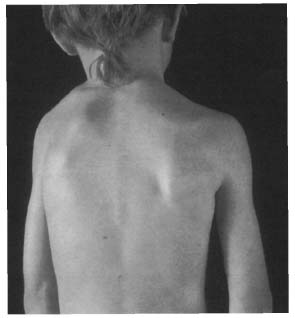
Fig. 1.4 Sprengel deformity showing the superiorly protruding scapula.
Isolated atrophy of the supraspinatus muscle suggests a tear in this tendon. Atrophy of the supraspinatus and infraspinatus muscles can be due to a tear in the rotator cuff or a scapular notch syndrome. Isolated atrophy of the infraspinatus muscle can be caused by entrapment of the infraspinatus branch of the suprascapular nerve.
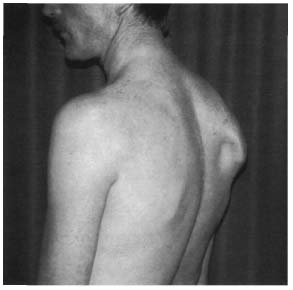
Fig. 1.5 Winged scapula, a sequela of a long thoracic nerve injury.
If there is one-sided atrophy of the trapezius muscle, possibly in conjunction with scarring after lymph-node dissection, this may imply a lesion of the accessory nerve.
Is the patient a muscular athletic type or an asthenic type? Several injuries and disorders can be detected by observation. An interrupted shoulder contour with the arm slightly abducted and in slight internal rotation is a sign of anterior dislocation. This contrasts with posterior dislocation, in which the arm is more frequently held in internal rotation and adduction.
The drooping dominant shoulder in a tennis player is a frequently seen posture, as is an internally rotated posture with hypertrophy of the pectoralis muscle. The drooping shoulder can result in a secondary thoracic outlet syndrome and secondary impingement syndrome. Scoliotic changes in the spine can also develop. An obvious hematoma in the middle third of the clavicle is a sure sign of a clavicular fracture. Conspicuous protrusion of the scapula (winged scapula) is often the result of paralysis of the muscles by which it is fixed (serratus anterior and trapezius; Fig. 1.5).
| • Tear of the long head of the biceps |
| • Chronic tear of the rotator cuff |
| • Acute anterior shoulder dislocation |
| • Separation of the acromioclavicular joint |
| • Erb palsy |
| • Winged scapula |
| • Sprengel deformity |
| • Torticollis |
Preliminary Examination of the Cervical Spine and Arm
Every examination of the shoulder girdle also includes an examination of the cervical spine (see p. 289). Often, the cause of shoulder symptoms may be found in the cervical spine and vice versa. The examination includes evaluating mobility in flexion and extension, right and left lateral bending, and right and left rotation in neutral head position and with the head flexed and extended. Next, palpate the bony structures, such as the transverse and spinous processes. Often, muscle tension in the paravertebral musculature and the trapezius will cause pain in the shoulder and the back of the neck. The pain is often localized in the descending part of the trapezius muscle. Finally, seek enlarged lymph nodes in the shoulder and neck area.
Look for tenderness to palpation about the elbow that may include medial or lateral epicondylitis. Pain in typical sensory nerve distribution may provide clues about compression neuropathies (cubital tunnel syndrome, carpal tunnel syndrome, or radial tunnel syndrome).
Palpation
The next step involves systematic palpation of the shoulder girdle. This is performed with the patient sitting or standing.
Sternoclavicular joint. Stand behind the patient and begin by examining the Sternoclavicular joint. Grasp the clavicle between the thumb and forefinger and move it back and forth to evaluate instability. Tenderness to palpation without instability is a sign of joint irritation. Move laterally along the clavicle from the Sternoclavicular joint to the acromioclavicular joint. Any irregularities from an old clavicular fracture will be palpable.
Acromioclavicular joint. The joint space is easily palpable when approached from the medial aspect of the clavicle. Particularly in athletes, whose sport involves overhead movements, and in weight lifters or body builders, the joint will often be tender to palpation, indicating irritation of the joint or the onset of degenerative changes. Instability or a loose acromioclavicular joint can be detected by grasping the clavicle between the thumb and forefinger and moving it back and forth. If the lateral end of the clavicle protrudes as the result of acromioclavicular joint separation, it can be reduced by applying vertical pressure. When the pressure is released, it will spring back into the original position (“piano key” phenomenon).
Coracoid process. Next move the finger approximately one to two finger breadths medially and interiorly to palpate the coracoid process. If the short head of the biceps or the coracobrachialis is overloaded, the area will be tender to palpation. In rare cases of coracoid impingement there may be local symptoms at this bony prominence.
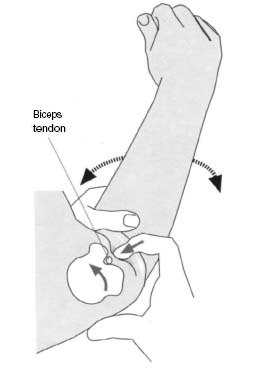
Bicipital groove. The proximal part of the long tendon of the biceps lies in the subacromial space and courses through the narrow bicipital groove. This groove can be palpated deep in the anterior deltoid region. With the patient’s arm flexed at the elbow, passively rotating the arm internally and externally presents the lesser tuberosity, bicipital groove, and greater tuberosity in a more exposed position (Fig. 1.6). If pathology is present, this examination will cause the patient discomfort. If the tendon has a tendency to sublux or dislocate, this test can be used to trigger instability for diagnostic purposes.
Subscapularis tendon. Irritation of the subscapularis tendon in athletes is often the result of overuse in throwing sports. With the arm in external rotation, the tendinous insertion can be palpated near the lesser tuberosity.
Anterior joint capsule. With the arm in external rotation, the anterior joint capsule and labrum complex can be palpated between the coracoid process and the lesser tuberosity. Localized pain in this area due to irritation and lesions of the anterior passive stabilizers, is a sign of anterior instability.

Fig. 1.7 The supraspinatus tendon and the subacromial bursa are palpated with the arm in extension.
Pectoralis major. The tendinous insertion of the pectoralis major is located distal to the lesser tuberosity. Changes in this muscle will often be found in weight lifters. If the history reveals use of anabolic steroids, a steroid-induced pectoralis tear can occur.
Subacromial space. With the shoulder in a neutral position, neither the subacromial bursa nor the supraspinatus tendon are accessible for palpation. Passively extending the shoulder rotates the structures underneath the acromion outward, allowing palpation of the anterior part of the supraspinatus tendon (Fig. 1.7). The parts located further posteriorly are exposed by flexing the arm and palpating immediately behind the posterior margin of the acromion.
Infraspinatus tendon. The infraspinatus tendon in the posterior and lateral portion of the humeral head is accessible with the shoulder in a neutral position. Degenerative changes or overuse injuries are less frequent than in the supraspinatus tendon. Pathologic findings, however, may be present, particularly in athletes with hypermobile or unstable joints as a result of repetitive eccentric stress from the external rotators.
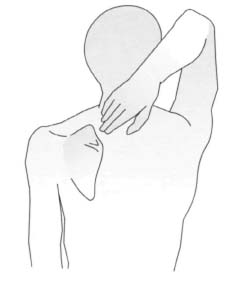
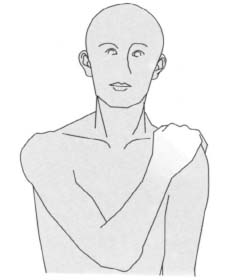
Fig. 1.9 To test internal rotation and adduction, the patient touches the anterior aspect of the contralateral shoulder.
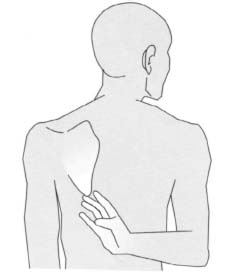
Fig. 1.10 To test internal rotation and adduction, the patient touches the inferior angle of the contralateral scapula.
Systematic and orderly palpation paves the way for further investigation. Despite the important information that can be acquired by physical examination, it may not be sufficient for positive differentiation of bursal-sided, intratendinous, or inferior tears in the rotator cuff. Since this differentiation is crucial in determining treatment, a tentative diagnosis should be confirmed by additional studies.
Assessing Range of Motion
Active range of motion. Several tests utilizing complex motions are suitable for initial evaluation of the patient’s active range of motion. These complex motions themselves comprise several separate component motions. One such test is the Apley “scratch” test. To test abduction and external rotation, ask the patient to reach behind his or her head and touch the superior medial angle of the contralateral scapula (Fig. 1.8) Internal rotation and adduction are tested by having the patient grasp the contralateral acromion (Fig. 1.9). Internal rotation and adduction can also be demonstrated by instructing the patient to touch the inferior angle of the contralateral scapula behind his or her back (Fig. 1.10). To test full bilateral abduction, instruct the patient to abduct both arms with the elbows extended and the palms in supination. The patient should be able to touch both hands together in the midline above his or her head (Fig. 1.11). The advantage of these tests is that they quickly demonstrate the patient’s range of motion for both sides simultaneously. Symmetry of motion and even slight limitations on the affected side are easily detected. In the range-of-motion examination, the patient first demonstrates the active range-of-motion of the unaffected side. Then he or she performs the same motions with the affected extremity.
Passive range of motion. These tests are best performed standing behind the patient. The patient may sit or stand. Holding the patient’s arm above the flexed elbow, place the other hand on the shoulder. The hand on the upper arm guides the patient’s arm through the arc of motion as the hand on the shoulder monitors the movements of the scapula and the humeral head. This permits detection of spasm. If motion is limited due to pain, the pendulum test can be used to document passive range of motion while eliminating the need to use rotator cuff muscles and avoiding stress on the subacromial space. To perform this test, instruct the patient to bend forward and allow the arms to hang down loosely from the body.
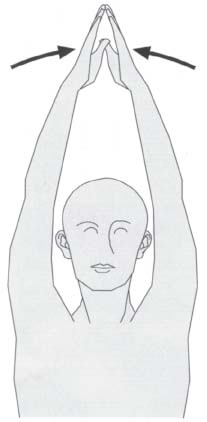
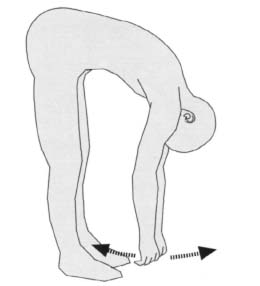
Fig. 1.12 The pendulum test for passive forward motion of the shoulder relieves tension on the subacromial space.

Fig. 1.13 To evaluate laxity in the joint, stabilize the scapula with one hand; with the other hand grasp the humeral head between the thumb and fingers and apply anterior and posterior forces.
This test can be useful to document inconsistencies between reported symptoms and physical examination findings (Fig. 1.12).
Limited range of motion after soft-tissue injuries may present as a frozen shoulder syndrome (adhesive capsulitis). Immobilization of the joint in adduction for several weeks can result in shortening of the adductors, which is identifiable by limited abduction and external rotation. Scars in the axilla can contribute to limited motion, as can radiation therapy. Palpable crepitus with audible snapping and grating, particularly during rotation, may have several causes. Crepitus during passive motion is frequently a sign of changes in the subacromial space. These changes may include thickening and irregularities in the subacromial bursa and the rotator cuff, or changes in the greater tuberosity. Crepitus during active motion is suggestive of instability and may indicate a labral lesion. Palpable snapping, particularly with horizontal adduction and abduction, is encountered with acromioclavicular joint pathology. Crepitus with external or internal rotation in abduction may point to instability of the long head of the biceps.
Normal and abnormal range of motion of the joint must be documented. Abnormal motion may be due to labral or capsular pathology or to weakness in the muscles used to actively stabilize the shoulder. Grasp the humeral head between the thumb and fingers and translate it anteriorly and posteriorly with the shoulder muscles relaxed (Fig. 1.13). This will demonstrate laxity in the joint. Excess laxity may be a part of shoulder instability.
Reduced horizontal adduction is a sign of shortening of the posterior joint capsule (Fig. 1.14).
The active and passive ranges of motion are measured and documented using the neutral-0 method. The following ranges of motion are regarded by some physicians as normal:
– Adduction and abduction: 75°-0°-180°
– Extension and flexion: 60°-0°-180°
– Horizontal extension and flexion: 45°-0°-135°
– Internal and external rotation in adduction: 80°-0°-65°
– Internal and external rotation at 90° adduction: 70°-0°-90°
These values are not always standardized. Note that any abduction past 90° indicates scapulothoracic, rather than glenohumeral, motion.
Although the neutral-0 method is used for all measurements of abduction and adduction, flexion and extension, and internal rotation, the extent of internal rotation is also frequently documented as the part of the body that the patient can reach with the thumb (for example, the greater trochanter, sacroiliac joint, lumbar spinous process, or thoracic spinous process). Both the active and passive ranges of motion are documented. Concentric limitation of motion is a sign of adhesive capsulitis. If external rotation, in particular, is limited, then the differential diagnosis must include chronic posterior dislocation or severe osteoarthritis of the shoulder. Concentric limitations of motion with relatively good external rotation while supine is suggestive of a chronic tear in the rotator cuff.
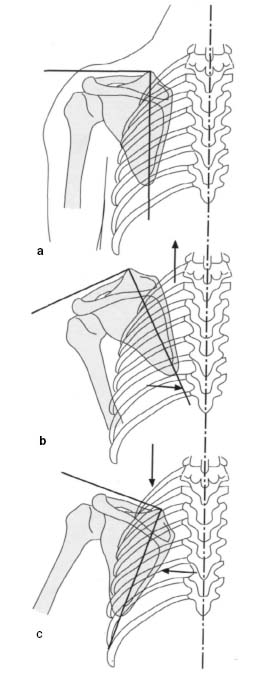
Scapulohumeral rhythm. Irregularities in the scapulohumeral rhythm are best observed from behind the patient. A frozen shoulder, degenerative glenohumeral arthritis, or rheumatoid arthritis of the shoulder will not permit uniform motion. In these conditions, the motion will be segmented and irregular; abduction of more than 90° is rarely possible. Abduction is achieved by scapulothoracic motion rather than by glenohumeral motion. A complete tear of the rotator cuff leads to an even more severe limitation; generally only a few degrees of abduction can be achieved. Again, most abduction will occur as a result of the scapulothoracic motion. With smaller tears, limited abduction will not be so severe; complete physiologic abduction can occasionally be achieved, albeit painfully. Minimally limited abduction may be seen with longitudinal tears. Any weakness detected in abduction is an indication for further diagnostic studies.
Scapula slide test. Physiologic coordinated motion between the scapula and the arm follows certain regular patterns. Abduction of the arm produces a regular lateral sliding motion of the scapula. Observe whether the coordinated motion of the scapula is symmetric. More than 1 cm of asymmetry is regarded as pathologic. For purposes of objective measurement, the distance between the inferior angle of the scapula and the spinous process of the seventh thoracic vertebra is used.
Nerve injuries can produce uncoordinated scapulothoracic motion. Coordinated motion requires stabilizing the scapula on the chest wall. If the stabilizing muscles are weakened or paralyzed, uncoordinated motion results. The main stabilizing muscles are the trapezius and serratus anterior. With neurologic injuries, a winged scapula can be present.
Paralysis of the serratus anterior is encountered most frequently. If this muscle is completely denervated, the diagnosis is made by inspection. Muscular imbalance causes the scapula to protrude, and the inferior angle migrates medially. Maximum scapular winging is demonstrated when the patient elevates his or her arms and presses against a wall (Figs. 1.15a–c). This test will clearly demonstrate slight weakness that will not cause noticeable changes at rest. Paralysis of the trapezius causes an identifiable change in the position of the scapula while the scapula is pulled inferiorly, and the inferior angle migrates laterally and inferiorly from the mid-line.
A lesion of the long thoracic nerve will cause winged scapula similar to a trapezius lesion and is seen in the setting of shoulder complaints that follow a lymph node biopsy. In such situations, the posterior triangle of the neck should be carefully inspected.
A compressive neuropathy of the suprascapular nerve will produce atrophy of the supraspinatus and infraspinatus muscles. If the syndrome involves only the infraspinatus branch, then only that muscle will be affected.
Dislocation of the shoulder can result in damage to the axillary nerve, producing paresis of the deltoid and an area of sensory deficit on the lateral aspect of the shoulder.
Paralysis of the deltoid muscle severely limits abduction. The first 45° of motion is largely unchanged; motion beyond this point can only be achieved with difficulty and requires rotation of the scapula and the use of accessory muscles, specifically the descending part of the trapezius, the serratus anterior, levator scapulae, supraspinatus, and infraspinatus.
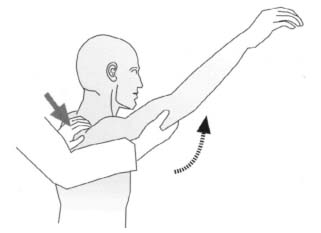
Fig. 1.16 Local anesthesia test for differentiating subacromial pain syndromes (Neer impingement test).
Specific Tests (see Table 1.7)
Painful arc. This is a painful segment of passive or active motion. It should be described in flexion, abduction, or external rotation. It is generally accepted to demonstrate subacromial pathology.
Acromioclavicular compression test (cross-body compression). With the patient’s shoulder flexed 90°, maximum internal rotation, and the elbow flexed 90°, press against the patient’s olecranon from lateral to medial. Pain projected into the acromioclavicular joint is a sign of involvement of this joint.
Neer impingement test. Stand behind the patient, immobilizing the scapula with one hand and briskly flexing the patient’s arm with the other (Fig. 1.16). This will cause the greater tuberosity to decrease the volume of the subacromial space. Pain and weakness may indicate an impingement syndrome. To distinguish between rotator cuff pathology and impingement of instability, repeat the test after infiltrating the subacromial space with local anesthetic. If painless weakness persists after infiltration, consider the possibility of a rotator cuff tear.
Differential anesthetic injection in the shoulder examination. Occasionally it is difficult to differentiate between pain due to degenerative changes in the acromioclavicular joint and subacromial impingement on the basis of the history and physical examination. If there is coexisting radiographic evidence of acromioclavicular and subacromial degenerative changes, the diagnostic dilemma is even greater.
In settings such as this, an extension of the Neer impingement test (using local anesthetic injection to isolate the pain generator) is helpful. These techniques are most useful when the possibility of a rotator cuff tear has been eliminated by history, physical examination, or imaging studies.
After obtaining informed consent, prepare and drape the appropriate shoulder. Verify that the patient is not allergic to the anesthetic you propose to use. It may be helpful to have the patient supine in case of a post-injection vasovagal event.
Palpate the acromioclavicular joint. Using a small gauge needle, inject this joint from an anterior or superior approach with a small amount (2–3 mL) of local anesthetic. Injection will be difficult and may require significant force on the plunger of the syringe. Take care not to inject the subacromial space at this point. Allow the anesthetic to take effect and repeat the physical examination, noting any changes in active range of motion and the degree of pain relief. If the needle placement was accurate and only the acromioclavicular joint was infiltrated, changes in motion and pain can be attributed to the acromioclavicular joint. Marked pain relief after isolated acromioclavicular joint injection is predictive of pain relief after acromioclavicular joint decompression.
If acromioclavicular joint injection provides neither pain relief nor a change in active range of motion, or only partial pain relief and minimal change in range of motion, proceed to subacromial injection at the same sitting. At this point the subacromial injection is performed as in the Neer impingement test.
Again, prepare and drape the appropriate shoulder. From an anterior or lateral approach, palpate the edge of the acromion and the subacromial space. Using a small-gauge needle of sufficient length (1.5 or 2 in), advance the tip into the subacromial space. If the needle tip clears the tip of the acromion, and the barrel of the syringe is perpendicular to the floor, the needle tip is almost certainly in the subacromial space. Make sure that the needle tip is not in the rotator cuff by instructing the patient to gently internally and externally rotate the shoulder. If the needle tip is in the subacromial space, the barrel of the syringe should not move significantly with internal or external rotation. Inject approximately 10 mL of local anesthetic. The injection should require little effort. Wait for the anesthetic to take effect, then re-examine the shoulder. Note any change in active range of motion and pain relief. Significant pain relief and increased motion is predictive of a good response to subacromial decompression.
A partial response to acromioclavicular joint injection with improvement after subacromial joint injection suggests that both areas are pain generators and therefore must be addressed when surgery is performed. If there is residual pain and restricted motion after injection of both the acromioclavicular and subacromial spaces, this should arouse suspicion of glenohumeral joint pathology.
The glenohumeral joint may be injected from an anterior or posterior approach. If the patient is supine, the anterior approach is easier. Prepare and drape the appropriate shoulder. Palpate the coracoid process. The glenohumeral joint is lateral and inferior to the coracoid, approximately two finger-breadths lateral and one finger-breadth inferior. Use a small-gauge needle of sufficient length; sometimes a short spinal needle is useful. Advance the needle, and if bony resistance is encountered ensure you are not on the humeral head or the glenoid. Inject 10 mL. The injection should require little force. Again, re-examine the shoulder noting any changes in pain and range of motion. If there is residual pain after acromioclavicular joint, subacromial space, and glenohumeral joint injection, consider a referred-pain syndrome.
Vasovagal events can occur after injection. Be prepared to allow the patient to lie down for a few minutes.
Jobe impingement test. Jobe introduced a modification of the impingement test in which the arm is rotated internally in abduction. This is more likely to compress the posterior parts of the supraspinatus tendon in the subacromial space (Fig. 1.17).
Hawkins and Kennedy impingement test. The Hawkins and Kennedy impingement test represents a further modification. Here, 90° of shoulder flexion is coupled with simultaneous forced internal rotation (Fig. 1.18). A positive test suggests the presence of a subcoracoid impingement syndrome.
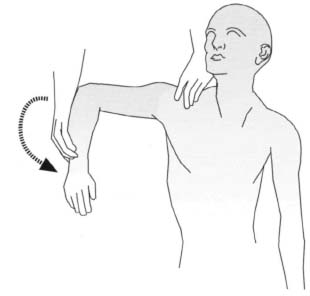
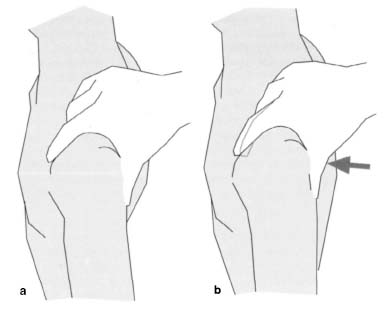
Drop-arm test. This test can be used to diagnose larger tears in the rotator cuff. First instruct the patient to fully abduct the arm. The patient may be able to do this using compensatory motions. However, when the arm is lowered from about 90° abduction, any tear that interrupts the continuity of the tendons will make it impossible to actively hold the arm, which will drop to the side. Occasionally the patient can maintain 90° abduction with great effort, but a mere light tap on the forearm will be enough to cause the arm to drop. If active abduction is not possible, passively abduct the arm to 90°. When the supporting hand is removed, the patient will be unable to maintain this position (Figs. 1.19a, b).
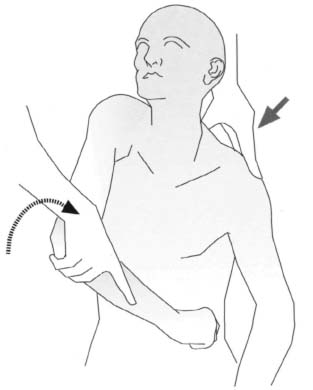
Fig. 1.18 Hawkins and Kennedy impingement test with horizontal flexion and internal rotation suggests the presence of a subcoracoid compression syndrome.
Figs. 1.19a, b The drop-arm test indicates a lesion in the supraspinatus tendon.
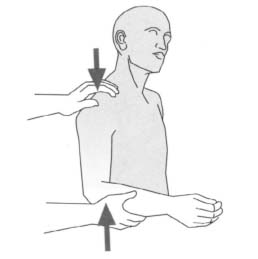
Fig. 1.20 Nabot sign with pain in the subacromial space on compression and rotation.
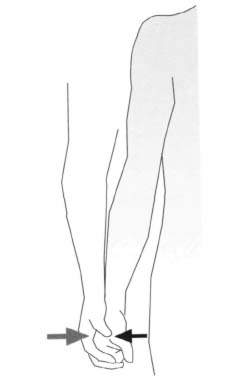
Fig. 1.21 Evaluating the abduction initiation role of the supraspinatus.
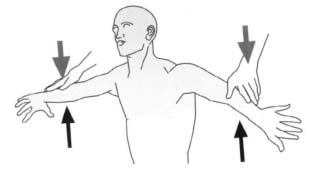
Fig. 1.22 Jobe test for the holding function of the supraspinatus tendon.
Pseudoparalysis. In the presence of pseudoparalysis, the patient will be unable to raise the affected arm. Occasionally, the patient will have learned to abduct the arm using compensatory or swinging motions. This sign suggests the presence of damage to the rotator cuff.
Nabot sign. Press the arm against the acromion along the longitudinal axis of the humerus while rotating it. Crepitus will often be discernible in the presence of rotator cuff pathology (Fig. 1.20).
Active abduction while relieving stress on the subacromial space. Pain during abduction from neutral can be caused by irritation of the supraspinatus tendon or by subacromial bursitis. To differentiate between the two, the attempt to decompress the subacromial space by applying traction along the longitudinal axis of the humerus with the arm at the patient’s side. This relieves tension on the bursa. If pain persists when the patient now attempts active abduction, this suggests supraspinatus pathology. If abduction is now significantly less painful, this suggests that the bursa is the main cause.
Clinical Signs and Specific Tests for Differentiating Pathology of the Rotator Cuff
Provocative test (isometric rotator tests). If pseudoparalysis is present, further evaluation is needed to precisely determine which component of the rotator cuff is involved. Provocative tests can be very helpful. These evaluate external and internal rotation against resistance with the shoulder in various positions. Weakness is usually attributable to a functional deficit, whereas pain with normal strength is usually attributable to tendinitis or bursitis. Selective testing can evaluate various components of the rotator cuff.
• Supraspinatus
Zero-degree abduction test. Abduction of the arm is initiated by the supraspinatus and deltoid muscles. The 0° abduction test is used to evaluate the abduction initiation role of the supraspinatus. The patient attempts to abduct the hanging arm against resistance (Fig. 1.21).
Jobe test. The 90° supraspinatus test evaluates the holding function of the supraspinatus muscle. In this test, described in the literature as the Jobe test, the patient holds the arms in 90° abduction with the elbows extended. The arms are flexed 30° horizontally in relation to the scapular plane and internally rotated (with the thumbs pointing to the floor). The patient attempts to open the arms further, against resistance (Fig. 1.22). The anterior portions of the rotator cuff are tested with the upper arms in the same position but in external rotation.
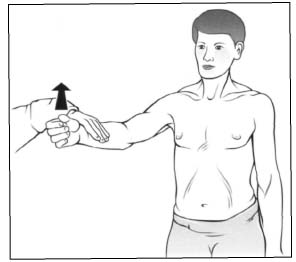
Fig. 1.24 Spontaneous internal rotation is a sign of a tear in the infraspinatus and supraspinatus tendon.
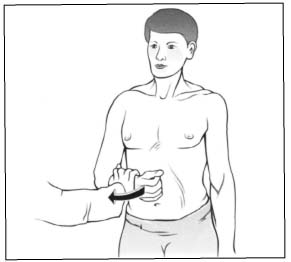
Fig. 1.25 Infraspinatus test. Optimal manual muscle-testing position for the isolation of the infraspinatus muscle: 0° of scapular elevation and 45° of internal rotation.
Full-can test. This test can also be used to evaluate the supraspinatus muscle in isolation. The arm is abducted 90° in the scapular plane and externally rotated 45°. Attempt to press the arm down (“full-can” position) against the patient’s active resistance (Fig. 1.23).
• Supraspinatus and infraspinatus muscles
Spontaneous internal rotation. The patient stands shirtless or appropriately gowned and as relaxed as possible. Instruct the patient to let the arms hang down at the sides. A tear in the rotator cuff, particularly in the superior and posterior portion, will cause spontaneous internal rotation of the affected arm. This is due to the uncompensated action of the intact internal rotators (Fig. 1.24).
To evaluate the infraspinatus and teres minor muscles, the patient’s arm is adducted, internally rotated 45°, and flexed 90° at the elbow. With the arm in this position, the patient attempts to externally rotate the arm against resistance (Fig. 1.25). To eliminate the deltoid muscle contribution in external rotation, the external rotation can be performed at 90° abduction and 30° flexion. Failure of active external rotation with the arm abducted is indicative of a clinically relevant tear of the infraspinatus tendon (Fig. 1.26).
• Subscapularis
Increased painless passive external rotation with the patient supine and loss of active internal rotation is a sign of a subscapularis tear.
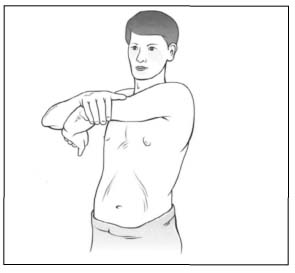
The internal rotators (subscapularis and pectoralis major) are also tested with the arm adducted and flexed at the elbow, this time with resistance against internal rotation (Fig. 1.27). The arm is not placed at the side but held in flexion to eliminate contribution of the deltoid muscle. Painful external rotation against resistance in this position is a sign of involvement of the infraspinatus tendon.

Fig. 1.26 Testing the external rotators while eliminating the effect of the deltoid muscle.

Fig. 1.27 Testing the internal rotators.
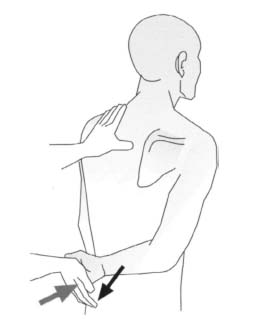
Fig. 1.28 Lift-off test as the sign of a subscapularis tear.
Lift-off test. This test can demonstrate tears in the subscapularis muscle. With the arm in internal rotation, the back of the patient’s hand is placed on his or her back at the belt line, and the patient attempts to lift the hand off the back (Fig. 1.28). A patient with a tear in the subscapularis will be unable to perform this test.
Modified lift-off test. If internal rotation is limited, the patient might not be able to place his or her hand on the back. In such cases the modified lift-off test can be used. The patient places his or her hand flat on the anterior abdomen and attempts to press with force against the abdominal wall. Inability to do so is a sign of a tear in the subscapularis tendon.
Compression and rotation test. This test is suitable for revealing degenerative changes in the glenohumeral joint. The patient lies on the unaffected side. The arm to be examined is flexed and placed at the side. Press on the humeral head from lateral to medial to produce glenohumeral compression, while the patient rotates the arm internally and externally. Cartilaginous lesions will cause audible and palpable crepitus, and the patient will experience subjective symptoms. To exclude possible accompanying subacromial pathology, inject the subacromial bursa with local anesthetic prior to the test (Fig. 1.29).
Specific Tests for the Long Head of the Biceps
Yergason test. This test demonstrates lesions of the long head of the biceps in the bicipital groove, its tendon sheath, or the transverse ligament that anchors it in the bicipital groove. The elbow is flexed 90° with the forearm pronated. The patient now attempts to supinate the forearm and flex the elbow against resistance (Fig. 1.30). Lesions in any of these structures will cause pain in the bicipital groove.
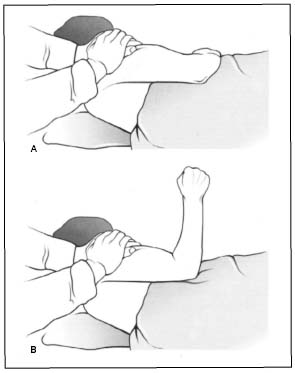
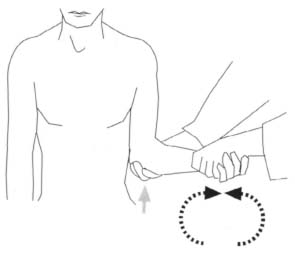
Fig. 1.30 Yergason test to evaluate the long head of the biceps.

Fig. 1.31 Speed test to evaluate the long head of the biceps.
Speed test. The speed test (palm-up test) is also used to demonstrate lesions of the long head of the biceps. The arm is in 90° forward flexion with the elbow extended and the forearm supinated. Attempt to press the extended arm down against the patient’s active resistance (Fig. 1.31). If the test is positive, the patient will complain of pain in the anterior deltoid region.
Ludington test. Both arms are abducted and the palms placed on the head with the fingers interlocked. Voluntary contraction of the biceps will cause pain in the anterior deltoid region if the test is positive.
Heuter test. Under normal conditions, forceful flexion with the forearm pronated is achieved with the brachialis. The biceps contracts simultaneously, causing supination of the forearm. If this is not observed, then you should look for a lesion of the biceps or its tendons.
The long head of the biceps is directly palpated in the Lippman and De Anquin tests.
Additional tests. These tests may be useful in demonstrating specific pathology. In the Lippman test, the examiner palpates the bicipital groove approximately 3 cm distal to the shoulder with the patient’s elbow flexed at a right angle. If the biceps tendon tends to sublux or dislocate, you can provoke dislocation or subluxation by palpation of the relaxed musculature. This is generally painful for the patient. In the De Anquin test, rotating the upper arm while palpating the biceps tendon in the bicipital groove will cause pain if the tendon is affected. In the Gilcrest test, reducing the subluxed or dislocated long biceps tendon while slowly adducting the arm will cause pain in the anterior deltoid region. The Beru sign demonstrates dislocation of the long head of the biceps tendon. If the long head dislocates, it can be palpated under the anterior deltoid when the biceps is voluntarily contracted. The Duga sign demonstrates an injury of the long head of the biceps tendon. In such an injury, the patient is unable to touch the contralateral shoulder with the hand of the affected arm.

Fig. 1.32 Stretching the long head of the biceps in the bicipital groove.
Stretch test. Passive extension of the shoulder, extension of the elbow, and pronation of the forearm, or the patient’s attempt to actively supinate the forearm, flex the elbow, or flex the shoulder forward from this position will cause pain in the anterior deltoid region (Fig. 1.32).
Compression test. Passive elevation of the arm to the end of the range of motion, and application of posterior pressure, causes pain in the tendon compressed between the acromion and humeral head (Fig. 1.33).
Clinical Tests for Glenoid Labral Lesions
O’Brien test. With the arm flexed 90° and adducted 10°, internally rotate the arm so that the thumb points down. The patient attempts to resist a downward force applied by the examiner. Pain in the acromioclavicular joint is a sign of acromioclavicular arthropathy. Pain projected to the superior part of the glenohumeral joint suggests a SLAP (Superior Labrum from anterior to posterior) lesion. Typically, the pain disappears when the arm is placed in external rotation with the palm up.
Compression and rotation test. With the arm abducted 90° and the elbow flexed 90°, apply compression to the glenohumeral joint by pressing on the humerus while rotating the joint. As in the McMurray knee test, a snapping noise is a sign of damage to the labrum.

Fig. 1.33 Compressing the long head of the biceps against the acromion.
Anterior slide test. The patient is examined either standing or sitting, with the hands on the hips and thumbs pointing posteriorly. Place one hand across the patient’s shoulder with the last segment of the index finger extending over the anterior aspect of the acromion at the glenohumeral joint. Place the other hand behind the patient’s elbow and apply force in an anterosuperior direction. Instruct the patient to push back against this force. Sudden pain in the anterosuperior shoulder, corresponding to the pain typically experienced during exercise, or a palpable snap phenomenon is indicative of a SLAP lesion (Figs. 1.34 and 1.35).
Clunk test. With the patient supine, place your hand on the posterior aspect of the shoulder directly under the humeral head. With the other hand, grasp the distal humerus and elbow condyles. The patient’s affected arm is now brought from the extended position into forward flexion and external rotation. A snap phenomenon or clunk sound indicates damage to the labrum (Fig. 1.36).
Crank test. The crank test is used to demonstrate damage to the labrum and can be performed with the patient sitting or supine. With the patient’s arm abducted 160° in the scapula plane, press along the longitudinal axis of the humerus while rotating the humerus with the other hand. The test is considered to be positive if:
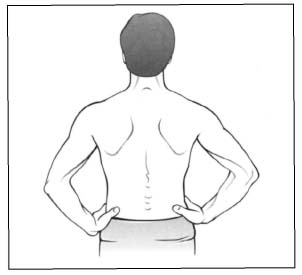
Fig. 1.34 Slide test. Position of the hands and arms for the anterior slide test.
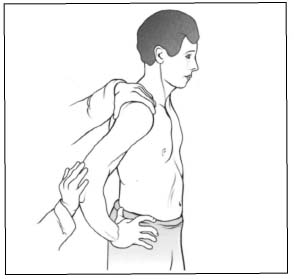
Fig. 1.35 Slide test. Application of force for the anterior slide test.
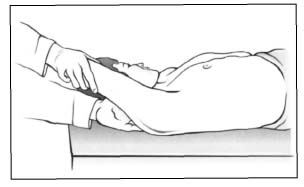
Fig. 1.36 Clunk test for diagnosing anterior lateral tears.
– The patient experiences pain during rotation (typically during external rotation) with or without a click phenomenon.
– The test reproduces the typical symptoms experienced by the athlete.
It is often an advantage if the patient is supine as he/ she will be significantly more relaxed in this position.
Specific Tests for Instability
Testing range of motion is especially crucial in a patient with suspected instability. Rotation should always be performed both in adduction and at 90° abduction. The first sign of anterior instability is often limited external rotation in both adduction and abduction. Flexion and abduction in the scapular plane are not usually limited. Occasionally, slight apprehension will be present during overhead motion. In addition to changes in the range of motion, parts of the infraspinatus and supraspinatus tendon are often sensitive to touch.
• Differentiating between instability and laxity
When evaluating shoulder instability, a clear distinction should be made between laxity and instability. Laxity refers to a hypermobile shoulder situation, such as can be demonstrated in the various translation tests, without any clinical symptoms. Laxity is often symmetric and is seen as part of generalized laxity. Instability refers to laxity with clinical impairment of the patient.
In North America, three acronyms are commonly used to classify shoulder instability. TUBS refers to Traumatic Unilateral Bankart lesion Surgery. AMBRII stands for Atraumatic, Multidirectional, Bilateral, Rehabilitation, Inferior capsular shift, Interval repair. AIOS stands for Acquired, Instability, Overstress, Surgery.
Anterior apprehension test. This test is positive in the presence of anteroinferior instability. The test is performed with the patient sitting or standing and the affected shoulder placed in 90° abduction and 90° external rotation. Continuing the external rotation while applying forward pressure to the humeral head with the thumb is met with muscular resistance as the patient feels that the shoulder is about to dislocate anteriorly (Fig. 1.37). The presence of pain alone should not be regarded as a positive test even though the muscular resistance can often appear simultaneously with the occurrence of pain. Patients will often indicate that “something bad is about to happen” or “it’s starting to go out.” This test can be performed in different degrees of abduction. Performing the test at 45° abduction evaluates the contribution of the medial glenohumeral ligament and the subscapularis tendon. In abduction of 90° and greater, the stabilizing effect of the subscapularis muscle is neutralized and contribution of the inferior glenohumeral ligament is evaluated.
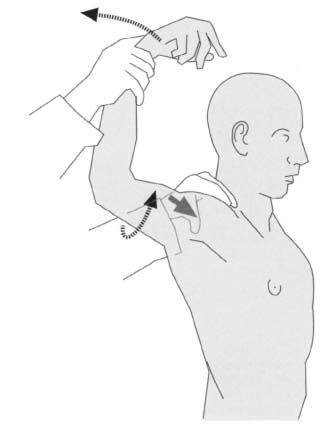
Fig. 1.37 Anterior apprehension test.
At 135° of abduction, the test primarily evaluates the anteroinferior joint capsule.
Occasionally, patients complain of pain in the posterior joint capsule. This is caused by the stretching of the joint capsule from the anterior translation of the humeral head.
A degenerative glenoid labrum with small tears can cause palpable and occasionally audible snapping during the apprehension test. Care should be taken with patients who have suffered multiple recurrent dislocations because dislocation can occur with the test. Performing the apprehension test with the patient supine is advantageous as the patient is in a more relaxed position.
Dead-arm sign. This refers to a situation in which the patient complains of a sudden stabbing pain with simultaneous or subsequent paralyzing weakness during the anterior apprehension test. This may be due to transitory pressure on the brachial plexus as the humeral head subluxes anteriorly.
Posterior apprehension test This is helpful for diagnosing posterior instability. Place the patient’s affected arm in 90° to 110° abduction at the shoulder and horizontally flex it approximately 20° to 30°. Immobilize the scapula from above with your other hand. The fingers cover the scapular spine and the humeral head while the thumb reaches anteriorly to a point slightly lateral to the coracoid process. As horizontal flexion is slowly increased, the force along the longitudinal axis of the humerus will cause the glenohumeral joint to sublux posteriorly. Both the thumb lateral to the coracoid process and the fingers can palpate the translation of the humeral head. Occasionally, the humeral head will be visible inferior to the acromion as a slight prominence. An extension of 20° to 30° in the same horizontal plane will palpably reduce the humeral head (Fig. 1.38).
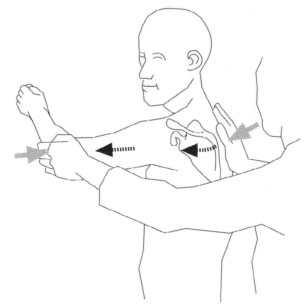
Fig. 1.38 Posterior apprehension test.
Evaluation of glenohumeral translation. Glenohumeral translation can be evaluated with the patient supine or sitting. This test provides a semiquantitative method of measuring the extent of laxity. The extent of translation is compared with the nonaffected shoulder.
Passive drawer test. When performing the test on a patient, place your contralateral hand on the patient’s shoulder from posterior so that the index and middle finger lie anteriorly on the humeral head while the ring finger lies on the coracoid process. To test for a passive drawer, grasp the shaft of the humerus with the other hand and move it anteroposteriorly, noting the translation of the humeral head in relation to the coracoid process. With the same landmarks located, you can document an active drawer by having the patient perform active abduction and external rotation of the affected arm (see Fig. 1.13).
AP drawer test. This test can also be used to document AP laxity in the shoulder. The patient is positioned supine with the arm lying comfortably at the side. Attempt to stabilize the scapula while achieving AP translation of the humeral head without encountering muscular resistance form the patient.
In the classic anterior drawer test, stand facing the affected shoulder. To examine the right shoulder, grasp the upper third of the patient’s arm with your right hand while immobilizing the patient’s forearm and hand between your body and upper arm. In this position, flex the patient’s upper arm approximately 20° and place it in slight external rotation. Immobilize the scapula with your other hand so that the fingers reach posteriorly to the scapular spine and the thumb anteriorly to the coracoid process. From this position, carefully translate the humeral head anteriorly. First perform the test at 50° abduction, repeating it at higher degrees of abduction up to 120°. This test can also produce a snapping phenomenon as a result of a torn or degenerative labrum.
Leffert test. This test is another way of obtaining quantitative information in the drawer test. Stand above the sitting patient and move the humeral head anteriorly. Anterior motion of your index finger in relation to the middle finger shows the translation of the humeral head (Figs. 1.39a, b).
Fukuda test. This test demonstrates a passive posterior drawer. With the patient sitting, place your thumbs on both scapular spines and your fingers anterior to the humeral head. Pressing posteriorly with the fingers creates a posterior drawer (Fig. 1.40).
Load-and-shift test. This test is performed similarly to the drawer test on the sitting patient. Immobilize the scapula with one hand, grasp the humeral head with the other, apply a medial force to the humerus, and translate the humerus anteroposteriorly.
Rowe test. In the Rowe test, the drawer test is performed with the patient standing and bending forward slightly. This allows the patient to fully relax the shoulder muscles as in the pendulum exercises (Fig. 1.41).
Sulcus sign. If multidirectional instability is present, a positive sulcus sign can be demonstrated. With the patient sitting or standing and the arm of the affected shoulder relaxed along the body, apply traction to the longitudinal axis of the humerus. This will widen the space between the acromion and the humeral head. A sulcus in the skin will appear in this region (Fig. 1.42).
Inferior apprehension test. For this test, place the patient’s arm in 90° abduction. While supporting the arm with one hand, attempt to provoke inferior subluxation by applying pressure to the proximal upper arm with the other hand (Fig. 1.43).
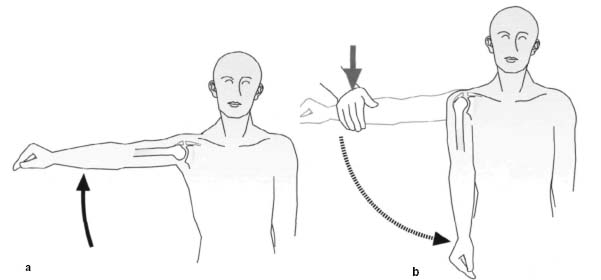
Fulcrum test. The patient is positioned supine on the examining couch with the affected arm externally rotated 90° and abducted 90°. Continuing the external rotation while moving the humeral head anteriorly will provoke muscular resistance by the patient, in combination with pain. Performing the same motion (external rotation) while moving the humeral head posteriorly is painless (Figs. 1.44a, b). This test is helpful in differentiating patients with a simple supraspinatus syndrome from those with tenosynovitis at the insertions of the rotator cuff as a result of hypermobility.
Figs. 1.39a, b Leffert test

Fig. 1.40 Fukuda test

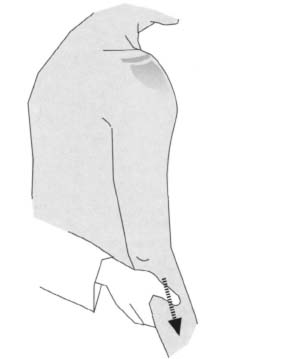
Fig. 1.42 Sulcus sign

Fig. 1.43 Inferior apprehension test.
Thrower test. In this test, the patient performs a throwing motion against your resistance. This can reveal anterior subluxation during the throwing motion (Fig. 1.45).
Examination under anesthesia. Examining the shoulder under anesthesia permits both clinical and fluoroscopic documentation of joint laxity. The drawer tests described in the previous section may be used.
Occasionally, it is helpful to have an assistant stabilize the scapula. Snapping phenomena resulting from labrum pathology can be readily documented by compressing the humeral head into the glenoid fossa while simultaneously translating the bone (shift-and-load test). The extent of translation with the arm in external rotation should be documented with the arm in various degrees of abduction (60°, 90°, and 135°). Performing a bilateral examination is recommended to allow comparison of both sides. Posterior translation up to half the humeral head diameter can be normal. Anteriorly, the normal translation is significantly less and is usually one-third of the diameter of the humeral head.
Quantifying examination under anesthesia. AP translation is divided into four grades (Fig. 1.46).
• Grade 0: no palpable translation between the humeral head and the glenoid fossa.
• Grade I: the humerus can be moved up to the margin of the glenoid.
• Grade II : Subluxation of the humeral head past the margin of the glenoid with spontaneous reduction. This is the maximum considered normal during examination under anesthesia.
• Grade III: complete dislocation without reduction.
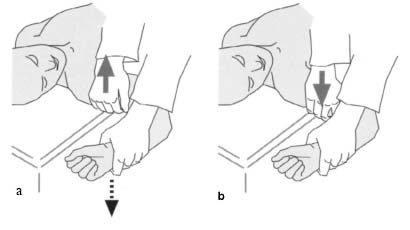
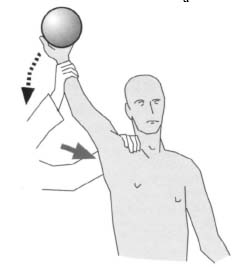
Fig. 1.45 Thrower test
Inferior translation is also graded on a scale of zero to three.
• 0: inferior translation of the humeral head with inner distance to the glenoid less than 0.5 cm.
• 1+: inferior translation between 0.5 and 1.0 cm.
• 2+: inferior translation greater than 1.0 and 2.0 cm.
• 3+: inferior translation greater than 2.0 cm.
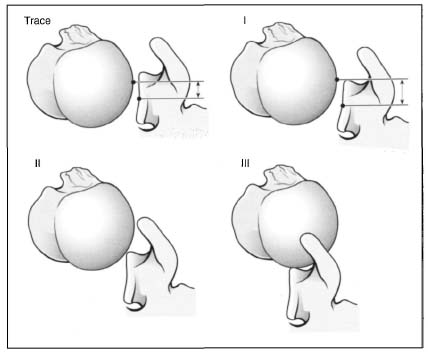
Fig. 1.46 Translation under anesthesia: humeral head translation is classified as types I–III.
| Muscle gradation | Muscle reaction |
| 0 = zero | No palpable contractility. |
| 1 = trace | Evidence of slight contractility, but insufficient to move the extremity with gravity eliminated. |
| 2 = poor | The muscle is able to move the extremity with gravity eliminated. |
| 3 = fair | The muscle is able to move the extremity against gravity. |
| 4 = good | The muscle moves the extremity against some resistance. |
| 5 = normal | Normal muscle strength against resistance. |
Neurologic Examination
The neurologic examination permits assessment of the individual muscle or muscle-group strength, testing reflexes and sensation. The examination can be performed with the patient standing or sitting.
Examining the Muscles
As in all other examinations, the strength of the muscle groups is compared with the opposite side. The chart shown in Table 1.8 is recommended for objective evaluation and documentation.
Forward flexion. Testing evaluates the anterior part of the deltoid muscle (axillary nerve, C5) and the coracobrachialis muscle (musculocutaneous nerve, C5–C6), the secondary flexors, the clavicular head of the pectoralis major, and the biceps. Stand behind the patient and place one hand over the acromion and scapula and the other above the flexed elbow; the fingers are over the anterior segment of the arm and the biceps muscle. Here and in the following tests, instruct the patient to perform the respective motion (in this case flexion). Provide resistance that the patient can barely overcome.
Extension. Testing evaluates the latissimus dorsi (thoracodorsal nerve, C6), teres major (subscapular nerve, C5–C6), and the posterior portion of the deltoid (axillary nerve, C5–C6). The secondary extensors are the teres minor and the long head of the triceps. Extension is tested in a similar position to flexion except that the palm of the hand is now placed on the posterior aspect of the humerus. Instruct the patient to extend the arm posterior, and again provide resistance that the patient can barely overcome.
Abduction. The primary abductors are the middle portion of the deltoid (axillary nerve, C5–C6) and the supraspinatus (suprascapular nerve, C5-C6). The secondary abductors are the anterior and posterior portions of the deltoid and the serratus anterior. Stand behind or beside the patient, placing your hand over the acromion. Place the other hand beside the elbow and press against the lateral epicondyle of the humerus. Instruct the patient to abduct the arm, and determine the amount of resistance that the patient can barely overcome.
Adduction. The primary adductors are the pectoralis major (pectoral nerves, C5–T1) and the latissimus dorsi (thoracodorsal nerve, C6–C8); the secondary adductors are the teres major and the anterior portion of the deltoid. Test adduction in the same position as abduction. Grasp the arm with the resisting hand so that the fingers reach the medial side of the humerus.
External rotation. The primary external rotators are the infraspinatus (suprascapular nerve, C5–C6) and the teres minor (axillary nerve, C5). The posterior portion of the deltoid is the secondary external rotator. Stand beside the patient instructing him or her bend the elbow to 90° with the arm at the side in a neutral position. Place one hand on the elbow and provide resistance on the posterior distal forearm.
Internal rotation. The primary internal rotators are the subscapularis (subscapular nerve, C5–C6), pectoralis major (pectoral nerves, C5–T1), latissimus dorsi (thoracodorsal nerve, C6–C8), and the teres major (subscapular nerve, C5–C6). The anterior portion of the deltoid is the secondary internal rotator. Standing in the same position as for testing external rotation, place your resisting hand close to the radial styloid.
Scapular retraction. The primary retractors of the scapula are the rhomboid major (dorsal scapular nerve, C5) and the rhomboid minor (dorsal scapular nerve, C5). The secondary retractor is the trapezius muscle. Stand in front of the patient and place your hands on the patient’s shoulders. Your palms should lie under the acromion with the fingers reaching around the patient’s shoulders and touching the back. Have the patient retract the scapula while offering as much resistance as the patient can barely overcome.
Scapular protraction. The primary protractor of the scapula is the serratus anterior (long thoracic nerve, C5–C7). Stand behind the patient giving instructions to elevate the arm to 90° so that the humerus is parallel to the floor. Now instruct the patient to attempt to bend the elbow so that the hand touches the shoulder. Place one hand on the patient’s spine; cup the patient’s elbow with your resisting hand.
Scapular elevation. The primary elevators are the trapezius (spinal accessory nerve or cranial nerve XI) and the levator scapulae (C3–C4 and frequently the dorsal scapular nerve, C5). The secondary elevators are the rhomboid major and minor. Stand by the patient and place one hand on each acromion. Normally the elevators of the shoulder girdle are so strong you will hardly be able to overcome them.
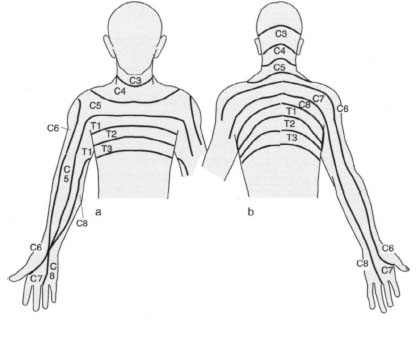
Figs. 1.47a, b Dermatomes in the upper extremity.
Reflex Testing
Always test the deep tendon reflexes on both sides. Differences in response between the two sides suggest a neurologic process.
Biceps reflex. The patient’s elbow should be flexed in a middle position and slightly pronated. Place your thumb on the distal portion of the biceps tendon and tap it. Normally the muscle will contract, causing flexion and supination of the forearm.
Triceps reflex.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree