Shock
M. Michele Mariscalco
PATHOPHYSIOLOGY
Shock is a clinical syndrome that has been characterized in cardiovascular terms. Shock states reflect a disruption in and eventual loss of normal metabolic function at the cellular level. Cellular derangement occurs because of the inadequate delivery or impaired use of oxygen, termed cellular hypoxia, and of other essential substrates. Cellular hypoxia causes the cell to shift to anaerobic metabolism; this shift causes the accumulation of lactic acid and other metabolic by-products, which can lead to further cell dysfunction. Shock can be recognized clinically by evidence of acute disruption of circulatory or other organ function, particularly of the brain, lungs, and kidneys.
Hypotension is a late manifestation of shock. The body has a host of mechanisms to maintain adequate perfusion to the central vascular bed. If a logical treatment plan is to be developed, the dynamics of the shock state must be understood.
Hypotension is a late manifestation of shock. The body has a host of mechanisms to maintain adequate perfusion to the central vascular bed. If a logical treatment plan is to be developed, the dynamics of the shock state must be understood.
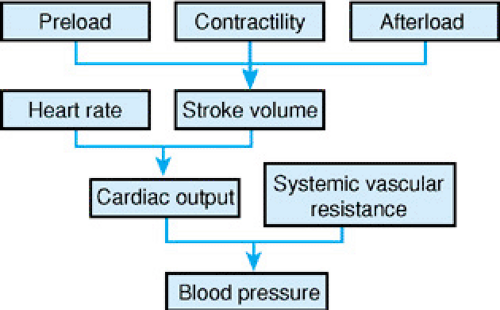
The cardiovascular system can be likened to a pump that generates pulsatile flow through a series of tubes. The pressure (blood pressure) generated by the pump (the heart) depends on the amount of fluid flowing through the tubes (cardiac output) and the resistance to that flow (systemic vascular resistance). Thus, as in Figure 453.1,
Blood pressure = cardiac output × systemic vascular resistance
If a decrease in cardiac output occurs (as in cardiogenic shock or hypovolemic shock), a compensatory increase in systemic vascular resistance occurs to maintain blood pressure. This increase is mediated by the sympathetic nervous system and endogenous catecholamines. Clinically, the patient’s periphery appears cool and mottled. In patients with septic shock, one of the primary defects is loss of systemic vascular resistance; the periphery is warm and appears vasodilated. To maintain blood pressure, cardiac output must increase to compensate for the decrease in systemic vascular resistance.
According to the model, the pulsatile flow generated by the pump depends on the rate and volume of each stroke:
Cardiac output = stroke volume × heart rate
Therefore, tachycardia should be present in most forms of shock as a compensatory mechanism to increase cardiac output. Severe bradyarrhythmias or tachyarrhythmias may themselves result in shock if the stroke volume is insufficient to compensate for the reduced cardiac output.
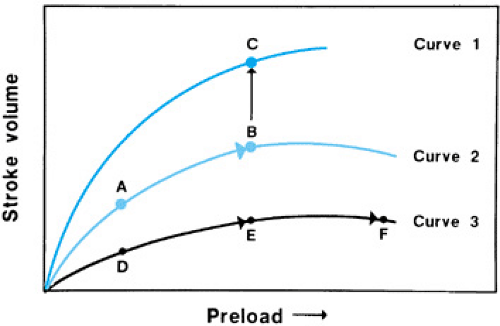
Stroke volume, the amount of blood ejected with each heartbeat, is determined by three factors (see Fig. 453.1): (a) ventricular preload, the volume of blood in the ventricle at the end of diastolic filling, which reflects venous return to the right side of the heart; (b) ventricular afterload, the impedance to the ejection of blood; and (c) intrinsic myocardial contractility. According to Frank-Starling mechanisms, the stroke volume is directly proportional to the preload (Fig. 453.2). For the myocardium to contract, the contractile proteins of the myocardial fibril, actin and myosin, must overlap. The greater the degree of stretch of the myocardial fibrils at the end of diastolic filling (i.e., increased preload), the greater the overlap of the contractile proteins and the greater the increase in stroke volume. Stroke volume decreases with increased preload if the myofibrils are stretched to the point where the contractile proteins no longer overlap.
At a given preload and afterload, the force that a myocardial fibril can generate depends on its intrinsic contractility. Contractility can be increased by the release of endogenous catecholamines, increased sympathetic stimulation of the nervous system, and the infusion of exogenous inotropic agents such as epinephrine, dopamine, and dobutamine (see Fig. 453.2). Afterload is the composite of factors that oppose ventricular ejection. These factors include resistance to flow by the arterial tree, as reflected by aortic blood pressure, and left ventricular cavity size. Afterload is inversely proportional to stroke volume. An increase in afterload decreases stroke volume, unless either preload or contractility increases concomitantly. Because blood pressure is a clinical estimate of afterload, increases in blood pressure may decrease cardiac output in certain hemodynamic states. Thus, support of blood pressure does not guarantee adequate delivery of blood and oxygen to the tissues.
Oxygen delivery to the tissues is defined as:
Oxygen delivery = hemoglobin level × saturation × cardiac output
In addition to cardiac output, the hemoglobin content of the blood and the oxygen saturation of the hemoglobin are important in oxygen delivery. If delivery is inadequate for cellular needs, cellular hypoxia results. Examples of inadequate oxygen delivery from decreased cardiac output include cardiogenic and hypovolemic shock. In contrast, in septic shock, cellular dysfunction occurs secondary to an intrinsic inability to use oxygen and/or increased needs above baseline, as well as a decrease in oxygen availability from peripheral vasodilation and decreased preload.
With these basic principles in mind, the practitioner can understand and treat the initial hemodynamic derangements seen in various shock states. In cardiogenic shock, the underlying hemodynamic dysfunction is in cardiac contractility; in hypovolemic shock, a decrease in preload volume occurs; and in septic shock, the initiating event is a decrease in systemic vascular resistance and hypovolemia. Hypoxia (absolute oxygen deficit) and ischemia (oxygen and substrate deficit) occur at some time in all types of shock. Either of these insults leads to lactic acidosis and the release of vasoactive metabolites and other mediators that are responsible for a host of cellular injuries. Some metabolites and mediators can cause an increase in capillary permeability that leads to a decrease in intravascular volume; others are direct depressants of myocardial contractility, which leads to further hemodynamic compromise and multiorgan dysfunction. Thus, the shock cycle perpetuates itself.
Unfortunately, the clinician can do little to interrupt the action of the mediators of cellular injury. Support of oxygen
delivery and blood pressure, along with specific measures to treat the underlying injury or infection, is critical to stopping the shock cycle. Success is greatest when shock is recognized and appropriate therapy is begun before the onset of hypotension.
delivery and blood pressure, along with specific measures to treat the underlying injury or infection, is critical to stopping the shock cycle. Success is greatest when shock is recognized and appropriate therapy is begun before the onset of hypotension.
ETIOLOGIES
Hypovolemia is the most common cause of shock in infants and children. Hypovolemic shock is defined best as a sudden decrease in the intravascular blood volume, relative to vascular capacity, that prevents effective tissue perfusion from being maintained. Causes include hemorrhage from gastrointestinal loss or trauma, plasma loss from burns, and fluid and electrolyte loss, such as occurs from vomiting and diarrhea or endocrinologic disease (e.g., adrenal insufficiency, diabetes insipidus, diabetic ketoacidosis).
Cardiogenic shock is the state in which an abnormality of cardiac function is responsible for the failure of the cardiovascular system to meet the metabolic needs of tissues. Common to all causes of cardiogenic shock is depressed cardiac output. In most cases, the depressed output is caused by decreased myocardial contractility. Decreased myocardial contractility may be caused by an idiopathic cardiomyopathy, by metabolic processes or inflammation of the myocardial muscle itself, or by hypoxic-ischemic events. In other cases, acute heart rate changes may result in inadequate preload (such as occurs with supraventricular tachycardia or ventricular dysrhythmias). Severe bradycardia may lead to shock if stroke volume cannot increase to maintain cardiac output.
Distributive shock is caused by a maldistribution of blood flow to the tissues. Such maldistribution of flow results from widespread abnormalities of vasomotor tone. Profound inadequacies in tissue oxygenation can occur, even in the face of a normal or high cardiac output. Distributive shock can occur with anaphylaxis, spinal or epidural anesthesia, or disruption of the spinal cord.
Septic shock is the most complex and controversial type of shock. It comprises a cascade of metabolic, hemodynamic, and clinical changes resulting from invasive infection and the release of microbial toxins into the bloodstream and the host’s response to them. Septic shock often is the combination of multiple problems, including hypovolemia with maldistribution of blood flow, myocardial depression, and multiple metabolic and endocrine derangements. Initially, in the early stage of sepsis, adult patients present in a hyperdynamic state characterized by elevated cardiac output, decreased systemic vascular resistance, widened pulse pressure, and warm extremities. If sepsis progresses, steady deterioration in cardiovascular performance occurs, marked by a decline in cardiac output, hypotension, and metabolic acidosis. In children with sepsis after fluid resuscitation, only about 20% demonstrated low systemic vascular resistance and increased cardiac output. Almost 60% had increased systemic vascular resistance and low cardiac output, and another 20% had low systemic vascular resistance and low cardiac output. Thus, children need specific therapies to address each of these states.
DIAGNOSIS
The key to making an early diagnosis of shock is to have a high index of suspicion and a knowledge of which conditions predispose children to shock. A correct diagnosis can be made only after a patient history has been obtained. Given the exigencies of the case, the history may be brief initially, but it is crucial in providing optimal stabilization.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree