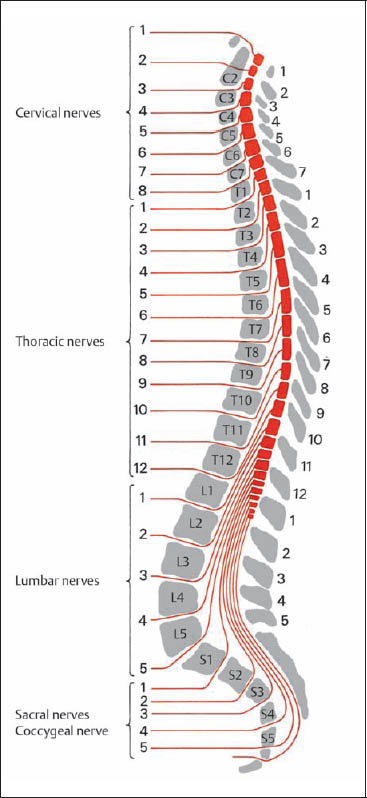
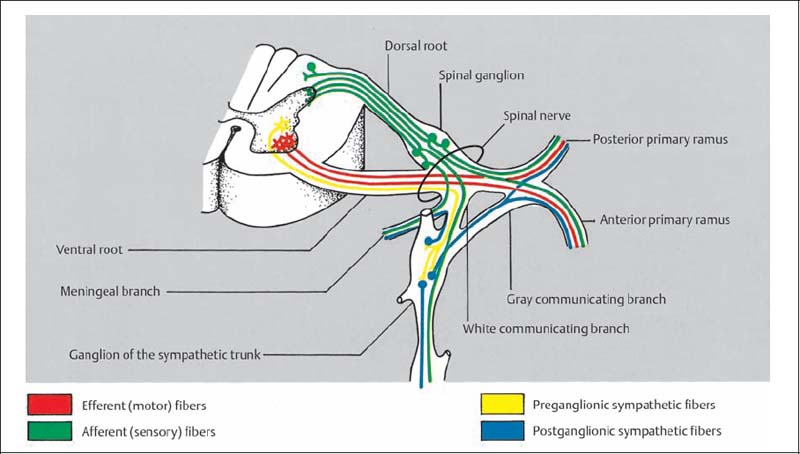
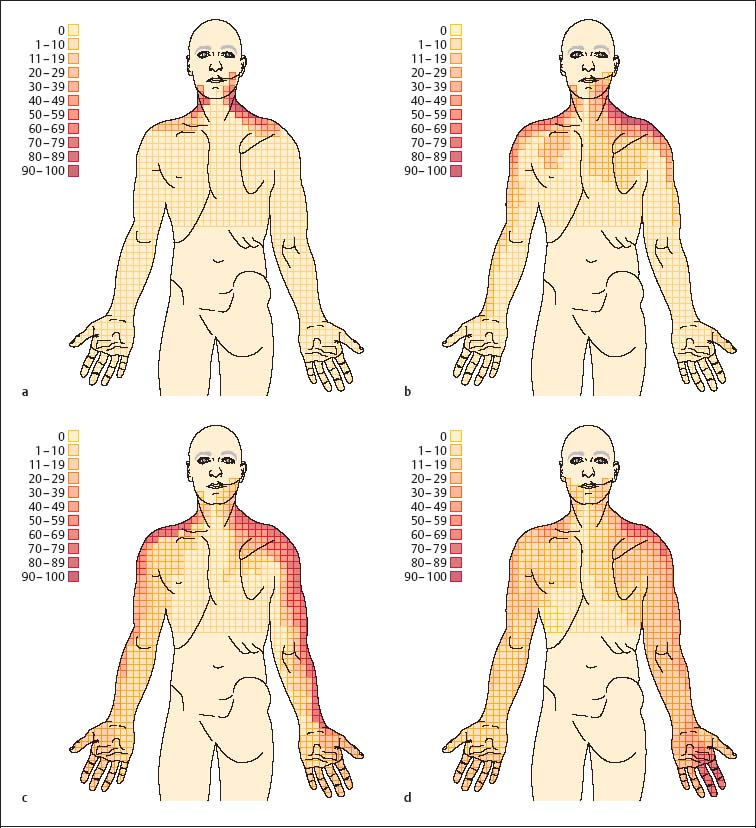
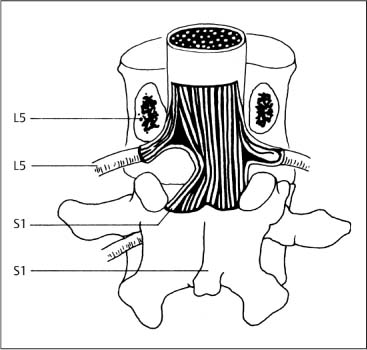
14 Selected Clinical Syndromes In 1955, Gutzeit referred to Mixter and Barr’sclassic article in the New England Journal of Medicine (Mixter and Barr, 1934) as a “turning point” in spine care. Prior to this article, there was generally the perception, especially by osteopathic physicians and chiropractors, that pain of vertebral origin could be positively influenced through specific manual treatment of the spine (think of this as “Chapter 1”). Soon after the publication of Mixter and Barr’s eminent article on the surgical removal of the herniated intervertebral disk it was believed that disk surgery could “cure” such entities as rheumatic ischialgia, and sciatica. Almost to the exclusion of conservative treatment options, surgical spine care became the accepted mainstay for years to come (this is “Chapter 2”). Today, both of these “Chapters” bear great significance, especially since “Chapter 3” is being written as we speak and draws upon both of the earlier ones. Guided by evidence-based medicine, one of today’s missions in good spine care is to evaluate the evidence of the relevant usefulness of any of the various treatment options described at times up to and including today: from doing nothing (“it will get better anyway”); to the conservative measures, including the hands-on manual, pharmacologic, and behavioral approaches; to interventional spine care (injections, nerve blocks, denervation procedures, among others) and finally spine surgery. Against this backdrop, and as true today as in the past, the diagnostic work-up and management of spine-related pain starts with the fundamentals of good medical care by making sure that the patient receives a thorough medical and pain history-taking and a detailed neurological and orthopedic examination. In addition to the standard medical approach, manual medicine examination routines provide further structural and functional information about specific segmental spinal joint dysfunctions as well as adaptive or compensatory global or regional musculoskeletal changes. The goal of the manual medicine practitioner is to determine the relevance of such findings within the entire clinical presentation, to elicit additional information that may aid in prognosis, and to provide management options that are not otherwise available in order to reduce pain and improve function within the entire bio-psycho-social context. The manual medicine approach that uses an individualized treatment approach with specific hands-on maneuvers (diagnostic and therapeutic), in combination with individually tailored exercise and lifestyle and activity modifications, may be indicated to address a clinical situation in which there is nonradicular or pseudoradicular pain, or where one of the pain-generators may be in the facet–joint–fascia–muscle–sympathetic nervous system complex. As a result of their extensive palpatory experience, manual medicine practitioners in allopathic medicine (Maigne, 1970), osteopathic medicine (Beal, 1984; Greenman and Buerger, 1984; Jones, 1981; Mitchell et al., 1979), and chiropractic (Walther, 1981) have made considerable contributions to the field of musculoskeletal medicine by refining and expanding on the structural and functional diagnosis of the musculoskeletal system, especially the vertebral column and the paraspinal and other soft tissues. In the final assessment, then, the true goal of good spine pain care is to provide the best patient-centered management with the most specific treatment, as early as possible in order to maximize individual functional outcomes. Pain, especially movement-related pain, should be considered a complex interplay, not solely as a psychiatric or a neurologic problem but rather as a problem related to the integration of nervous and biomechanical mechanisms, and the various feedback mechanisms from muscles, fasciae, disks, and joints in relationship to their central, autonomic, and peripheral nervous system interactions (Holm and Indahl, 2004). Pain and the associated functional deficits are what—ultimately—prompt the patient to seek medical help. A recent study (Videman and Nurminen, 2004) reported that the frequency of back pain had a highly significant relationship to the occurrence of lumbar anular tears. Utilizing barium sulfate discography in more than 150 specimens, Videman and Nurminen conclude that anular degeneration and tears of the lumbar disks appear earlier and are more clearly related to back pain than previously thought. While the underlying “source” may be the anular tears, it becomes important to address as soon as possible the adaptations and compensatory reactions not only at the level of the tears (localized reactions) but also the effect these ultimately have on the entire body, such as postural changes, muscle activities, or recruitment of “new” muscle patterns, and avoidance of certain activities for fear of pain (generalized reactions). The indications for surgery remain a matter of ongoing discussion, especially when considering the results from various outcome studies. Deyo’s excellent review of the role of outcomes research points out that, for low back disorders, traditional measures such as death, cure, and physiologic outcomes have some, but limited, applicability (Deyo, 2004). Deyo states that in many cases, patient’s symptoms, function, and work status are the most important outcomes to measure. He furthermore points out that extreme care is warranted to ensure that comparisons are fair when comparing providers as to quality of care and treatment effectiveness. According to their prospective study of 131 patients, Komori et al. (2002) concluded that while the initial assessment and type of a herniated nucleus pulposus on MRI evaluation could be used as major prognostic factors, the conventional manner of treatment selection appears inadequate for the appropriate management of lumbar disk herniation. From an international perspective, the United States appears to perform roughly twice as much back surgery as most developed countries, and five times more back surgery than the United Kingdom (Cherkin et al., 1994). Large statistical analyses indicate that conservative measures show satisfactory results in 80% of patients (Jörg, 1982). In former West Germany, for instance, 20 000 patients underwent lumbar disk surgery in one year (Schirmer, 1981). The question whether the surgical procedure was indicated in all of these patients remains unanswered. In the authors’ own experience, approximately one-third of patients who had undergone back surgery were later dissatisfied with the results, and between 10% and 20% of the patients were in partial or complete disability (Dvořák et al., 1988c). On the other hand, one can say that surgery was able to help the majority of these back pain sufferers, and offers legitimate if not total curative potential. These statistics and clinical experiences should be thought-provoking, because only a few decades ago the criteria for surgery appear to have been much stricter. Certainly, surgical technology, experience, and treatment options might not have been as advanced as they are today, yet it is interesting to note that residual symptoms have been observed less frequently in those elderly patients who were seen by a physician at a time when practitioners were more reluctant to use surgical intervention to treat low back pain (Jörg, 1982). In this context, the conservative approach, based on functional and palpatory examination of patients with back pain, assumes a paramount role. If complaints continue to be reported by the patient despite what would be considered successful therapy (i. e., surgery), the question of psychologic overlay is sometimes raised. However, it is extremely difficult to determine whether there had been preexisting psychologic factors that played into the pain situation, or whether the pain resulted in psychological changes, such as anxiety, depression, or behavioral changes. In some cases then, it may actually be beneficial to arrange for preoperative psychological evaluation (i. e., the Minnesota Multiphasic Personality Inventory [MMPI]), as the results may influence the decision whether or not to operate (Cashion and Lynch, 1979; Southwick and White, 1983; Herron and Turner, 1985; Dvořák et al., 1988c). It is still the case today that a helpful piece of information is the location of the pain as described by the patient (Yoss, 1957). To recapitulate, the key to good management is the individual practitioner’s ability to integrate the current evidence for back pain (see further reading: Deyo and Weinstein 2001) and for neck pain (see further reading: Tsang, 2001). While the evidence may change from time to time, it is the “partnership” of up-to-date knowledge with real-world patient experience and its application to individualized patient care that will ultimately determine outcomes. In addition to performing the best possible patient history and detailed neuromusculoskeletal examination, the judicious use of imaging techniques and appropriate referral strategies is key (Findlay, 2002). The remainder of this chapter will attempt to provide a practical, and admittedly not an exhaustive, overview of various disorders or syndromes as they relate to pain and the spine. Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001; 344(5):363–370. Hazard RG. Failed back surgery syndrome: surgical and non-surgical approaches. Clin Orthop Relat Res. 2006;443:228–232. Henry SM, Hitt JR, Jones SL, Bunn JY. Decreased limits of stability in response to postural perturbations in subjects with low back pain. Clin Biomech (Bristol, Avon). 2006;21(9):881–892. Manek NJ, MacGregor AJ. Epidemiology of back disorders: prevalence, risk factors, and prognosis. Curr Opin Rheumatol. 2005;17(2):134–140. Pahl MA, Brislin B, Boden S, et al. The impact of four common lumbar spine diagnoses upon overall health status. Spine J. 2006;6(2):125–130. Smeets RJ, Wade D, Hidding A, et al. The association of physical deconditioning and chronic low back pain: a hypothesis-oriented systematic review. Disabil Rehabil. 2006;28(11):673–693. Speed C. ABC of rheumatology. Low back pain. BMJ 2004;328:1119–1121. Speed CA, Crisp AJ. Referrals to hospital-based rheumatology and orthopaedic services: seeking direction. Rheumatology. 2005;44(4):469–471. Tsang I. Rheumatology: 12. Pain in the neck. CMAJ. 2001;164(8):1182–1187. Wasan AD, Kaptchuk TJ, Davar G, Jamison RN. The association between psychopathology and placebo analgesia in patients with discogenic low back pain. Pain Med. 2006;7(3):217–228. All but three of the 31 pairs of the peripheral nerve roots exit the spinal column through intervertebral foramina. The first cervical root exits between the occiput and the atlas, and the last sacral and the only coccygeal nerve exit via the sacral hiatus (Fig. 14.1). The faster growth rate of the vertebral column results in a height difference between the spinal cord level and the vertebral level. Due to this displacement, the nerve roots in the lumbar and sacral region run laterally and almost vertically to their point of exit in the intervertebral foramen. This is in contrast to the cervical roots, which are nearly aligned with the horizontal plane. The length of the roots increases from a few millimeters to about 25 cm (Mumenthaler and Schliack, 1977). The spinal cord inferior to L2 contains nerve roots only, and is referred to as the cauda equina. Fig. 14.1 Relationships between the individual nerve roots, spinal nerves, and vertebral levels. (After Borovansky, 1967a). Anatomic relationships between spinal nerve and vertebra: • In the cervical spine, the same-named spinal nerve leaves the cord above its respective vertebra (e. g., C1 spinal nerve leaves above C1 vertebra, C2 spinal nerve above C2 vertebra, until C8 spinal nerve, which leaves above T1 vertebra). • Starting from the T1 vertebral level, the spinal nerve related to the particular vertebral level leaves the cord inferior to its respective vertebra (e. g., T1 spinal nerve leaves inferior to T1 vertebra, T2 spinal nerve inferior to T2 vertebra, and so forth all the way inferior down to • The lumbar spine (e. g., L5 spinal nerve and ultimately the S5 spinal nerve, which leaves inferior to the S5 “vertebra” (fused here). Disk herniation level and spinal nerve root involvement • Nerve root compression follows the same “rule,” even though the rationale is different for the various spinal regions: in general, it can be said that at any spinal unit with intervening disk (e. g., C5–C6disk) will impinge on the spinal nerve that is named according to the lower partner (in this example, the C6 spinal nerve). • In the cervical spine, if the C3–C4 disk is involved, one would expect the C4 spinal nerve root to be impinged. • In the lumbar spine, a disk herniation between L5 and S1 (one of the most common areas of lumbar disk herniation) would impinge on the S1 nerve root (also see Fig. 14.3). Note that C1 nerve root leaves the cord above C1 (atlas), and the C8 nerve root above T1. Fig. 14.2 Schematic representation of the nerve fibers of one individual spinal nerve. Note the pre- and post-ganglionic sympathetic connections. The spinal nerve roots are positioned for the most part intradurally. The pia mater covers the initial portions, and the arachnoid runs along the roots, terminating at the root pockets formed by the dura. Both the anterior and the posterior roots exit through separate openings in the dura before they unite to form the spinal nerves. After leaving the intervertebral foramen, the spinal nerve divides into four typical rami (Fig. 14.2). The meningeal nerve contains both sensory and autonomic fibers and returns to the spinal cord. The white communicating branches of the sympathetic fibers are directed to the corresponding ganglion of the sympathetic trunk in the paravertebral region. A section of the post-ganglionic, less-myelinated sympathetic fibers returns to the nerve roots via the gray communicating branches. The remaining fibers continue to the visceral organs. The rami communicantes contain sensory fibers in addition to autonomic fibers that pass through the ganglion and terminate at the visceral organs. Further, each spinal nerve root divides into a dorsal ramus and a ventral ramus. With the exception of the first and second dorsal rami of the cervical spinal nerve (the suboccipital nerve and greater occipital nerve, respectively), the ventral rami are substantially thicker than the dorsal rami. It is important for practical purposes to appreciate the topographic relationship of the nerve root to two spinal “tunnels,” namely: (1) the spinal canal, and (2) the intervertebral foramina. The vertebral bodies, the vertebral arches, and the articular processes form the bony limitations, whereas the joint capsule and the intervertebral disk represent the soft-tissue borders. Fat tissue (which is easily noted in a CT or MRI scan) and the venous plexuses actually cushion the spinal nerve against the wall. It is of clinical significance that the diameter of the intervertebral foramina decreases from L1 to L5, whereas the circumference of the nerve roots increases severalfold from superior to inferior. In addition to radicular pain that is caused by compression upon the nerve itself, any of the surrounding osseous and soft-tissue structures may serve as a source of pain (Wyke, 1967). The joint capsule of the small apophyseal joints seems to play a special role in the character of nonradicular pain, sometimes termed referred pain or pseudoradicular pain (Brügger, 1977; Feinstein et al., 1954; Hockaday and Whitty, 1967; Kellgren, 1938; Korr, 1975; Reynolds, 1981; Sutter, 1975; Wyke, 1967, 1979). In a more recent study of the cervical spine, Slipman and colleagues determined that the areas of symptom provocation of fluoroscopcially guided cervical nerve roots is similar to but not identical with the “old” dermatomal maps of spinal nerve distribution. These symptom-provoked maps are termed “dynatomes” by these authors and are represented in Figs. 14.3a–d. (Slipman et al., 1998). Fig. 14.3a–d Dynatomes of the C4, C5, C6, and C7 levels (Slipman et al., 1998). Representation of the various dynatomes: the area of symptom provocation of fluoroscopically guided cervical nerve roots. a C4 nerve root. b C5 nerve root. c C6 nerve root. d C7 nerve root. The topographic relationship between the nerve roots and the intervertebral canal and the disk, as well as the differing loads on the individual spinal segments (also known as vertebral units), is primarily responsible for disk protrusion (or prolapse) that occurs most frequently at the lower lumbar and first sacral root levels. The relationship between the diameter of the nerve root and the intervertebral canal is distinctly unfavorable in the lumbosacral junction in comparison to other segments of the spinal cord. Apart from the limited spatial arrangement, the vertical course of the nerve roots at the lumbosacral junction can cause the next root to come into contract with the intervertebral disk as well. The posterolaterally herniated disk at L4–L5 primarily compresses the fifth lumbar nerve, whereas the disk of L5–S1 compresses the first sacral nerve. The nerve root leaving the intervertebral foramen in this vertebral unit can exit without compression. When the disk herniation is substantial, the L4–L5 and L5–S1 disk or a radicular syndrome can arise (Fig. 14.4). The incidence of the radicular syndrome from involvement of the cervical nerve roots is about one percent of that encountered in the lumbar region. The root of C6 is involved most frequently, which may be due to the comparatively large mobility of the segment C5–C6. Thoracic root syndromes are extremely rare. The clinical presentation of a herniated disk in the mid-thoracic spine can be very dramatic, however, since the diameter of the canal of the spinal column between T4 and T9 is very small and the vascular supply is markedly decreased in comparison to the remaining segments of the spinal cord (White and Panjabi. 1978). These two factors can increase the likelihood of injury as the consequence of a “contrecoup” mechanism involving the spinal cord and the nerve roots (Fig. 14.5). Compression of the individual nerve roots is typically accompanied by the following signs and symptoms (Table 14.1): • Pain following the dermatomal region supplied by the incriminated nerve root (s). • Radicular loss of sensitivity along a dermatomal distribution. • Motor loss of the muscles innervated by the corresponding roots. • Abnormal (reduced or absent) muscle stretch changes. Fig. 14.4 Schematic representation of a large lateral lumbosacral disk herniation between L5 and S1, which compresses not only the first sacral root (S1, which would be expected) but also the fifth lumbar root (L5) (after Dubs, 1950). Typically, the L5 nerve root should have left the canal above the L5–S1 disk level (in other words, L5 spinal nerve leaves “below” the L5 vertebra). However, if the disk is sufficiently large, it can extend and compress the L5 root by pushing “up” on the nerve root from below. The S1 nerve root at that level is still mostly in the spinal canal on its nearly vertical course to leave the canal just under the S1 vertebral level. Cyteval C, Fescquet N, Thomas E, et al. Predictive factors of efficacy of periradicular corticosteroid injections for lumbar radiculopathy. Am J Neuroradiol. 2006 May;27(5):978–992. Dvořák J, Grob D. Epidural injections. What is certain? Orthopäde. 2004;33(5):591–593. Hirayama J, Yamagata M, Ogata S, et al. Relationship between low-back pain, muscle spasm and pressure pain thresholds in patients with lumbar disk herniation. Eur Spine J. 2006;15(1):41–47. Kendall R, Werner RA. Interrater reliability of the needle examination in lumbosacral radiculopathy. Muscle Nerve. 2006;34(2):238–241. Rothman SM, Kreider RA, Winkelstein BA. Spinal neuropeptide responses in persistent and transient pain following cervical nerve root injury. Spine. 2005 Nov 15;30(22):2491–2496. Waggershauser T, Schwarzkopf S, Reiser M. Facet blockade, peridural and periradicular pain therapy [in German] Radiologe. 2006;46(6):520–526. Fig. 14.5 Schematic cross-section of the spinal cord at different levels and the blood supply in the various spinal regions. Demonstration of the contrecoup phenomenon seen with thoracic disk herniations. The small spinal cord cross-sectional area in the thoracic spine, coupled with the smallest blood supply in this region, is felt to be responsible for the potentially disastrous outcomes when the mid-thoracic spine is injured. With permission from White and Panjabi, Clinical Biomechanics of the Spine, Lippincott Williams & Wilkins, 1990. An excellent review of the literature was presented by Mattle (1986). The following descriptions are based on and expand this review. In the presence of prolonged and prominent radicular symptoms, differentiation must be made between a cervical herniated disk and an extramedullary, intraspinal tumor. Schwannomas (neurilemmomas) are the most frequently encountered tumors (Burger and Vogel, 1982). These tumors are benign. When they are found during the course of the clinical work-up in a patient with radicular symptoms, surgical interventions are associated with good outcomes (Fig. 14.6). However, the prognosis is worse in a patient with a transection-type of injury to the spinal cord. Causes of such an injury may include prolonged compression of the spinal cord by the tumor or, as in an acute situation, occlusion of the anterior spinal artery. Schwannomas may grow along the nerve root and extend inferiorly beyond the intervertebral foramen, thereby enlarging it at the same time. This can be demonstrated on oblique radiographs, and better yet on axial CT scans or MRI. It can be weeks to months before neurological deficits associated with intramedullary space-occupying lesions become clinically noticeable. The presentation may be neck pain or back pain, or both. There is usually segmental, radiating pain corresponding to the level of tumor involvement, as well as distal paresthesias and peripheral paresis or overt paralysis. Segmental muscle weakness and atrophy or fasciculations are sometimes seen on physical examination. Below the level of involvement, a central palsy and dissociated sensory changes can occur (loss of pain and temperature sensation with preserved proprioceptive and touch modalities). Frequent causes of space-occupying lesions include astrocytomas and ependymomas. If the symptoms have extended over years, and especially when the patient has not had a prior neurologic work-up (e. g., the patient has not seen a physician), a syringomyelia should be suspected. The causes of syringomyelia may include malformations such as basilar impression or Klippel–Feil or Arnold–Chiari syndromes. The diagnosis is made either by CT or by MRI (Fig. 14.7). Fig. 14.6 Demonstration of a neurinoma in the left intervertebral foramen at C5–C6 (oblique view). Fig. 14.7 Syringomyelia in the upper cervical spine as demonstrated via MRI in this 52-year-old man. Probably due to bony abnormality in the upper cervical spine. Diffuse pain that develops over a relatively short period of time and that can be localized to a particular spinal region or specific vertebrae with possible dermatomal radiation may be due to metastatic carcinoma of the bone (Harner and Wiernir, 1982). The spine is recognized as one of the most common sites, if not the most common site, for bony metastases in patients with systemic malignancy (Ecker et al., 2005) . Patients with metastatic spinal tumors may present with pain, neurologic deficit, or both, while it should be remembered that some tumors can be entirely asymptomatic (Ecker et al., 2005), metastases usually reach the spinal cord anteriorly, therefore causing more destruction on the anterior components of the cord than the posterior ones. Clinically, there may be paraparesis with loss of pain and temperature sensation, whereas touch and positional sensation are usually preserved. Conventional radiographs, in particular the anteroposterior view, may reveal bony changes, and particular attention should be paid to the arches of the roots. Whenever a patient presents with “obvious” spinal pain, e. g., pain that would point to degenerative disk or joint disease, the entire clinical situation should be taken into account, including the patient’s age, trauma, and the potential for any underlying and yet-to-be-recognized sinister pathology. A recent case underscores the medical necessity for being “on the alert,” as here the patient presented with upper thoracic pain of prolonged duration only to reveal metastasis of poorly differentiated carcinoma (Stoll et al., 2005). Neurogenic shoulder amyotrophy is primarily a lower motor neuron disorder with pain. It is characterized by initial constant, severe pain or sharp, throbbing, stabbing pain. The pain may be exacerbated by shoulder motion, and the pain may actually wake the patient from sleep. Frequently, it is not until the original sharp pain has subsided that the patient realizes the presence of weakness, atrophy, or even paralysis in the upper arm (Fig. 14.8). Tsairis et al. (1972) report that in approximately half of the patients investigated the weakness was confined to the shoulder region, with the majority of the deficits suggestive of multiple nerve lesions (90% vs. 10% suggestive of individual nerves; e. g., radial, long thoracic, or suprascapular nerve). Sensory changes may be present, especially in the region over the deltoid muscle and the lateral side of the forearm. By definition, if the patient’s presentation can be attributed to one or several nerve roots or extrinsic cord compression, it is not neuralgic amyotrophy. Fig. 14.8 Neuralgic shoulder amyotrophy visible in this 60-year-old man. Note the prominent atrophy of the right shoulder blade muscles. The polyradiculopathy in Guillain–Barré syndrome usually progresses without much pain except for initial paresthesias at the onset (Loffel et al., 1977; Guillain et al., 1916). It has occasionally been observed that a patient complains of nonspecific lumbago-like, nonspecific low back pain for days to weeks preceding the muscle weakness. A polyradiculitis caused by spirochetes (Lyme disease; Borrelia burgdorferi infection, borreliosis) is usually characterized by monosegmental or plurisegmental pain and may reveal severe, pronounced peripheral muscle weakness (Pacher and Steere, 1985; Schmitt et al., 1985; Steer et al., 1983). Asking specifically whether the patient has been bitten by a tick or has traveled to tick-infested areas may help in specifying this diagnosis, especially when the exposure is followed by skin changes consistent with erythema chronicum migrans (“target lesion” or “bull’s eye lesion”). Laboratory examination of the spinal fluid of the patient infected with spirochetes usually reveals an increased cell count. Confirmation of a diagnosis of spirochete infection requires serological testing. It is difficult to differentiate dermatomal pain from other causes in a patient who suffers from a herpes zoster infection, for instance, but who has not progressed beyond the prodromal period, until the vesicles actually appear (Mumenthaler, 1985). A recent article investigating potential differences in pain pathways associated with either radicular pain or neuropathic/neurogenic pain reports that while the two models of persistent pain may produce similar allodynic outcomes, there is a difference in gene expression (Lacroix-Fralish et al., 2006). According to their pain models, these authors suggest that diverging mechanisms may lead to a common behavioral outcome. The vessel most frequently involved is the anterior spinal artery. Occlusion of this artery may lead to a central monoparesis with contralateral dissociated sensory disturbances, that is, the Brown–Sequard syndrome (Aminoff, 1996) (Figs. 14.9a, b). These neurological deficits are often accompanied by acute back pain which radiates segmentally. There is flaccid paresis in the segmentally related muscles in the presence of circulation abnormalities. According to Kelley (1991), transient occlusion of the anterior spinal artery due to aortic thrombosis may cause paraplegia and may also progress to renal failure, bowel infarction, and limb loss if left untreated. Abdominal aortic thrombosis should be considered in a patient who presents with an anterior spinal artery syndrome, which, if present, must be treated as rapidly as possible to preserve motor and sensory function. The occurrence of a spontaneous spinal epidural hematoma is rare (Foo and Rossier, 1981). Immediate diagnosis of this disorder and prompt laminectomy will prevent the patient from becoming permanently disabled (Mattle et al., 1987). The first clinical symptoms the patient complains about are usually severe neck pain or back pain, or both, soon followed by pain radiating along the distribution of the incriminated nerve root. Within minutes to hours, or perhaps days, the patient may develop a transection type of cord injury with paraplegia. The possibility of a spontaneous spinal epidural hematoma should always be considered when there is acute pain, especially when the patient is on anticoagulation medication. The diagnosis is confirmed by CT or MRI, replacing the formerly “standard” myelogram. Favorable surgical outcomes of SSEH include an incomplete neurological injury at the time of the preoperative status (vs. complete neurological injury) and a short operative time interval (Shin et al., 2006). Fig. 14.9a,b The original presentation of the Brown-Séquard syndrome. Extremely severe and well-localizable pain in patients with signs of a systemic infection and fever may be due to an epidural abscess. In most cases Staphylococcus is the offending organism (Kaufmann et al., 1980; Baker et al., 1975). The abscess causes the dura to bulge into the spinal cord, whereby it applies mechanical pressure on the cord, which in turn can impair normal spinal circulation. The ensuing paraplegia may progress quite rapidly Today the diagnosis is made by MRI, whereas in the past myelograms were required (An and Seldomridge, 2006; Stäbler and Reiser, 2001). Therapeutic intervention includes surgical decompression by drainage, possible laminectomy and appropriate intravenous antibiotic coverage. A recent case report of a 44-year-old man who developed paraplegia due to a paraspinal and epidural abscess after reported spinal manipulative intervention (with a reported delay in diagnosis) highlights once more the need for comprehensive clinical vigilance in order to initiate the appropriate diagnostic work-up promptly when the situation dictates, and especially when there is well-localizable back pain (Wang et al., 2006). Lumbar spinal stenosis should be suspected especially in the elderly patient who presents complaining of chronic back pain with radicular symptoms and with intermittent neurogenic claudication (Blau and Loque, 1978; Benini, 1981; Hohmann et al., 1984). The patient’s history usually reveals the need for frequent rest periods after walking a short distance. Furthermore, a change in posture, such as leaning forward (e. g., supporting oneself over the cart when shopping) or assuming a sitting position, is necessary to bring about some relief. To demonstrate possible deep tendon reflex changes, alteration in sensation, as well as muscle weakness, it is often necessary to have the patient move until the state of claudication is reproduced. Electro-diagnostic studies may provide additional information, especially when the presentation is relatively “classic” but the neurologic examination is rather unremarkable. MRI or CT have become the mainstay tools in the diagnostic work-up, in addition to a thorough history and physical examination (Fig. 14.10). Fig. 14.10 Central canal spinal stenosis as demonstrated in a conventional myelogram (a) and with myelo-CT (b) in a 74-year-old man who had presented with neurogenic claudication. Note the complete interruption of flow of the contrast material at the L4–L5 level, where there is also noted a pseudospondylolisthesis. Atlas SJ, Delitto A. Spinal stenosis: surgical versus nonsurgical treatment. Clin Orthop Relat Res. 2006 Feb;443:198–207. de Graaf I, Prak A, Bierma-Zeinstra S, et al. Diagnosis of lumbar spinal stenosis: a systematic review of the accuracy of diagnostic tests. Spine. 2006 May 1;31(10):1168–1176. Huntoon MA. Anatomy of the cervical intervertebral foramina: vulnerable arteries and ischemic neurologic injuries after transforaminal epidural injections. Pain. 2005 Sep;117 (1–2):104–111. Kluner C, Kivelitz D, Rogalla P, et al.. Percutaneous discography: comparison of low-dose CT, fluoroscopy and MRI in the diagnosis of lumbar disk disruption. Eur Spine J. 2006 May;15(5):620–626. Vogt MT, Cawthon PM, Kang JD, et al. Prevalence of symptoms of cervical and lumbar stenosis among participants in the osteoporotic fractures in men study. Spine. 2006 Jun 1;31 (13):1445–1451. Yamashita K, Ohzono K, Hiroshima K. Five-year outcomes of surgical treatment for degenerative lumbar spinal stenosis: a prospective observational study of symptom severity at standard intervals after surgery. Spine. 2006 Jun 1;31(13):1484–1490. Some authors (e. g., Hülse, 1981) suggest that manual medicine treatment is indicated in those cases where the presenting cervical vertigo or reported perception of imbalance is felt to be the result of relevant structural and functional disturbances (i. e., somatic dysfunction) in the upper cervical spine. This is true particularly when it would appear that the facet joints in the upper cervical spine (C0–C1 and C1–C2 articulations) are involved. However, cervicogenic vertigo must always be clearly differentiated from other causes of vertigo, especially those not amenable to or even contraindicated for manual therapy. In 1913 Oppenheim described vertigo as an unpleasant sensation resulting from a disturbance in perception of the body in relation to its surroundings and position in space. To maintain equilibrium, or in other words to assure an intact awareness of the body in space, three sources of afferent impulses from different systems are required: the optic, vestibular, and proprioceptive systems. In addition, according to studies by Hülse (1981, 1982, 1983) and Wyke (personal communication, 1983), the receptors of the facet (apophyseal) joints in the cervical spine assume an important role in the maintenance of equilibrium. A disturbance or irritation of the receptors in the cervical spine may lead to vertigo and cervical nystagmus. Hülse (1981, 1983) describes cervical nystagmus as a sine qua non condition in patients with complaints of dizziness and findings of functional disturbances in the cervical spine (i. e., somatic dysfunction). In their experimental studies, Hikosaka and Maeda (1973) suggest that a connection exists between the facet joints and the abducens nuclei. It has been shown that impulses originating from joint receptors are transmitted to the vestibular nuclei (Fredrikson et al., 1965; Maeda, 1979). These two connections may help explain the existence of cervicogenic vertigo. At the same time, it may be difficult to differentiate between cervical vertigo and that caused by vascular abnormalities or changes in the vestibular apparatus. Various authors (e. g., Hülse, 1981) suggest that manipulative therapy is indicated in those cases where the cervical vertigo or perception of unbalance is caused by functional disturbances (i. e., somatic dysfunction) in the upper cervical spine, including the C0–C1, C1–C2 facet joints. However, this form of vertigo must always be clearly differentiated from other causes of vertigo, especially those not amenable to or even contraindicated for manual therapeutic maneuvers. A carefully performed case history is of utmost importance. One of the main tasks for the examiner is to pay particular attention to those reported symptoms that assist in the differentiation between the so-called systematic and non-systematic types of vertigo. The systematic form of vertigo is most often being encountered when the patient complains about such sensations as head and body rotation or whirling (known in the European literature as “rotary vertigo”), nonrotatory swaying or to-and-fro movements (“sway vertigo”), or up-and-down movement (“lift vertigo”). This form of vertigo is usually due to a disturbance in the vestibular system. In contrast, nonsystematic vertigo is associated with such complaints as unsteadiness, lightheadedness, and general unpleasant feeling of discomfort. During the neurological examination, particular attention should be paid to the sensory branch of the trigeminal nerve and the other more inferior cranial nerves. The patient should also be evaluated for the presence of nystagmus, including spontaneous nystagmus (Pfaltz, 1983), vestibular nystagmus by use of provocative testing, as well as postural nystagmus, and the nystagmus elicited with head positioning or induced movement (using fitted Frenzel spectacles; Hess, 1983). However, it must be emphasized, that, in association with head rotation, it is easy to mistakenly diagnose a postural nystagmus that in reality is a cervical nystagmus (Hülse, 1983). Kornhuber (1974) rejects the idea that a postural nystagmus can be caused by a disturbance in the somatosensory proprioceptors located in the C0–C1 or upper cervical spinal joints. A detailed structural and functional examination of the cervical spine is particularly indicated in patients who present with vertigo that is thought to be related to cervical joint receptor irritation. This evaluation should include a careful search for particular irritation zones as well as localized muscle changes (i. e., palpable bands) associated with potential myofascial trigger points. Radiographic evaluation includes the conventional anteroposterior and lateral views of the cervical spine. In the presence of segmental or regional joint dysfunctions, additional views should be utilized, such as the functional lateral and transbuccal anteroposterior views. It has been suggested that atlantoaxial instability may be demonstrated on functional transbuccal views. Otoneurologic studies, including electronystagmography, aid in the differentiation between peripheral and central abnormalities of the vestibular apparatus. Based on studies by Hülse (1983), electronystagmography is also very helpful in distinguishing between vascular and cervical nystagmus or vertigo. CT and MRI scans of the head and cervical spine have become very useful in the diagnostic work-up, especially when a tumor (intracranial or extracranial) is suspected. • Ménière disease: labyrinthine disease characterized by whirling or rotational vertigo, tinnitus, unilateral deafness, autonomic changes (nausea, vomiting); nystagmus is present during the acute attack. • Vestibular neuronitis (neuropathy): disturbance in vestibular function (mostly unilateral vestibular paresis) characterized by suboccipital headaches, rotatory vertigo (hours, days, weeks), autonomic symptoms (nausea, vomiting), and the feeling of unsteady gait (“off balance”); tinnitus and deafness are usually absent. • Oculomotor disorders: diplopia, possible brief sensation of vertigo accompanied by mild nausea; may be seen in persons with error of refraction (astigmatism, myopia, hyperopia). • Tumors in posterior cranial fossa: including meningioma, ependymoma. • Acoustic neuroma: loss of hearing, tinnitus, vertigo (usually of the nonsystematic type and rarely observed as initial symptom), ipsilateral ataxia of limbs, nystagmus, involvement of the trigeminal nerve (corneal reflex), increased intracranial pressure. • Ischemia (labyrinthine apoplexy): basilar insufficiency, orthostatic vertigo, usually a single precipitous attack with nausea and vomiting but without tinnitus or hearing loss. • Epilepsy due to abnormalities in the temporal cortex. • Trauma: traumatic brain injury, cervical spine trauma, including hyperextension/hyperflexion injuries to the cervical spine due to deceleration accidents. • Craniocervical malformations: basilar impressions, assimilation of the atlas. • Neurotic or psychogenic abnormalities. • Cervical vertigo. Differentiation between the proprioceptive and vascular types of cervical nystagmus is significant inasmuch as manipulative therapy is contraindicated in the vascular type due to potential complications associated with the procedure. According to Hülse (1983), proprioceptive nystagmus occurs immediately upon turning the head (i. e., there is no latent period). In contrast, the vascular type of nystagmus is usually not evident until the patient’sneck isturned to the extreme position, in which case it takes from seconds up to 3minutes to become apparent. Thus, a certain latent period is more characteristic of the vascular type of nystagmus. An additional differentiating quality is the clearly decrescendo character of the nystagmus seen with the proprioceptive type, in contrast to the crescendo character of the nystagmus observed with the vascular type. Ernst A, Basta D, Seidl RO, et al. Management of posttraumatic vertigo. Otolaryngol Head Neck Surg. 2005;132(4):554–558. Cervicogenic and tension headache are frequent reasons for medical visits, particularly to manual medicine practitioners. Tension-type headache and cervicogenic headache are two of the most common nonmigraine headaches (McCrory et al., 2001). This report, which was produced by the Duke University Evidence-Based Practice Center (EPC), concludes that with regard to cervicogenic headache manipulation is effective, while with regard to tension-type headache manipulation is unproven (based on the studies available and their methodological shortcomings, among other reasons). The same report further reports that the various behavioral therapies have modest efficacy for tension-type headache. Cervical spinal manipulation was associated with significant improvements in headache outcomes in trials involving patients with neck pain and/or neck dysfunction and headache (McCrory et al., 2001). As reported in the same monograph, compared to a placebo control, manipulation resulted in immediate improvement when used to treat a single episode of headache with posterior cervical discomfort in one trial (Hoyt et al., 1979). It is further reported that when compared to soft-tissue therapy (e. g., deep friction massage), a course of manipulation treatment resulted in sustained improvement in headache frequency and severity in patients with cervicgogenic headache (Nilsson et al., 1997). Virtually any structure in the upper cervical spine has been incriminated at some time as a potential source of headache. Neurophysiologic experiments (Kerr, 1961) have shown that stimulation of nerve roots, ligaments, periosteum, apophyseal joints, and paravertebral muscles can project pain into areas that topographically separate from a particular nerve’s innervation. By injecting hypertonic salt solution into the joint capsules of the upper cervical spine, Cyriax (1938) and Kellgren (1939) were able to show that pain may be provoked in a specific region. Dwyer et al. (1990) produced pain by injection of contrast material into the intra-articular space. Bogduk and Marsland (1986) used specific nerve blocks to investigate whether the source of the cervical headache could be attributed to the C2–C3 apophyseal joint, for instance when affected by osteoarthritis. They found that in seven out of ten consecutive patients with suspected cervical headache the pain originating from the C2–C3 joints was mediated by the third occipital nerve. The structures that may cause cervicogenic headaches are typically supplied by the dorsal rami of the cervical spinal nerves. In the lateral portion of the neck they are in proximity to the cervical plexus and the areas supplied by the ventral rami. In the head they are in proximity to the trigeminal region. The receptive field is associated with the uppermost three spinal nerves and their associated joints, the ligaments, and the vertebral motion segment as well as the anterior and posterior neck muscles, the sternocleidomastoid, and the trapezius muscles. Also, the dura of the posterior fossa and the intracranial portion of the vertebral artery may be part of the receptive field. The spinal tract descending from the medulla oblongata reaches the spinal medulla at the level C2 to C4. Fibers arising from the spinal tract terminate in the inferior portion of the fifth spinal nucleus in the upper three segments of the spinal medulla. In the spinal medulla, the terminal projections of the fibers of the spinal tract overlap those from the afferent fibers of the upper three cervical spinal nerves. Therefore, they form an overlapping region in which the individual contributions cannot be separately distinctly. This region in the gray substance of the spinal cord is thus described as the trigeminal-cervical nucleus in (Neuhuber et al., 1990). The trigeminal-cervical nucleus may be viewed as the nociceptive nucleus of the head and the upper cervical spine according to Bogduk (1992). The Swiss physician, Otto Nägeli (1843–1922) was one of the first physicians in Europe to treat headache by using specific hand applications or manipulative procedures to the cervical spine. In his text “Therapy of Neuralgia and Neurosis by Hand Application” (1894), Nägeli presented his theoretical construct concerning the development of headache in an attempt to explain the therapeutic success of his various manipulative techniques (Biedermann, 1954). At about the same time, various osteopathic physicians and chiropractors in the United States were also trying to treat headache using spinal manipulations and other hands-on techniques applied to the cervical spine. Some of the osteopathic and chiropractic techniques developed in the United States were imported into Europe where they were adopted by physicians and integrated into their medical armamentarium. This would later lead to the formation of the field of manual medicine (Cramer et al., 1990). In reviewing the osteopathic and chiropractic literature, it is readily apparent that the upper cervical spine, and in particular the various somatic dysfunctions related to it, have always been considered to be one of the clinically important regions that may lead to headache. In 1928, J. A. Barré and his student, Y. A. Lieou, coined the term “sympathetic posterior cervical syndrome.” They described a clinical presentation the symptoms of which include neck pain, dizziness, vertigo, and latent headache. They thought that the symptoms were due to irritation of the vertebral nerves. Degenerative changes that involve the uncovertebral joints in the lower cervical spine have been thought to be one of the causes of the pain due to the potential irritation of the neighboring vertebral nerves (Barré and Lieou, 1928). In 1949, Bärtschi published a text entitled “Cervical Migraine, the Encephalic Syndrome after Cervical Spine Trauma”) (Bärtschi, 1949). He described a situation in which the patient presented with headache that was similar to the classical presentation of migraine while demonstrating features that were quite different from those associated with migraine. Heyck (1982) devised four categories according to the potential source of the cervical headache in an attempt to provide an overview of the rather complex symptomatology. As with any category, there are often rather blurred borders rather than distinct groupings (Table 14.2). Sjaastad et al. (1983), who coined the term “cervicogenic headache,” made the attempt to differentiate between the presentation of classic migraine or paroxysmal hemicrania on the one hand and other types of headache. The term “cervicogenic” was specifically chosen to indicate a possible relationship between the cervical spine and the headaches. While initially there was lack of a potential physiologic correlation between headaches and an abnormality or dysfunction in the cervical spine, more recently Bogduk in his own anatomic studies concluded that a dysfunction affecting the spinal segment at C2–C3may lead to irritation of the third occipital nerve and thus may be one of the major causes of cervical headache (Bogduk and Marsland, 1986). One currently proposed explanation for cervical headache is the convergence of incoming information at the spinal and trigeminal levels (medulla level) that is being transmitted centripetally from the periphery due to inflammatory reactions or other injury-related processes. In 1983, Sjaastad and colleagues presented a clinical syndrome they termed “cervicogenic headache.” This presentation is defined as the paroxysmal occurrence of unilateral headaches with associated symptoms that are similar to those typically associated with migraine. The headaches are often precipitated or aggravated by certain neck movements and in particular seem to become more prominent after trauma (Sjaastad et al., 1983, Sjaastad, 1992).
Clinical Disorders and Syndromes of the Spine
Pain and the Spine: A Brief Overview of Approach
Assessing the Patient Who Has Spine-related Pain
Surgery or Not?
Further Reading
Nerve Roots and Nerve Root Pain
Anatomy of the Spinal Nerves
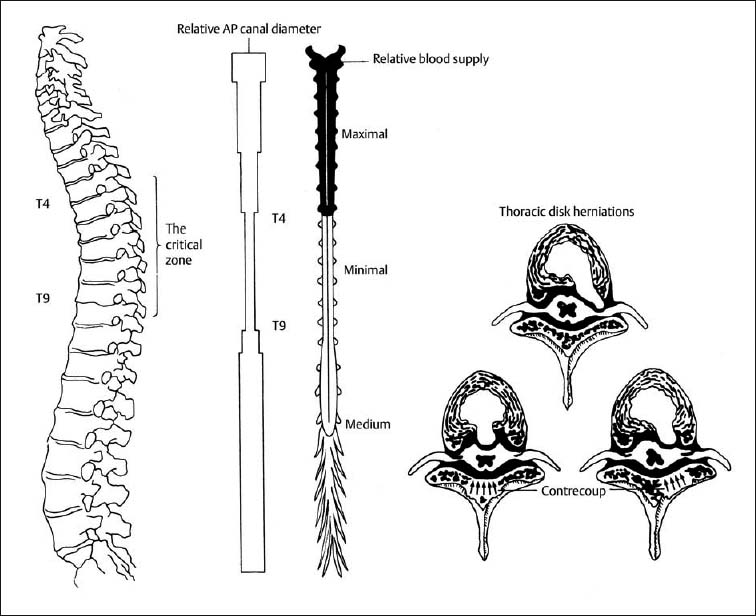
Important Radicular Syndromes
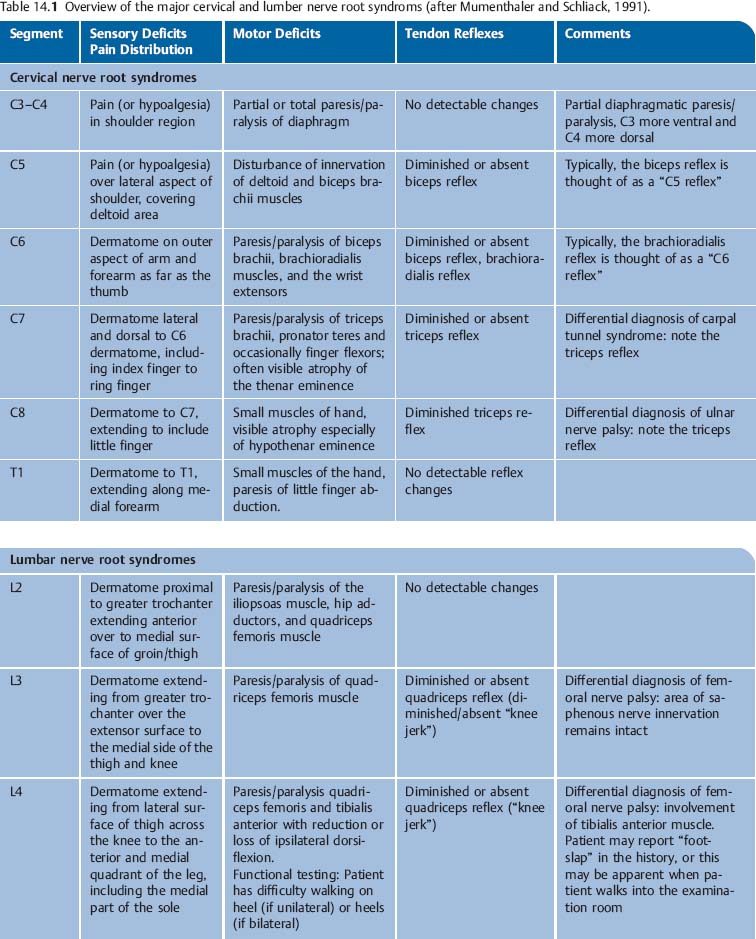
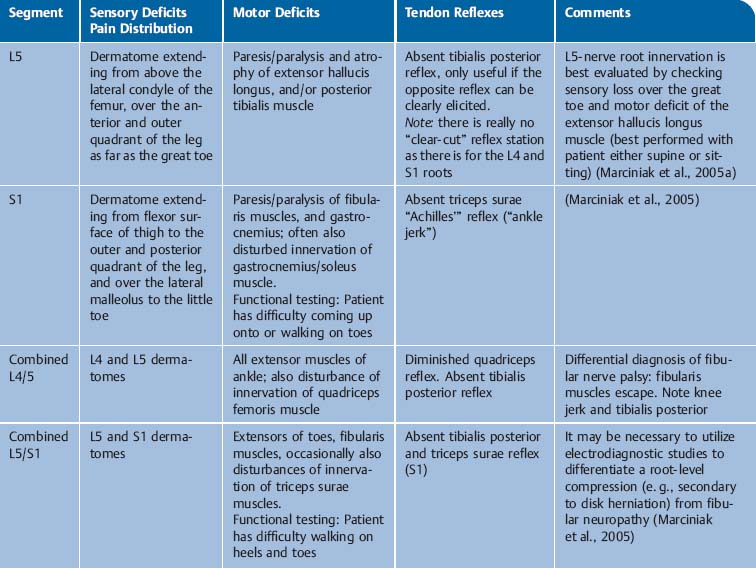
Symptomatology of Nerve Root Syndromes
Further Reading
Neurologic Disorders Associated with Back Pain
Extramedullary, Intraspinal Tumors
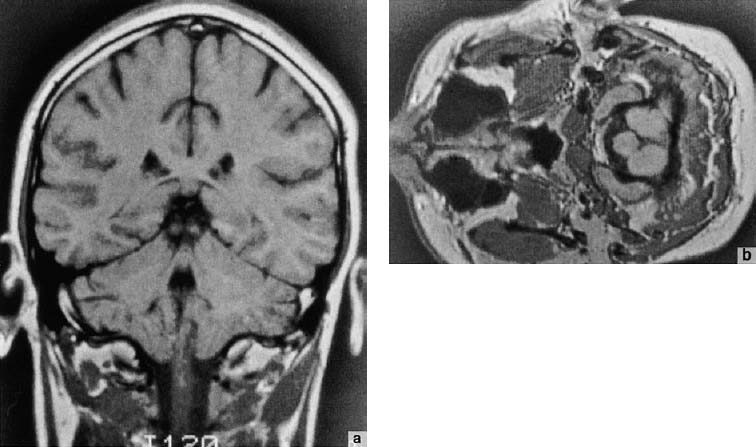
Intramedullary Space-Occupying Lesions and Syringomyelia
Metastatic Bone Disease
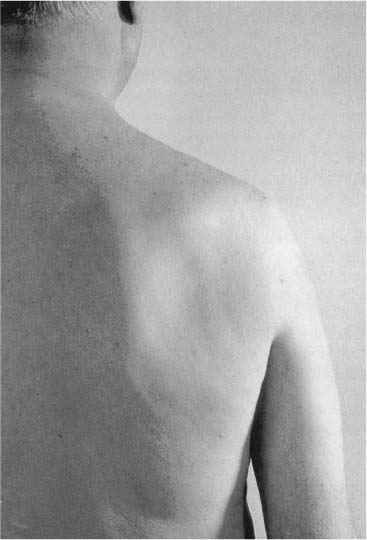
Neurogenic Amyotrophy, Neuritis, and Polyradiculitis
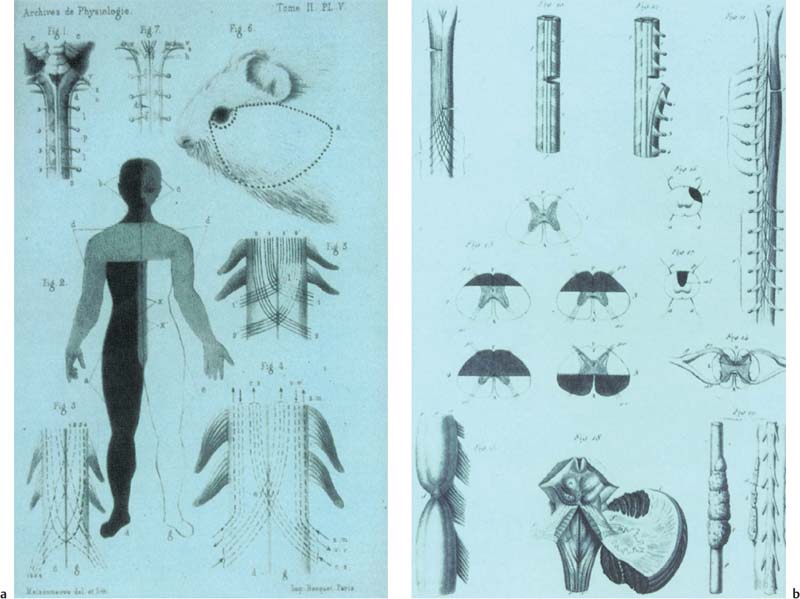
Circulatory Changes Affecting the Spinal Cord
Spontaneous Spinal Epidural Hematoma (SSEH)
Spinal Epidural Abscess
Lumbar Spinal Stenosis
Further Reading
Cervicogenic Vertigo and Headache
Sensation of Imbalance (Disequilibrium): Dizziness, a Cardinal Symptom
Differential Diagnosis of Vertigo
Examination of the Patient with Vertigo
Important Disorders Associated with Vertigo
Further Reading
Cervicogenic Headache
Anatomy
Peripheral Anatomy
Central Anatomy
Hypotheses for Cervical Headache
Clinical Presentation of Headache Associated with Cervical Syndrome
1 | Myogenic pain due to involvement of the suboccipital muscles |
2 | Neurogenic pain due to nerve root irritation of C2 and C3 Greater occipital nerve—C2 nerve root Lesser occipital nerve—C2 and C3 nerve roots Greater auricular nerve—C3 nerve root |
3 | Projected pain due to irritation of the periarterial sympathetic nerve plexus of the vertebral artery and the vertebral nerve |
4 | Venous congestion in the cervical canal |
A | Pain referred from a source in the neck, and perceived in regions of the head or face |
B | Clinical, laboratory, and/or imaging evidence of a disorder within the cervical spine or soft tissues of the neck generally accepted to be a valid cause of headache Fractures, infections, tumors, rheumatoid arthritis, or other distinct and objectively verifiable pathology (not cervical spondylosis or osteochondritis) |
C | Evidence that the pain can be attributable to the neck disorder based on one of the following: • Demonstration of clinical signs which implicate a source of pain in the neck • Abolition of headache following diagnostic blockade of a cervical structure or its nerve supply using placebo or other controls – Neck pain, focal tenderness, history of trauma, mechanical exacerbation of pain, reduced range of motion, nuchal onset, nausea, vomiting, photophobia are suggestive of but do not define cervicogenic headache |
D | Pain resolves within 3 months after successful treatment of the causative disorder |
1 | Pain localized to the neck and/or occipital region |
2 | Secondary pain may be referred to the frontal region |
3 | Characteristics of (1) and (2) above, except that the pain is unilateral |
4 | Recurrences, with each the episode lasting for quite some |
5 | Pain may be precipitated or aggravated by abnormal loading to the cervical spine secondary to postural or motion abnormalities |
6 | Either associated with or noted in the history: • Cervical spine pathology, such as torticollis, cervico-brachialgia, etc. • Cervical spine lesion (dislocation, fracture, ligamentous tears) due to trauma or extension/flexion injury, etc. |
7 | A detailed physical examination reveals the following: • Motion restriction in the cervical spine (hypomobility), or abnormally large motion (hypermobility) • Pain elicited with palpation in the cervical musculature • Radiologic findings • Congenital or acquired anomalies: trauma, bony, degenerative, functional, etc. |
8 | Other causes of occipital headache have been ruled out |
9 | Specific treatment is successful |
In 1988, the Headaches Classification Committee of the International Headache Society determined criteria for cervicogenic headaches. The criteria were recently revised in 2004 (Table 14.3). The pain is typically referred from a source in the neck, and perceived in regions of the head or face.
Mumenthaler and Regli presented their criteria for spondylogenic headache in their text “The Headache” (Mumenthaler, 1990) (Table 14.4).
Thus, over time a number of clinical characteristics have been gathered that are commensurate with headache of cervical origin. These include characteristics of pain location, temporal profile, provocative factors, associated signs and symptoms, as well as objective findings of motion restriction (hypomobility) or situations of ligamentous insufficiency (after trauma, massive degenerative processes, for instance) that result in hypermobility (Table 14.5).
Treatment of cervicogenic headaches, while apparently amenable to manual medicine intervention, may require a multimodal approach when refractory to hands-on treatment. This multimodal or multidisciplinary approach may utilize the spectrum of pharmacological interventions (e. g., NSAIDs, analgesics, tricyclic antidepressants, antiepileptics, and muscle relaxants, with awareness of their potential side-effects), and nonpharmacologic interventions such as appropriately dosed physical therapeutic intervention (preferably active-exercise-based therapy), transcutaneous electrical nerve stimulation (“TENS”; there may be benefit from an initial trial course), or biofeedback and other therapeutic behavioral treatments. If all of this fails, or concurrently, one may consider interventional care including anesthetic block, trigger point injections (this especially may be done concurrently with manual medicine procedures), botulinum toxin injections, or neurolytic interventions. The patient may be acandidate for surgical interventions in sufficiently severe cases.
1 | Pain location | Occipital Frontal Temporal and/or facial |
2 | Temporal profile | Episodic With/without each episode lasting for a prolonged period (constant pain of long duration) |
3 | Pain provocation | Movement of the head or the neck |
4 | Associated signs/symptoms | Autonomic changes |
5 | Examination findings | Motion restriction determined by a functional–structural manual medicine examination Increased muscle tone |
Further Reading
Antonaci F, Bono G, Chimento P. Diagnosing cervicogenic headache. J Headache Pain. 2006 7(3):148–148.
Biondi DM. Cervicogenic headache: a review of diagnostic and treatment strategies. J Am Osteopath Assoc. 2005;105 (4 Suppl 2):16S–22S.
Biondi DM. Noninvasive treatments for headache. Expert Rev Neurother. 2005;5(3):355–362.
Bogduk N. Headache and the neck In: Goadsby PJ, Silberstein SD, eds. Headache. Boston, MA: Butterworth–Heinemann; 1997.
Fernandez-de-las-Penas C, Alonso-Blanco C, San-Roman J, Miangolarra-Page JC. Methodological quality of randomized controlled trials of spinal manipulation and mobilization in tension-type headache, migraine, and cervicogenic headache. J Orthop Sports Phys Ther. 2006;36(3):160–169.
Frese A, Schilgen M, Edvinsson L, Frandsen E, Evers S. Calcitonin gene-related peptide in cervicogenic headache. Cephalalgia. 2005;25(9):700–703.
Hülse M, Seifert K. Cervicogenic head and neck pain [in German]. HNO. 2005;53(9):804–809.
McCrory DC, Penzien DB, Hasselblad V, Gray RN. Evidence report: behavioral and physical treatments for tension-type and cervicogenic headache. Des Moines (IA): Foundation for Chiropractic Education and Research; 2001. Product No. 2085.
Zito G, Jull G, Story I. Clinical tests of musculoskeletal dysfunction in the diagnosis of cervicogenic headache. Man Ther. 2006;11(2):118–129.
Degenerative Disorders of the Spine
The neuromusculoskeletal evaluation and treatment of the patient presenting with spine-related pain, and in particular when there are degenerative changes, should always be tailored to the individual presentation and particular patient needs. The approach takes into account all of the objectively verifiable and functionally meaningful parameters that can be determined in detailed history and a thorough physical examination that is then expanded by a targeted structural–functional examination (manual medicine assessment).
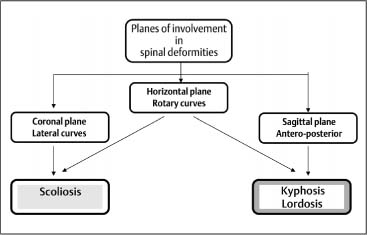
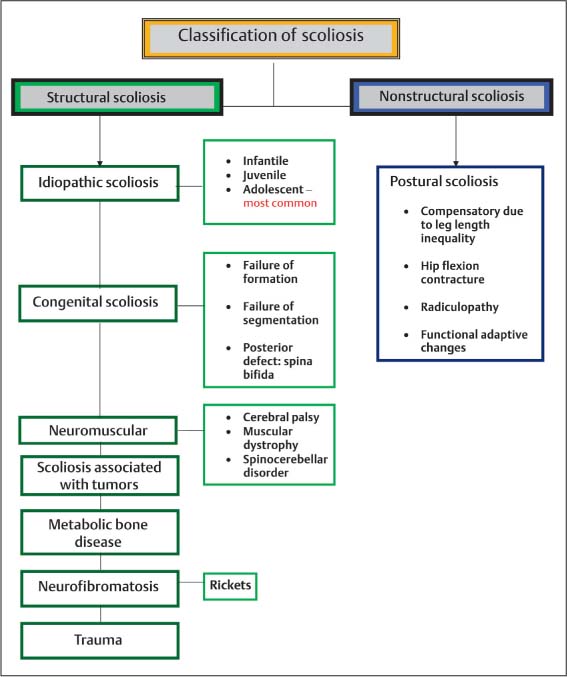
For instance, the examination of an adolescent spine directs the history and the examination in one clinical direction (e. g., scoliosis), while that of an octogenarian spine would emphasize different directions (e. g., degenerative changes, spinal stenosis, metabolic disorders, space-occupying lesions).
Standard radiographic studies have some, albeit limited, usefulness. It is well known that radiographic findings, as well as CT and MRI findings, often do not correlate well with a patient’s painful presentation. Severe degenerative changes may be noted in diagnostic studies in a patient who has virtually no pain, and vice versa. The literature has thus far not been able to explain this common phenomenon satisfactorily.
The manual medicine approach to a patient with known spondylotic changes follows a rational sequence of first eliminating any sinister pathology (“red flags”), while the management addresses structural and functional changes as elicited in the detailed work-up. The goal of the manual medicine assessment and treatment is not to “correct” a single “lesion” or “joint blockage,” rather it wants to determine the relevance of the various motion and tissue restrictions within the entire clinical presentation. The evaluation of fascial restrictions and of the different muscles as being short (e. g., tonic muscles, type I muscles) or being weak (e. g., phasic muscles, type II muscles) takes on an important role. Furthermore, while localized findings in one particular region may be quite prominent, the detailed manual medicine assessment investigates the influence of such local findings on other regions, as one can rather quickly observe adaptive and compensatory changes in regions quite distant from the original area of dysfunction (e. g., neck pain resulting from lumbosacral or pelvic aberrations).
With respect to manual medicine maneuvers performed on patients with spondylotic changes, the distinction must be made between performing high-velocity/low-amplitude thrusting maneuvers (“thrust,” or manipulation-with-impulse maneuvers) and the non-thrusting techniques (mobilization-without-impulse techniques, e. g., soft-tissue techniques, among others). The manipulative techniques that involve high-velocity/low-amplitude thrusting (referred to by some authors as “spinal manipulative therapy,” or SMT) have been subject to considerable intra- and interprofessional discussions and varied interpretations and conclusions (Haldeman et al., 2002; Malone et al., 2002); more studies, especially large population-based studies are needed to comprehensively address the multifactorial influences involved in the topic.
Further Reading
Daffner SD, Hilibrand AS, Hanscom BS, et al. Impact of neck and arm pain on overall health status. Spine. 2003;28(17):2030–2035.
Ratliff JK, Cooper PR. Cervical laminoplasty: a critical review. J Neurosurg. 2003;98(3 Suppl):230–238.
Roh JS, Teng AL, Yoo JU, et al. Degenerative disorders of the lumbar and cervical spine. Orthop Clin North Am. 2005; 36(3):255–262.
Metabolic and Rheumatologic Disorders Affecting the Spine
Four major metabolic subsets involving the spine include osteoporosis, osteomalacia, Paget disease, and proximal motor neuropathy.
Osteoporosis
Osteoporosis may be best defined as normally calcified but quantitatively deficient bone that has resulted in clinical disability. The generalized loss of bone mass is typically asymptomatic. However, when sufficiently severe, it often results in painful fractures that draw attention to the underlying problem. The most common areas of increased risk for fracture include the hip, the distal radius (Colles’ fracture), and the vertebrae, especially in the thoracic spine.
The etiology is known to be multifactorial, but the outstanding feature is an imbalance between bone formation and resorption, in favor of the latter. Thus new bone is not formed to the same extent as in the normal, healthy situation, resulting in a decrease in bone mass secondary to bone loss.
Causative factors implicated in osteoporosis are immobilization, estrogen reduction as occurs during menopause, hyperparathyroidism, calcium deficiency, and corticosteroid use.
Pain is typically not one of the presenting signs for a patient with osteoporosis until a fracture has occurred. Conversely, it should be remembered that vertebral compression fractures may have actually been present for quite some time before they become symptomatic.
Prolonged periods of immobilization quite readily lead to substantial loss of bone mass. This should always be kept in mind when dealing with forced immobilization after the patient has had a stroke, spinal cord injury, or fracture, for instance. During the immobilization period, dramatically more bone is being resorbed than is being produced. Up to 40% of the initial bone mass can be lost when a person is immobilized for 6 months. This, therefore, leads to greater risk of spontaneous fractures. After about 6 months, however, it seems that a new homeostatic balance is reached.
Clinical Examples
An elderly patient may lose as much bone mass within one month of immobilization as the typical bone loss that occurs over one year in an otherwise healthy person.
If a patient has been subjected to a prolonged period of immobilization, they may have lost an amount of bone mass that could not be restored to the pre-injury level even if mobility were to be fully restored. The major criterion for reversibility is the degree to which the trabeculae have been destroyed. In younger patients, osteoporosis may be reversible as long as the trabeculae have not been entirely resorbed.
Presenting Signs and Symptoms
In general, osteoporosis is not painful; it is the occurrence of a fracture or several fractures that presents with notable pain. In a patient with progressive osteoporosis, only a small amount of trauma is necessary to cause a fracture. It is known that once a fracture has occurred, there is a greater chance of additional fractures in other vertebrae. A stable vertebral fracture in the absence of nerve root compression typically heals within 3 months.
From a manual medicine perspective, one would want to know whether a vertebral fracture due to osteoporosis is a stable or an unstable fracture. Additionally, one should remain vigilant for occult fractures and should not assume that every vertebral fracture in the presence of osteopenia is due only to osteoporosis. These points can be evaluated with good radiographic studies. Frequently they can only be resolved by the use of CT or MRI. Indications for CT include the presence or suspicion of vertebral cord compression or pain of unknown source, especially when there has been what would be considered adequate therapy, which might include the use of the a three-point corset and appropriate analgesics. Indications for MRI include suspicion of occult fracture due to malignancy, spinal cord myelopathy, or radicular nerve root compression.
Again, it is emphasized that a patient who is known to have an osteoporotic process may have an increased risk of further bone mass loss due to immobilization. This may require the utilization of calcitonin or bisphosphonates, whose action if thought to be as bone resorption blockers.
DEXA (dual-energy roentgen ray absorptiometry) is a useful study for determination of the patient’sosteoporotic status.
Cummings (Cummings et al., 1993) demonstrated that individuals who are between 20 and 40 years old, and whose bone density value is one standard deviation below the average value for their age group, are at two to three times the risk of sustaining a fracture. The same study also observed a direct correlation between bone density and the ability to withstand mechanical stress.
From a manual medicine perspective, it is important to recall that when pain is elicited over the spinous process with palpatory percussion, one’s suspicion should be raised for the presence of osteoporotic vertebral fracture. As long as the provocation pain upon percussion remains over the spinous process of a vertebra that has sustained a fracture, one may assume that the vertebral fracture has not completely healed. In particular, mobilization techniques with impulse (thrusting or high-velocity, low-amplitude impulse) to the site of vertebral fracture involvement are contraindicated unless there are other intervening factors that enter the overall clinical situation. These should be clearly documented.
Osteomalacia
Osteomalacia is a disorder of bone metabolism characterized by a faulty process of mineralization of the organic matrix.
Associated etiologies include malabsorption-related vitamin D deficiency, renal and hepatic disease, and abnormalities in calcium and phosphorous mineralization.
In contrast to osteoporosis, nearly 90% of patients with osteomalacia experience back pain, along with pain in the long bones of the legs and the ribs. There is palpatory tenderness and the patient may present with a readily recognizable waddling gait. Laboratory studies reveal elevated alkaline phosphatase in the majority of patients. Nearly half of the patients have hypocalcemia and hypophosphatemia. Treatment involves the use of vitamin D supplements.
Differential diagnosis includes osteoporosis and tumors including multiple myeloma.
Paget Disease
Another metabolic bone disorders Paget disease, also known as ostitis deformans, is characterized by abnormally high bone resorption while at the same time the bone formation is disorganized. Even though the bone is enlarged in the individual with Paget disease, it is functionally weak. The bone is prominently vascularized.
Paget disease increases with age. Men are involved twice as frequently as women. Approximately 3% of men over the age of 50 are reported to have Paget disease, and its incidence triples to 10% in the cohort of men older than 80 years of age.
The distribution of the various skeletal regions is as follows:
• Sacrum 56%
• Spine 50%
• Femur 46%
• Skull 28%
• Sternum 23%
• Pelvis 22%
• Clavicle 13%
• Ribs 7%
There is typically multilocation involvement of different bones in the Paget disease patient.
The patient with Paget disease is usually asymptomatic. However, when presenting to the office with pain, the patient as a rule reports it as a deep, aching type of pain that is constant rather than fluctuating. Back pain is present in about 10–30% of patients. There are often associated deformities including an enlarged skull, bowing of the legs, and spinal abnormality due to weakening of the bone itself. While spinal cord compression has been reported to occur, especially in the hypertrophic form, it is relatively rare.
The most critical region is the thoracic region where the spatial spinal canal–spinal cord relationships are tightest. The enlargement of the vertebral bodies, especially the vertebral arch and the articular facets, may lead to intervertebral foraminal narrowing and nerve root compression that may present as a neurogenic claudication.
It should be noted that secondary osteoarthritic changes of the facet joints may cause articular pain that is resistant to treatment due to the plastic deformation of the bone. Often the pain is exacerbated when the patient performs simultaneous extension and rotation movements. In addition to carefully applied manual medicine treatment, medical treatment including the use of bisphosphonates and/or calcitonin should be utilized.
Proximal Motor Neuropathy
Proximal motor neuropathy due to diabetic polyradiculopathy or diabetic amyotrophy is another metabolic disorder that may be seen in a spine clinic. This typically occurs in patients older than 50 years and is associated with a recent onset of type II diabetes. As with Paget disease, men seem to be more commonly affected.
The hallmark of presentation for a patient with proximal motor neuropathy is that of bilateral or unilateral lower limb pain that may actually resemble or mimic that of sciatica. The pain is usually worse at night. The patient may report spontaneously that she or he has difficulty climbing and managing stairs. Upon examination there is notable proximal upper muscle weakness and muscle wasting may be noted during the examination.
The primary goal of treatment is to address the underlying disorder of glucose metabolism.
Further Reading
Argoff CE, Backonja MM, Belgrade MJ, et al. Consensus guidelines: treatment planning and options. Diabetic peripheral neuropathic pain. 1: Mayo Clin Proc. 2006 Apr;81(4 Suppl): S12–25. [Erratum: Mayo Clin Proc. 2006 Jun;81(6):854].
Hosking D. Pharmacological therapy of Paget’s and other metabolic bone diseases. Bone. 2006 Feb;38(2 Suppl 2):S3–7. [Epub ahead of print 2006 Jan 10].
Lespessailles E, Prouteau S. Is there a synergy between physical exercise and drug therapies for osteoporosis? Clin Exp Rheumatol. 2006 Mar–Apr;24(2):191–195.
Licata AA. Discovery, clinical development, and therapeutic uses of bisphosphonates. Ann Pharmacother. 2005 Apr; 39 (4):668–677.
Sambrook P, Cooper C. Osteoporosis. Lancet. 2006 Jun 17;367(9527):2010–2018.
Seeman E, Delmas PD. Bone quality—the material and structural basis of bone strength and fragility. N Engl J Med. 2006 May 25;354(21):2250–2261.
Rheumatologic Disorders
Seronegative Spondyloarthropathy
The seronegative spondyloarthropathies (SNSAs), represent a group of arthritides that, while lacking the antibodies for rheumatoid arthritis in the serum (hence “seronegative”), are inflammatory in nature. Representatives include such entities as ankylosing spondylitis (Bechterew disease), psoriatic spondyloarthropathy, and Reiter syndrome. The involvement is typically that of the spine (hence “spondylo-”), the sacroiliac joint, and other bones. The pain at the long bone is typically due to an inflammatory response at the attachment of muscle to bone, the region of the enthesis. Thus, enthesitis is not uncommon in this group of disorders. Although the HLA-B27 antigen (see below) has been used as the mainstay of laboratory examination, conventional radiographs of the lumbosacral spine have remained the imaging investigation of choice. However, it has recently been reported that standard radiographs are unable to detect early inflammatory changes of sacroiliitis, potentially delaying the establishment of the appropriate diagnosis, which may therefore require employment of additional radiographic modalities (MRI) as early as possible (Grigoryan et al., 2004).
The only laboratory marker is the presence of the HLAB27 gene. There is strong correlation of the laboratory finding of the HLA-B27 gene marker with the various spondyloarthropathies. Currently, there are seven subtypes known of the HLA-B27 gene. However, the gene marker is not required for diagnosis.
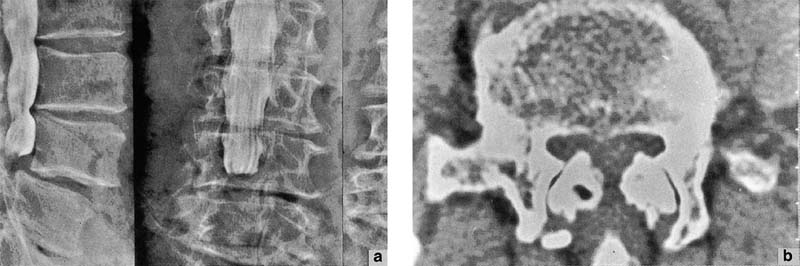
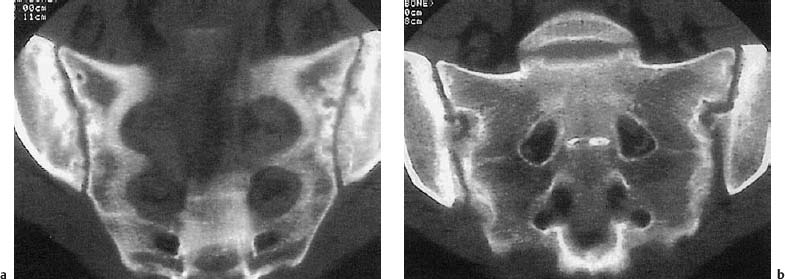
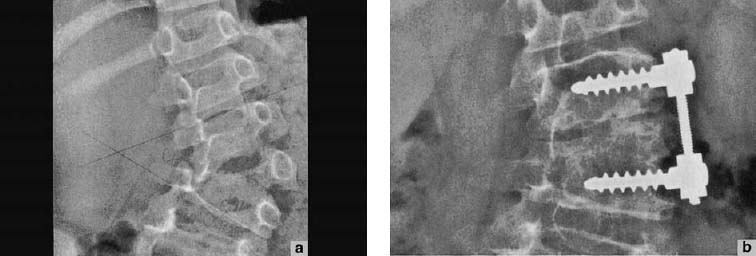
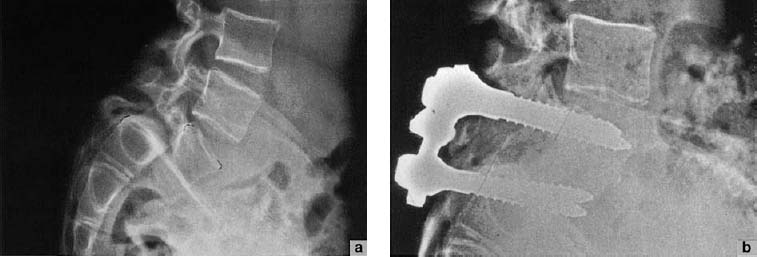
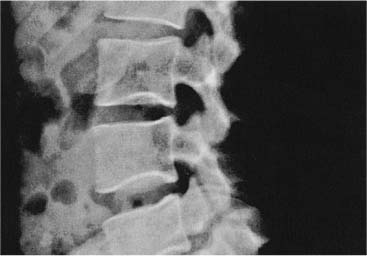
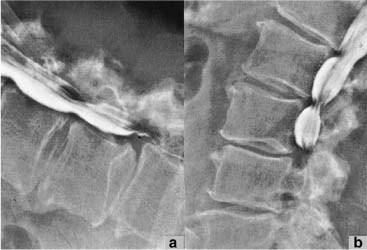
Typically, the seronegative spondyloarthropathies are diseases of the young person as the initial presentation is often between the 25th and 40th year of life. The patient typically reports early morning pain in the sacroiliac joint region associated with morning stiffness of the spine. The diagnosis is primarily clinical, with appropriate laboratory studies to exclude other rheumatologic or autoimmune diseases. The work-up may additionally require the appropriate use of radiographs, CT scan, and other diagnostic imaging studies, especially when the diagnosis is uncertain (Grigoryan et al., 2004). The standard radiographs include films of the sacroiliac joint as well as of the lumbar spine (Fig. 14.11).
The clinical presentation of the seronegative spondyloarthropathies is characterized by low back pain and morning stiffness. The average age of the initial manifestation of the disease is 26 years. Men are affected by SNSA three times more often as women (Table 14.6).
The physical examination concentrates on the mobility of the spine in general and the segmental or vertebral mobility, and includes the measurement of thoracic cage excursion. If the thoracic excursion is less than 3cm between the extremes of inhalation and exhalation, this may be an indication for further work-up with regard to SNSA.
Fig. 14.11a, b CT of the sacroiliac joint revealing degenerative changes and “bridge-formation.”
Acute sacroiliac joint arthritis or acute spondylodiscitis is often associated with prominent percussion pain over the incriminated sacroiliac joint or the incriminated vertebrae.
Complications of SNSA include spinal fracture and/or dislocation, cauda equina syndrome, or osseous ankylosis of the spine resulting in an abnormal posture.
While manual medicine treatment is not expected to alter the underlying pathophysiology in the SNSA patient, careful application of hands-on techniques should address the associated secondary adaptive or compensatory changes locally and distally. The goal of the manual medicine treatment is that of restoring as much mobility as possible while designing an individually tailored exercise program for the patient to encourage their own active program.
Disseminated Idiopathic Skeletal Hyperostosis (DISH; Forestier Disease)
Disseminated idiopathic skeletal hyperostosis (DISH), also known as Forestier disease, is considered a variant of osteoarthritis or osteoarthrosis. The hallmark is the presence of significant ossification of the spinal ligaments while there is surprisingly little pain.
This is a chronic disorder of the connective tissue of the body in the musculoskeletal apparatus, affecting up to 10% of men and 8% of women over the age of 65 years. The ossification of the ligaments in the spine and the joints results in prominent stiffening of the spine with notable reduction in mobility. While stiffness is prominent feature in both the seronegative spondyloarthropathies and the DISH syndrome, pain is relatively uncommon in the DISH population. The DISH syndrome correlates well with a diminished glucose tolerance test (17–60% of all patients with DISH syndrome) but also with adiposity. However, it appears that the glucose tolerance and adiposity are independent factors in relationship to the DISH syndrome. A clear correlation between the severity and duration of hyperglycemia and radiologic findings has not been demonstrated. Also, there is no correlation between juvenile diabetes and the DISH syndrome.
Skeletal involvement Spine • Sacroiliac joint involvement/spondylitis (90%) Arthritis of the joints • Shoulder girdle and pelvic girdle (25%) • Peripheral joints—rare • Enthesopathy |
Nonskeletal structures • Acute anterior uveitis (25%) • Cardiac involvement (1–4%) • Pulmonary involvement (less than 1%) • Amyloidosis (less than 1%) |
The DISH syndrome is not associated with the HLA-B 27 antigen, but the advanced stage of the DISH patient is closely resembles that of the patient with ankylosing spondylitis.
From a manual medicine standpoint, it is not expected that hands-on application would alter the underlying pathophysiology directly. Nonetheless, the manual medicine evaluation and treatment should concentrate on both the primary as well as the secondary changes and adaptive compensatory alterations in the regions directly involved or distant so as to minimize energy expenditure due to the higher demand secondary to the compensatory changes.
Polymyalgia Rheumatica
Polymyalgia rheumatica is a is a relatively common disease in middle-aged and older persons that generally runs a self-limited course (Chuang et al., 1982).
The initial presenting symptoms include proximal shoulder and hip girdle pain that is typically associated with stiffness. According to Bird et al. (1979) the seven most valuable criteria for differentiation were bilateral shoulder pain or stiffness, onset of illness of less than 2 weeks’ duration, initial ESR greater than 40 mm/h, duration of morning stiffness exceeding 1 hour, age 65 years or more, depression and/or weight loss, and bilateral tenderness in the upper arms. The diagnosis is made upon confirmation by a significant elevation of the sedimentation rate. The disorder is responsive to low-dose prednisone.
A recent review comparing the sensitivity of the various parameters (Bird et al., 2005) suggests that criteria proposed by Bird et al. (1979) or Hunder and Bunch (1982) should be used whenever possible.
Women are affected more frequently than men. Various etiologies have been proposed, but no specific etiologic factor has been identified.
The patient complains typically of pain affecting the shoulder and neck, upper and lower back, and buttocks. There may be a report of thigh pain and particularly morning stiffness is often pronounced. Tenderness is typically elicited in the soft tissues upon palpation. Potential complications include giant-cell arteritis (temporal arteritis), especially if untreated. A detailed history may reveal recent headaches or visual disturbances.
From a manual medicine standpoint it is important to proceed carefully in the diagnostic palpatory assessment as patients frequently report pain upon palpation. Thus a thorough explanation of the examination procedure may be helpful. A hands-on approach is not expected to alter the underlying etiology but may be able to address early any potential compensatory or adaptive movement patterns or abnormalities associated with the patient’s use of alternative muscle groups for moving about, as when getting up from a chair or ambulating.
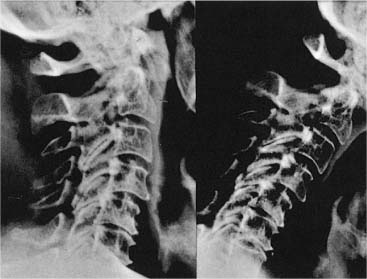
Fig. 14.12 Lateral radiograph demonstrating numerous manifestations of rheumatoid arthritis in the cervical spine.
Rheumatoid Arthritis
Rheumatoid arthritis may be difficult to diagnose in the spine especially in the early stages. A detailed review of the differential diagnostic approach to a patient with rheumatoid arthritis would be beyond the scope of this text, but a specific review in relation to manual medicine approaches is indicated. The use of manual medicine techniques in a patient with rheumatoid arthritis affecting the spine requires particular attention and care.
Juvenile chronic arthritis rarely starts with an initial presentation involving the cervical spine. However, this changes drastically as the disease progresses, and as soon as 5 years after the onset of the disease, 40% of children with juvenile chronic arthritis show involvement of the cervical spine (Ansell, 1980).
The different forms and degrees of subluxation, translation, and overt dislocation in the cervical spine, including basilar compression, account for the many different neurologic presentations. In a meta-analysis of 1749 patients, Casey (1995) reports that 32% of patients with rheumatoid arthritis have demonstrated atlantoaxial instability; 17% of the study population presented with neurologic deficits (Fig. 14.12). In association with the findings of localized instability, there is development of significant arthritic degeneration noted in the involved region of the cervical spine, which in and of itself may then lead to significant pain. (Fig. 14.13).
Fig. 14.13 Lateral radiograph of the upper cervical spine that demonstrates a significant atlantoaxial arthrosis in this 65-year-old man with known history of chronic polyarthritis.
The indication for spondylodesis is the presence of cervical myelopathy. Conclusive demonstration of a cervical myelopathic process may require the use of evoked potentials as this may currently be the only way to demonstrate the neurologic involvement early. Clinical signs of myelopathy such as atrophy of the intrinsic muscles may be difficult to assess, especially in the patient with rheumatoid arthritis who may already have the associated degenerative changes involving the joints and muscles secondary to the polyarthritis.
An important sign for myelopathy is the L’hermitte sign. Sudden “electric” pain with jerky motions that involve the entire the body should be considered a sign of compression myelopathy. The Hoffman test may also be useful.
Patients who suffer from rheumatoid arthritis typically develop osteoporosis concurrently. This may be due to non-use atrophy associated with prolonged bed rest or secondary to long-term corticosteroid use.
Manipulation with impulse in particular should not be employed in a patient with demonstrated rheumatoid arthritis in the cervical spine because of the potential risks of injury. Each treatment should be individualized, especially those consisting of soft-tissue techniques, and the patient should be examined neurologically prior to such application.
Fibromyalgia
Fibromyalgia (FM) evokes rather controversial opinions. There are essentially two major camps with a considerable spectrum spanning between these two opposing views. One group affirms its belief that such an entity as FM does indeed exist, while the other group does not believe in this diagnosis at all. Despite these varying opinions, and following best current evidence, it is recommended to apply a stepwise approach that consists of education, certain medications, appropriately dosed exercise, and cognitive therapy, or a combination of these (Goldenberg et al., 2004).
Fibromyalgia is defined as a chronic, difficult-to-treat, and often therapy-resistant generalized musculoskeletal pain syndrome with pain throughout the body. There is often associated fatigue, muscle and joint stiffness, and reports of paresthesias as well as the patient’s perception of swelling, and reproducible tender points on physical examination.
According to the late Allen Barbour, it is useful to have a name for every functional syndrome, for communicating both with patients and with other doctors. He believed “fibromyalgia” to be a good name for the kind of diffuse pain associated with it (Barbour, 1995). However, in the naming of a syndrome, no matter how organically focused and even if the name might imply a certain pathophysiologic insight (Hadler, 1986), the name itself (in this case fibromyalgia), should not serve as a substitute for trying to understand the person with a functional disorder (Barbour, 1995).
The diagnosis of fibromyalgia often depends on the point of entry of the patient into the medical system. For instance, if the patient is seen by a rheumatologist, the initial diagnosis may be just that of fibromyalgia. If the patient enters the system through psychiatry, the patient may be diagnosed with a chronic sleep disorder or chronic fatigue syndrome with a pain component. Thus, the treatment of patients who have widespread total body pain can be challenging, both in the diagnostic and therapeutic arenas.
For the manual medicine practitioner, this becomes important as he or she is often consulted as a matter of “last resort” after many and various other specialties have been visited and revisited and multiple diagnostic tests have already been performed, typically without specific findings that would be able to explain or “prove” the patient’s generalized pain. The pain symptoms might have started in one location, especially in the cervical spine and shoulder region, and then may develop to a diffuse pain syndrome involving the entire body (Goldenberg, 1987).
Patients typically report continued fatigue even if they have received what appears to be a sufficient amount of sleep of as much as 8–10 hours per night.
More than 50% of fibromyalgia patients complain of headaches.
Clinical examination comes up with very few systemic findings or abnormalities and patients may have had a number of advance studies including very rarely utilized laboratory studies in the futile hope of determining one “pain-generating” entity.
One finding that has been utilized as a standardized type of approach is the evaluation for so-called fibromyalgia tender points. If 11 of 18 circumscribed points are present, the patient can be diagnosed with fibromyalgia (Wolfe et al., 1990). The examination should be performed with the thumb and no more than 4 kilograms (8.8 pounds) of pressure (Table 14.7).
Note: There are 18 points of which the following 9 are symmetrical points. Typically the diagnosis is made on the basis of 11 findings out of the 18 points • Occiput: Bilateral at the insertion of the suboccipital muscles • Lower cervical spine: Bilateral at the anterior margin of the transverse process between C5 and C7 • Trapezius: Bilateral at the mid portion of the muscle at the upper margin • Supraspinatus muscle: Bilateral at the origin at the scapula (or close to the medial angle) • Second rib: Bilateral at the costochondral junction • Lateral epicondyle: Bilateral, 2 cm distal to the epicondyle • Gluteal muscle: Bilateral at the upper outer quadrant of the buttock • Greater trochanter: Bilateral posterior to the trochanter minor • Knee: Bilateral in the region of the medial subcutaneous fat pad approximately one hand-width proximal to the medial joint space |
There has been significant controversy in the literature and practice of pain management. A concise history of fibromyalgia is presented by Inanici and Yunus (2004). They point out that the original term fibrositis was coined by the British neurologist Gowers over a hundred years ago (Gowers, 1904), and was changed to the descriptive term “fibromyalgia” in the 1970s, whereby Smythe (1972) is identified as the “grandfather of modern fibromyalgia syndrome (FMS) (Inanici and Yunus, 2004).
However, it is important for the manual medicine practitioner that while the etiology and pathophysiology of the fibromyalgia may remain unclear, there may be concurrent findings of somatic dysfunction and/or myofascial pain syndrome in the form of a regional pain syndrome superimposed on the fibromyalgia. Careful examination is indicated to determine the extent and relevance of such findings.
Differential diagnostic evaluations would include the following:
• Polymyalgia rheumatica.
• Myositis.
• Hypothyroid disease.
• Neuropathies.
• Systemic lupus erythematosus.
• Rheumatoid arthritis.
There has been correlation with psychosomatic disorder in up to 25–60% of patients, but it is not clear what is “the chicken or the egg.”
Further Reading
Arnold LM, Lu Y, Crofford LJ, et al. A double-blind, multicenter trial comparing duloxetine with placebo in the treatment of fibromyalgia patients with or without major depressive disorder. Arthritis Rheum. 2004;50:2974.
Bennett RM, Kamin M, Karim R, Rosenthal N. Tramadol and acetaminophen combination tablets in the treatment of fibromyalgia pain: a double-blind, randomized, placebo-controlled study. Am J Med. 2003;114:537.
Braun J, Baraliakos X, Godolias G, Bohm H. Therapy of ankylosing spondylitis—a review. Part I: Conventional medical treatment and surgical therapy. Scand J Rheumatol. 2005; 34(2):97–108.
Fitzcharles MA, Esdaile JM. The overdiagnosis of fibromyalgia syndrome. Am J Med. 1997;103(1):44–50.
Frank AO, De Souza LH, Frank CA. Neck pain and disability: a cross-sectional survey of the demographic and clinical characteristics of neck pain seen in a rheumatology clinic. Int J Clin Practice. 2005;59(2):173–182.
Hakkinen A, Neva MH, Kauppi M, et al. Decreased muscle strength and mobility of the neck in patients with rheumatoid arthritis and atlantoaxial disorders. Arch Phys Med Rehabil. 2005;86(8):1603–1608.
Holden W, Orchard T, Wordsworth P. Enteropathic arthritis. Rheum Dis Clin North Am. 2003;29(3):513–530.
Keitel W. Backache from the internal medicine-rheumatologic viewpoint [In German]. Z Ärztliche Fortbildung (Jena). 1997; 90(8):671–676.
Nash P, Mease PJ, Braun J, van der Heijde D. Seronegative spondyloarthropathies: to lump or split?. Ann Rheum Dis. 2005;64(Suppl 2):ii9–13.
Smythe HA. Rheumatologists and neck pain. Scand J Rheumatol. 2000;29(1):8–12.
Organ-related Pain and Pseudo Spine Pain
Organic pain is pain that arises from the viscera or other hollow or solid body structures and that may cause either diffuse or specific pain, and pain of varying characteristic presentations from “colicky” to “lancinating.” Within the sequence of a detailed work-up of a patient presenting with the pain initially, these organic sources should be sought in order to rule out any “red flags” as the goal is to diagnose sinister pathology as early as possible.
The pain presentation can be categorized in a number of ways, but using an organ systems classification is relatively straightforward way to approach a patient whose presentation points into the realm of organic disease.
Organ System | Disease State | Comments |
Cancer and entire body system | Pain that is related to different types of cancer (% indicates the percentage presentation of pain for the particular type of cancer. Example: 85% of patients who have bone cancer report pain) • Bone (ca. 85%) • Oral cavity (ca. 80%) • Genitourinary (ca. 78% female and 75% male) • Breast (ca. 50%) • Lung (ca. 45%) • Gastrointestinal (40%) • Lymphoma (20%) • Leukemia (5%) | There is a rather wide range of pain incidence for various types of cancer, but note that nearly half of the cancer patients do have pain. Patients with lymphoma and leukemia, however, have statistically a lower incidence of pain (Foley, 1985) Bone involvement is almost always painful and is responsible for most presentations to pain clinics (Kelly and Payne, 1995) |
Cardiovascular system | • Abdominal aneurysm • Angina • Aortic aneurysm • Myocardial infarction obliterating arteriosclerosis | Abdominal aneurysm: • Abdominal pain which may range from asymptomatic to the “worst ever” • 10% of patients with abdominal aneurysm have low back pain |
Gastrointestinal system | • Cholecystitis • Duodenal ulcer • Irritable bowel syndrome • Pancreatitis | Penetrating or perforating ulcer: • May mimic acute pancreatitis • Is associated with back pain Pancreatitis is associated with: • Acute mid-epigastric abdominal pain • Radiating through to the back in up to 90% of patients |
Genitourinary system | • Cystitis • Nephrolithiasis • Prostatitis | Bacterial prostatits: • Associated with fevers • Associated with low back pain and/or perineal pain Nephrolithiasis: • Flank pain |
Gynecologic system | • Endometriosis • Pelvic inflammatory disease • Ectopic pregnancy | Endometriosis: • One-fourth to one-third of patients have back pain Ectopic pregnancy: • Abdominal pain; may mimic upper lumbar radiculopathy with radiation to the thighs |
Respiratory system | • Pulmonary embolism • Pneumonia |
|
When the patient describes back and/or leg pain as the presenting symptom of an underlying systemic disease, it is often referred to as pseudo spine pain (Mazanec, 2003). The same author reminds us that the recognition of conditions associated with pseudo spine requires an appreciation of key extraspinal diagnostic clues in the appropriate demographic setting.
A summary overview is presented in Table 14.8, adapted from Mazanec (2003).
Further Reading
Heary RF, Bono CM. Metastatic spinal tumors. Neurosurg Focus. 2001;11(6):e1.
Hosono N, Ueda T, Tamura D, et al. Prognostic relevance of clinical symptoms in patients with spinal metastases. Clin Orthop Relat Res. 2005; (436):196–201.
Lu C, Gonzalez RG, Jolesz FA, et al. Suspected spinal cord compression in cancer patients: a multidisciplinary risk assessment. J Supportive Oncol. 2005;3(4):305–312.
Ross MD, Bayer E. Cancer as a cause of low back pain in a patient seen in a direct access physical therapy setting. J Orthop Sports Phys Ther. 2005;35(10):651–658.
Orthopedic Spinal Disorders
Congenital Malformations of the Spine: Spinal Dysraphism
It should be remembered that spinal malformations do not necessarily present with pain. For instance, a block vertebra in the cervical spine associated with a Klippel–Feil malformation may present with no symptoms at all (Patel et al., 1995) and is often found as an incidental finding during radiologic studies.
Congenital deformities of the spine due to spinal dysraphism (from Greek meaning defective fusion of a raphe, in particular the neural folds) and are associated with neural tube defects represent a group of congenital spinal anomalies that result from failure of fusion of the neural tube early in fetal life. The anomalies in this group include such entities as meningocele, myelomeningocele, myelocele, spina bifida cystica and occulta, tethered cord, diastematomyelia, diplomyelia, and others. As in spina bifida, the malformations may range from minor abnormalities (e. g., spinal bifida occulta) to lesions that are incompatible with survival. Most cases of spina bifida occulta (as the name implies) are not detected until they are recognized serendipitously on routine radiographic examination.
Widening of the spinal canal in the cervical spine in the craniocervical junction may require further work-up due to the potential presence of an Arnold–Chiari deformation in this region (Fig. 14.14a, b).
Incidental findings of an abnormal spinal curvature in the lumbar spine and thoracic spine may reveal a hemivertebra (Fig. 14.15a, b). These findings often are pain-free initially, but with advancing age the patient may report radicular type of pain, especially in the presence of adeveloping scoliosis in the spine and especially when there is radicular symptomatology.
If there is a significant functional finding, especially in a young person, further radiographic studies are indicated to rule out malformations or space-occupying lesions. In particular when there is unresolved pain, progressive neurologic symptoms, and overt signs, one should strive to correlate these with additional diagnostic findings.
Further Reading
Herman MJ, Pizzutillo PD. Cervical spine disorders in children. Orthop Clin North Am. 1999;30(3):457–466, ix.
Kaplan KM, Spivak JM, Bendo JA. Embryology of the spine and associated congenital abnormalities. Spine J. 2005;5(5):564–576.
Mitchell LE, Adzick NS, Melchionne J, et al. Spina bifida. Lancet. 2004;364(9448):1885–1895.
Fig. 14.14 Arnold–Chiari malformation
a Coronal view.
b Axial view.
Fig. 14.15a Hemivertebra at L3 in this 6-year-old girl who presented with a progressive lumbar scoliosis. b Radiographic follow-up study in the same patient 3 years after surgical decompression and spondylodesis.
Fig. 14.16 Spondyloptosis in a 14-year-old girl.
a Preoperative study.
b Six months after surgical correction and spondylodesis.
Spondylosis, Spondylolysis, Spondylolisthesis, and Spinal Stenosis
Spondylos (Greek) refers to the spinal vertebrae. Spondylolysis refers to the degenerative process in the spinal structures (lysis; Greek “loosening”) refers to a disruption or dissociation of a bony part (e. g., spondylolysis). Listhesis (also Greek) means slippage or sliding. Thus, spondylolysis refers to a fracture or disruption of the pars interarticularis; spondylolisthesis refers to the displacement of one vertebra with respect to another, usually described in the anterior direction. Spondyloptosis (ptosis “dropping”;adjectival form: ptotic) is the “end-result” of spondylolisthesis, where there is complete slippage of the fifth lumbar vertebra with respect to the first sacral segment. Spondyloptosis is associated with severe spinal and postural deformity (Figs. 14.16a, b) and may be associated with neurologic deficits.
The gradation according to Meyerding has been a useful tool for baseline assessment and time-based follow-along/monitoring:
• Grade 1: 0–25%
• Grade 2: 25–50%
• Grade 3: 50–75%
• Grade 4: 75–100%
Spondylolisthesis in the child or young adult is typically due to bilateral or unilateral spondylolysis affecting the pars interarticularis. This spondylolysis is best visualized in standard radiographs (Figs. 14.17, 14.18). The spondylolysis may or may not be associated with a slippage itself. It should be noted that an incidental finding of a spondylolysis does not automatically mean a recent injury or fracture, nor can such a finding be ascribed to recent trauma (e. g., in a motor vehicle accident) if there are no other signs of forceful trauma, for instance (Table 14.9).
Fig. 14.17 Spondylolysis at L5 in a 20-year-old man; observe the typical “Scottie dog” formation in the L4 vertebra, where there is “no collar”. As the pars interarticularis is disrupted in the L5 vertebra, the Scottie dog is “wearing a collar” (disruption of the bony component with greater radiolucency).
Fig. 14.18 Minimal gliding/translation of the fifth lumbar vertebra in this 25-year-old male top athlete.
Classification of Types | Comments |
Isthmic | Most common type of spondylolisthesis Due to pars interarticularis lesion: • Lytic fatigue fracture • Microfracture that healed with elongation • Acute trauma |
Congenital or dysplastic | Dysplastic facets and/or abnormal orientation |
Degenerative | Prolonged segmental instability with associated remodeling of the articular processes at the incriminated vertebrae |
Traumatic | Fracture of the facet, lamina or pedicle Note: The traumatic type of spondylolisthesis refers to a fracture that involves structures neighboring the pars interarticularis |
Pathologic | Bone disease: either localized or systemic/general Examples: • Osteogenesis imperfecta • Paget disease |
The congenital or early-acquired spondylolysis–spondylolisthesis may be amenable to manual therapeutic approaches; that is, these diagnoses are not absolutely contraindications for manipulative approaches. However, a clear diagnosis must be established prior to the application of a hands-on approach, especially when considering thrusting or high-velocity, low-amplitude thrusting techniques.
The first description is vertebral gliding in the absence of significant lesion in the pars interarticularis as presented by Junghans (1931), which he describes as pseudospondylolisthesis. Newman (1965) describes this situation as a degenerative lumbar spondylolisthesis due to degenerative changes, especially in the presence of arthrosis of the intervertebral joints.
If the listhesis is progressive, which is found more frequently after the 5th decade of life, especially in women, the extent can be sufficient to cause a spinal stenosis. The stenosis may be central or foraminal or both. The incidence is known to increase several-fold with advancing age. The greatest incidence of pseudospondylolisthesis is at the L4–L5 and L3–L4 levels (Fig. 14.19). The fact that the intervertebral joints bear up to a 30% of the axial load may be one explanation for the rather early degenerative changes involving these joints (Nachemson, 1960).
The orientation of the facets in the apophyseal joints, especially when aligned in the coronal plane, may also constitute a negative factor. The natural progression of this abnormality reveals that the extent of the gliding associated with the listhesis may reach up to 30% of the vertebral body. Patients who have back pain alone in such a situation may not require surgical intervention. However, the presence of neurogenic claudication with or without radicular symptomatology may be an indication to proceed to operative decompression and/or spondylodesis. Naturally this requires the appropriate diagnostic work-up routines employing the full complement of the appropriate radiographic/neurodiagnostic studies as indicated for the individual patient. It is a reasonable requirement that the conservative treatment should be exhausted prior to consideration of surgical intervention unless the clinical situation dictates otherwise.
Fig. 14.19 Degenerative pseudospondylolisthesis in a 75-year-old man with complete blockage of the contrast material in the myelogram noted at the L3–L4 level. a Myelogram in flexion. b Myelogram in extension.
The conservative treatment should include an individually tailored manual therapeutic approach (mobilization/soft-tissue techniques rather than manipulative thrusting techniques) with an appropriate and well-dosed muscular exercise program to stretch the shortened postural muscles and strengthen the paravertebral musculature (e. g., isometric techniques). As with other disorders, one of the goals of the manual medicine practitioner is to determine relevant adaptive, compensatory, and overcompensatory changes. Once there is muscular insufficiency (e. g., decompensation due to fatigue, structural damage of the stabilizing structures, for instance) and other failure to provide sufficient stability, then manipulative techniques are indicated.
According to the review by Mossaad (2004) radicular pain due to spondylolisthesis or spinal stenosis is much less amenable to the same nonoperative management strategies that are applicable when radiculopathy is related to a herniated disk. Speaking in general terms, Mossaad notes that when there is predominantly leg pain, the course of nonoperative care may require a prolonged period of time to determine if it is efficacious or not. For some patients with leg pain the administration of epidural steroids (ESI, epidural steroid injection) may provide an appropriate temporizing measure.
With regard to surgical intervention, Herkowitz (1995) has formulated the following indications for surgery:
• Persistent or recurring leg pain lasting more than 3 months and refractory to appropriate conservative treatment.
• Progressive neurologic deficits where additional neurologic signs need to be excluded.
• Significant reduction of quality of life.
• Diagnostic substantiation using appropriate studies including CT, myelo-CT, and MRI depending on the individual patient and including neurodiagnostic studies if indicated.
Further Reading
Gibson JN. Waddell G. Surgery for degenerative lumbar spondylosis: updated Cochrane Review. Spine. 2005;30(20):2312–2320.
Logroscino G, Mazza O, Aulisa G, et al. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst. 2001;17(11):644–655.
Mossaad MM. Degenerative lumbar spondylolisthesis with spinal stenosis: natural history, diagnosis, clinical presentation, and nonoperative treatment. In Herkowitz H, Dvořák J, Bell G, et al., eds. The Lumbar Spine, 3rd ed. Philadelphia: Lippincott, Wilkins Williams; 2004:514–522.
van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine. 1997; 22(4):427–434.
Spinal Deformities
The spine can be distorted in any one plane or in all directions or (Fig. 14.20). While there is almost always a rotatory component in the horizontal plane that accompanies the spinal distortions, the most common spinal deformities occur in the coronal and the sagittal planes. Abnormalities in the coronal plane are associated with scoliosis. Changes in the sagittal plane involve the spine’s anterior and posterior relationships.
When sufficiently pronounced, the spinal deformities can be recognized easily by the naked eye, as is the case in thoracic kyphosis, for instance, where a curve of approximately 30° is easily discernible. Minor and even moderate spinal contour changes, especially in the coronal plane, may not be readily apparent upon visual inspection alone and therefore routinely require radiologic assessment. Recent studies (Huysmans et al., 2005) have reported that it may be possible to replace radiographs by surface measurements in order to measure position and orientation of the pelvis. These authors conclude that using certain anatomic landmarks of the back it may be possible to reduce the number of radiographs otherwise employed to measure the position of the pelvis in a scoliotic deformity.
Fig. 14.20 Spinal deformities.
Any and all of the tissues and structures that aid in axial stability can be affected, including the nervous system, muscles, bones, ligaments, cartilage, and other connective tissues. This explains the varied factors that may underlie the various etiologies.
In the pages that follow adolescent kyphosis, often referred to as Scheuermann disease, will be discussed in more detail. Both are very commonly represented. As the name implies, the disease progression occurs most significantly during adolescence until the final stage is reached around the time of maturity. Adolescent idiopathic scoliosis affects girls much more commonly than boys and is relatively asymptomatic. In contradistinction, juvenile idiopathic kyphosis affects boys more commonly and it is often pain that brings the patient to the medical office.
Changes in the Coronar Plane: Scoliosis
Distortions of more than 10° in the coronal plane result in a deformity known as scoliosis. Scoliosis is the appearance of aberrant lateral curves in the otherwise “straight” spine. The most common etiology of scoliosis is idiopathic, with a number of other etiologies forming a rather large spectrum of possibilities. The classification of scoliosis (Fig. 14.21) distinguishes between nonstructural and structural scoliotic distortions and the various subsets. Nonstructural scoliosis is reversible, while structural scoliosis is not reversible. The appearance of a nonstructural scoliosis is in response to postural or other neuromusculoskeletal changes. The structural scoliotic abnormalities are grouped according to more than 10 subsets. The idiopathic adolescent form of structural scoliosis is found more frequently than any of the other entities.
Adolescent Idiopathic Scoliosis
Retrospective review of one scoliosis database showed that while adolescent idiopathic scoliosis is the most common it also felt to represent the least significant variety of spinal deformity (Goldberg et al., 2002a,b) (Fig. 14.21).
In their study of 112 girls (Goldberg et al., 2002a,b), it was shown that the date of menarche is an important factor in the natural history. Furthermore, they noted that braces were prescribed early but were gradually abandoned, and did not increase the study’s surgical rate. Progression of the curve was reported to depend on the age and maturity of the patient as well as the initially presenting Cobb angle. One-quarter to one-third of the patients studied were recommended to undergo surgery. (Goldberg et al., 2002a,b).
Adolescent idiopathic scoliosis becomes apparent in early adolescence, and is often detected through various screening examination routines in the community. Pain is typically not one of the presenting or early complaints. Another common presentation comes with the young patient or the family seeking medical advice when a very minor lateral curvature is noted.
Etiology
As the name implies, the etiology is unknown, although various factors have been incriminated, including genetic, hormonal, neurogenic and myogenic causes. Certainly there exist non-genetic influences, while at the same there are clear genetic components with a sex-linked trait given the prominent female predominance (five to seven times more frequent than boys), or the familial involvement (between 10 to 20 times greater chance of intra-familial involvement),
Biomechanical Considerations
In a scoliotic curvature, the incriminated structures all have a “domino” effect upon each other.
Taking the thoracic spine as an example, the characteristic changes shown in Table 14.10 take place. In contrast to the postural scoliotic curve, the noted deformity has a rather limited involvement, since it usually affects no more than seven to eight vertebrae.
Muscle Fiber Changes
In unbraced patients, a shift in the fiber distribution (from “slow twitch” fibers to “fast twitch” fibers) was observed exclusively at the concave side of the apex. This shift was paralleled by an increased percentage of the intermediate type IIC fibers, which would be indicative of fiber transformation (Meier et al., 1997). In the same study, and in contrast, patients wearing a corset revealed muscle fiber transformation at different levels along the scoliosis, supporting the notion that those muscular changes noted in the apical regions are secondary, rather than being due to specific muscular disorders restricted to the area of the apex. (Meier et al., 1997).
Fig. 14.21 Classification of scoliosis.
| Convexity to the Right | Convexity to the Left |
Vertebral rotation | Vertebrae are rotated to the right (in direction of the convexity): • Transverse processes rotate toward convexity (right transverse process is prominent) • Spinous processes rotate in direction of concavity | Vertebrae are rotated to the left (in direction of the convexity): • Transverse processes rotate toward convexity (left transverse process is prominent) • Spinous processes rotate in direction of concavity |
Intercostal space | Widened on side of convexity (right) | Widened on side of convexity (left) |
Bulging of ribs posteriorly (rib hump) | Side of convexity (right) | Side of convexity (left) |
Thoracic kyphosis | Reduced | Reduced |
Shoulder level | Elevated on convex side (right) | Elevated on convex side (left) |
King I type | Double major curve • Lumbar curve is more pronounced than the thoracic curve |
King II type | Right thoracic and compensatory left curve • Thoracic curve is more pronounced than the lumbar curve |
King III type | Right thoracic curve • Thoracic curve is the major deformity while the lumbar curve does not cross the midline |
King IV type | Right thoracolumbar curve • Major curve that “sweeps” from thoracic to lumbar region |
King V type | Double thoracic curve • Essentially no involvement of the lumbar spine but double curves in the thoracic spine |
Types of Scoliosis Curves
The King classification is one of the more common systems for categorizing scoliosis. Any classification is often an approximation rather than a rigid representation, given the large variability of the presentations (Table 14.11).
More recently Lenke et al. (2001) introduced a new three-component classification system based on the evaluation of standing coronal and lateral radiographs as well as supine side-bending views. The three-component criteria include a description of the curve type, a lumbar spine modifier, and a sagittal thoracic modifier. According to these investigators, this new classification was found to be more reliable than the King classification, but they also noted that further studies are needed to determine the new classification’s accuracy, reliability, and versatility. The system by Lenke et al. appears to underscore the complexity and variability of the different vertebral deformities, with their individual presentations, biomechanical challenges, and different opinions about surgical approach.
Clinical Assessment of Scoliosis
Clinical Presentation
Lateral idiopathic scoliotic deformities in the coronal plane can occur at any age (infantile and juvenile forms), but the most common presentation is the spinal deformity that presents in the younger adolescent girl, at approximately 10 to 16 years of age. Typically the deformity is the reason for the visit, which is often noted in a routine screening examination. When pain is the presenting reason in the young child, one should be sure to rule out any sinister pathology.
Clinical Examination
The detailed history is followed by a thorough examination that relies on the typical components of inspection, a structural and postural evaluation of the entire musculoskeletal apparatus, assessment of leg length, and a thorough neurologic examination. Gait is evaluated in sufficient detail. Recently, Kramers-de Quervain et al. (2004) measured the abnormal gait patterns in their patients with adolescent idiopathic scoliosis (left lumbar and right thoracic curve pattern). While the timing of the individual gait phases and the hip, knee, and ankle motion were all normal with respect to the sagittal plane, it was found that there was significant asymmetry in trunk rotation within the trans-verse plane with respect to a symmetric motion of the pelvis. These authors describe this as torsional offset to the line of progression. The magnitude of offset during the gait cycle correlated directly with the severity of the thoracic deformity and with the standing posture. It was noted, however, that the range of rotational motion was not affected by the severity of the deformity.
The forward-bending test of the trunk is one of the hallmark tests for scolios is as it is very sensitive. Landmark comparisons are equally useful, especially in order to obtain a general overview and for follow-along recordings. Currently the best tool to determine the presence and magnitude of the disease is the standard posterior–anterior radiograph.
Inspection
If sufficiently progressed, a noticeable vertebral rotation or torsion about the longitudinal axis in the horizontal plane is usually seen with scoliosis. The involved vertebral units typically rotate in the direction of the convexity and contribute to the visible prominence of a rib-hump on the same side as the convexity. For instance, with a scoliosis that has a right-sided convexity, the vertebrae are rotated toward the right, where the right rib and right transverse processes are more prominent than on the left. Conversely, the spinous processes move in direction of the concavity. In our example, the motion direction would be to the left side. In clinical practice, however, it should be remembered that the observation of motion behavior of the spinous processes is relatively unreliable and underestimates the degree of rotation, because the vertebral body and transverse processes undergo significantly greater rotation.
Further inspection of the involved spinal region may reveal a less accentuated thoracic kyphosis with an elevated shoulder on the ipsilateral side to the convexity.
The patient’s overall flexibility is evaluated by determining the ranges of motion in the cervical, thoracic, and lumbar regions, including flexion/extension, side-bending, and rotation.
A focused neurologic examination, including a detailed motor-sensory assessment, should be performed, not only in the initial examination but also routinely in periodic check-ups.
Again, it is emphasized that the typical presentation of adolescent idiopathic scoliosis is not associated with pain. If considerable pain is reported spontaneously or is the precipitating reason for the medical visit, the history and examination should be careful in ruling out the possibilities of space-occupying lesions, inflammatory or auto-immune disorders, a tethered spinal cord, or other sinister pathology.
Motion Testing; Trunk Forward-Bending Test
The patient is requested to stand with the medial malleoli touching each other and the knees extended. With the hands together in front, both palms and fingers touching each other, the patient is then requested to bend forward from the waist. The scoliotic curve becomes most prominent when the patient bends forward. This maneuver is known as the forward-bending test of the trunk. The test is quite sensitive test and thus clinically very useful.
Landmark Measurements
A scoliometer can be utilized to measure the extent of the rib hump that is tested during the motion testing in the forward-bending test of the trunk.
The levels of the trochanteric heights in comparison to the levels at the iliac crest, the lower costal margin, and the shoulders are valuable landmarks for recording postural abnormalities.
There may also be a functional or structural leg length discrepancy, which should be noted during structural–functional examination.
The spatial relationships between trunk and pelvis are best visualized by comparing the body posture against the plumb line, which is aligned with the seventh cervical vertebra, which in typical situations should be the most prominent vertebra. However, this may be confirmed by specific segmental motion testing because the first thoracic vertebra can be the most prominent.
Studies by Huysmans et al. (2005) assist in the objective verification of observable changes. The future usefulness of routine clinical practice is yet to be determined.
Radiographic Evaluation
Standard radiographs consisting of both the postero–anterior (PA) (13in. × 36 in. cassette) and lateral views, which should include the cervicothoracic junction and the lumbosacral junction, and should be done with the patient standing. Care must be taken to minimize radiation exposure to the gonads and the breasts. It may sometimes be helpful to obtain views while the patient side-bends in order to determine the rigidity of the thoracolumbar spine.
Based on the radiographic study, one is able to determine the Cobb angle (Fig. 14.22). This angle is measured by the intersection of two lines, upon which perpendicular lines are constructed: (1) one line follows the superior end plate of the uppermost involved vertebra of the scoliosis; and (2) the other line follows the inferior end plate of the most inferior involved vertebra.
The Cobb angle is then recorded and used as baseline for any future follow-up studies to determine the progression of the curve.
Treatment of Scoliosis
Treatment for scoliosis is principally divided into nonoperative and operative care. In nonoperative approaches, the mainstay components are a “wait-and-see” observation period, the application of orthoses or braces, and exercise. Despite various empirical claims, manual medicine techniques or approaches have not been shown to halt or even reverse the progression of a structural scoliosis. When they are applied, the major goal is to address the regional specific segmental changes that have adapted or compensated in response to the associated scoliosis. This may include the region neighboring directly above or below the scoliosis, as well as regions quite distant from it. Another goal is to address the associated muscular changes, in an attempt to normalize the balance between the tight or shortened primarily tonic muscles and strengthen the weakened, primarily phasic muscles.
Nonoperative Treatment
Nonoperative treatment consists of the following three mainstays of treatment:
1. Wait-and-see observation.
2. Orthotic management—bracing.
3. Exercise.
Wait-and-See Observation
• 20–25°—follow with serial radiographs every 6–12 months (skeletally immature patient).
• If the curve changes by more than 5° (initial curve is 20° or greater), this should be followed up by spine surgeon.
Orthotic Management: Bracing
The use of different orthoses to correct spinal deformities in one way or another has been an accepted practice in the standard orthopedic armamentarium. Howard et al. (1998) in their retrospective cohort study of 170 patients who had been fitted with different braces found the thoracolumbosacral (TLS) orthosis to be superior in preventing curve progression in adolescent idiopathic scoliosis to the Milwaukee or Charleston braces.
More recently, the effectiveness of braces has been questioned. Goldberg et al. (2002a,b) conclude that if bracing does not improve prognosis significantly, its efficacy cannot be accepted. In a study of 136 patients (Ugwonali et al., 2004), it was shown that brace wearing did not decrease the quality of life of adolescents compared with their observed counterparts who had not been fitted with braces.
A recent study (O’Neill et al., 2005) suggests that over-weight patients with adolescent idiopathic scoliosis will have greater curve progression and less successful results following orthotic treatment than those who are not over-weight. The same authors conclude that the ability of an orthosis to transmit corrective forces to the spine through the ribs and soft tissues may be compromised in over-weight patients. This factor should be taken into consideration when making treatment decisions. Additional study is warranted to determine a threshold effect.
Exercise
Exercise is used as an adjunct to minimize potential compensatory changes, regionally or globally, by trying to keep the spineas flexible and strong (“stable”) as possible.
Exercises have not been shown to prevent the progression of an already existing or newly developing curve.
Electrical Stimulation
While historically a number of smaller-sized studies have supported the use of electrical stimulation, a well-designed study found no statistical difference in outcome between patients in the electrical stimulation treatment group and those who had no treatment at all (O’Donnell et al., 1988).
Surgery
Once surgery is indicated, there are many surgical techniques, approaches, and hardware options available with encouraging innovations. Wiggins et al. (2003) point out that the classifications and treatments of pediatric spinal deformities have evolved since the distraction instrumentation introduced by Harrington. Surgical approaches ranging from anterior-spine instrumentation systems and segmental fixation to the recently introduced the pedicle screw-augmented fixation approach demonstrate the evolution. According to these authors, the pedicle-augmented fixation approach promises to shift, once more, the standard of surgical therapy.
Fig. 14.22 Measurements used in the evaluation of idiopathic scoliosis, employing the angle method of Cobb. The angle is measured as follows:
1. Draw a line along the superior surface of the uppermost involved vertebra.
2. Draw a line along the inferior surface of the lowermost involved vertebra.
3. Construct perpendicular lines onto the lines constructed in steps (1) and (2).
4. Measure the angle with respect to the horizontal.
Note: The rotation of the vertebrae can actually “move” beyond the involved region.
The primary goals of treatment are as follows (An, 1998):
1. Prevention of curve progression.
2. Maintenance of balance: if the patient is to undergo surgery, spine and pelvic balance are more important than curve correction.
3. Maintenance of respiratory function.
4. Reduction of pain and preservation of neurologic status.
5. Cosmesis.
Natural History of Scoliosis: Factors Contributing to Curve Progression
A number of variables have been incriminated in contributing to the progression of the scoliotic curve. There is an increased risk associated with sex, as females are affected more frequently.
There is clearly a greater risk of progression in curves of greater magnitude at time of first presentation. For instance, a 20° curve is at lesser risk of progress than a 45° curve. Skeletal maturity as correlated with the patient’s age is a significant contributing factor: that is, the younger the patient the greater the risk of curve progression.
Progression
Studies of the natural history of adolescent idiopathic scoliosis reveal that a number of factors are of predictive value in assigning risk for progressive curvature and subsequent deformity and/or morbidity (Gunnoe, 1990). These include the age at the time the diagnosis is first made, the stage of skeletal maturity, and magnitude and pattern of curvature (Cobb angle). A recent study confirmed these prior notions, supported by the specific findings in a subgroup that had actually discontinued bracing (Goldberg et al., 2002a,b).
The goal in scoliosis surgery is to reduce curvature and to create a stable framework on which vertebral fusion can occur so as to reduce curve progression and to minimize or prevent secondary changes such as respiratory complications.
Changes in the Sagittal Plane: Kyphosis and Lordosis
Spinal deformities in the sagittal plane result from distortions of the normal anterior–posterior relationships of the spinal curve. Any direction can therefore become exaggerated, resulting in either an exacerbation or flattening of what otherwise would be considered a normal kyphosis in the thoracic spine, or lordosis in the cervical and lumbar spine (Table 14.12).
Postural | |
Scheuermann disease |
|
Congenital | • Defect of formation • Defect of segmentation • Mixed |
Neuromuscular | |
Myelomeningocele | • Congenital (present at birth) • Developmental (late paralytic) |
Traumatic | |
Postsurgical | • Postlaminectomy |
Postirradiation | • Neuroblastoma • Wilms tumors |
Metabolic | • Osteoporosis • Osteomalacia • Osteogenesis imperfecta |
Skeletal dysplasia |
|
Collagen disorders | Marie–Strümpell disease |
Tumors |
|
When standing erect, the sagittal plumb line should ideally cross the individual’s cervicothoracic (C7–T1) and thoracolumbar junctions (T12–L1). Thus, when viewed from the side, the anterior convex curve (lordosis) in the cervical and lumber spine may become more pronounced or more flattened. In the thoracic spine, the posterior convex curve, the kyphosis, can become prominently accentuated or reversed. Senile kyphosis, adolescent postural round back, and Scheuermann disease are examples of an abnormally increased thoracic kyphosis. Exaggerated kyphosis may be smooth and continuously rounded, as is typically seen when several adjoining vertebrae are involved. An angular formation, described as a gibbus (Latin “hump”) deformity, is more typical of vertebral collapse due to osteoporosis and associated fracture, neoplasm, or infection.
Scheuermann Disease: Juvenile Scoliosis
This disease represents an accentuation of the normal thoracic kyphosis with adaptive changes in the cervical and lumbar spine secondary to anterior wedging of the vertebrae in the adolescent. It is a growth disorder that involves several vertebrae and leads to an overall loss of flexibility in the involved spine secondary to developmental abnormalities in the cartilaginous end plate. In Scheuer-mann disease there are abnormal vertebral pressure relationships with: (1) abnormal compressive loading abnormalities anteriorly disrupting end plate function and thus stunting normal growth; and (2) increased posterior tension stress leading to hypertrophy. Thus a vicious cycle is being set up. In addition to changes seen in the cartilaginous vertebral end plate, such as irregularities and Schmorl’s nodes, and compression of the vertebral body, there is later disk prolapse, all of which again contributes to the anterior wedging of the vertebrae.
Etiology
Although the etiology remains unknown, various factors have been incriminated including endocrine factors (growth disturbance during puberty), familial and congenital factors (assumed), nutritional factors (nontropical sprue), and postural abnormalities associated with mechanical abnormalities. The latter, however, are probably the consequence of the vertebral changes rather than being a causative factor.
Pathogenesis
The underlying pathology is thought to involve developmental abnormalities of the cartilaginous end plate. With disruption of the end plate, there is stunted vertebral growth and a shift in load sharing with wedge-shaped abnormalities.
The shape changes associated with continued abnormal load is summarized by the Hueter–Volkmann law of physeal growth. With a narrowed intervertebral disk, there is increased anterior loading. Also observed is a thickened and tightened anterior longitudinal ligament. Disruption of the intervertebral disk and vertebral end plates may result in penetration of the vertebral body by disk material. This is thought to lead to the formation of Schmorl’snodes, a phenomenon readily visible on radiographs. Continued abnormal loading stress may lead to structural change of the entire vertebra, which changes shape from a rectangular outline (lateral view) to wedge-shaped, with the anterior portion significantly narrower than the posterior portion.
Thus, the formation of the kyphotic posture is due to a mismatch between the anteriorly narrowed and posteriorly maintained vertebral height.
Clinical Presentation
The adolescent presents to the office primarily for two reasons: (1) the noticeable deformity; and/or (2) the presence of pain in up to half of the patients. Pain presentation is more typical for patients who have lumbar spine involvement. Again, this is different from the adolescent idiopathic scoliosis, which typically does not present with initial pain unless there is a concomitant co-morbidity or sinister pathology present.
There may be a history where the deformity had been noted for some time and had not responded to a self-initiated exercise program. One of the frequent parental complaints is that their child is unable to stand up straight, unable to assume a good “military position.”
Examination
The patient’s thoracic kyphosis is exaggerated. Normal thoracic kyphosis ranges between 20° and 45°.
There may be adaptive or compensatory hyperlordosis of the lumbar spine.
Neurologic examination is usually unremarkable unless severe progression or significant pain is reported, requiring further work-up in some cases.
No special tests are necessary.
Radiographic Examination
The lateral radiograph and the postero–anterior view of the entire thoracic spine together provide the diagnostic clues to substantiate the diagnosis:
1. Exaggerated thoracic kyphosis measuring more than 45° (using Cobb angle measurement techniques) with noticeable anterior wedging of at least three adjacent apical thoracic and/or lumbar vertebrae. The wedging should measure at least 5° or more.
2. Irregular appearance of the vertebral end plate.
3. Schmorl’s nodes.
Differential Diagnosis
• Ankylosing spondylitis.
• Fixed kyphotic deformity due to paralysis.
• Inflammatory changes affecting the spine.
• Neurofibromatosis.
• Postural kyphosis (radiographic findings are typically minimal).
• Space-occupying lesions of the spine.
• Tuberculosis of the spine (Pott disease).
• Vertebral fracture (trauma, metabolic disorder).
Treatment
Similarly to the treatment of adolescent idiopathic scoliosis, the conservative treatment relies on exercise and orthotic prescription/bracing while keeping a watchful eye on the potential progression. Especially recommended are swimming and guided extension exercise regimens coordinated with pelvic tilt exercises and abdominal strengthening. Maintaining as much flexibility in the spine as possible, including the adjoining regions, should be a central goal. Also, stretching of the pectoralis muscle is indicated as they are often shortened.
Manual medicine approaches have not been reliably shown to arrest curve progression, especially if advanced. However, an individually tailored program to maintain flexibility of the tonic, and typically shortened, muscles is of importance. Treatment should also address the compensatory changes associated with the primary disorder, which may be in areas quite distant from the kyphosis, e. g., upper cervical spine or lower limb, especially if associated with tight hamstrings, for instance.
If the patient is skeletally immature and the curve is greater than 50°, treatment utilizes a Milwaukee brace until maturity is reached (Frymoyer, 1993).
Surgical intervention is indicated when there is intolerable pain, neurologic deficit, and/or severe deformity with curves measuring more than 75°. A trial of bracing may have been utilized as a “last conservative attempt” measure prior to proceeding with surgery.
The surgery involves anterior release and spinal arthrodesis, or posterior arthrodesis with instrumentation to accomplish permanent correction (Frymoyer, 1993).
Clinical Disorders and Syndromes of the Upper Limb
General Comments
The upper limb comprises the shoulder–elbow–wrist complex, and functionally should be viewed as one mobile unit. Mobility is favored over stability, especially in the shoulder, which is the most mobile of all of the joints in the human body (Kapandji, 1982).
Upper limb function is viewed as a four-phase process that includes the following specific components:
1. Reaching
This activity allows placement of the hand upon the desired spatial target.
2. Carrying
This activity, like reaching, allows placement of the hand upon the desired spatial target while at the same time securing transportation of an externally applied load.
3. Prehension patterns
This activity is a description for hand function, which consist primarily of three components, namely, pinching, grasping, and hooking.
4. Releasing
After holding an object with one’sfingers, the voluntary release of the held object is the final action in hand function. It is accomplished by the extensor action of the thumb and fingers, and little active strength is required for the release. However, if release cannot be initiated actively within the desired parameters, hand function is severely impaired if not rendered ineffectual.
Beyond this four-phase activity, the use of the hand is what gives life to the majority of the expression of our cognitive and creative activities: the hand serves as the most versatile “translator” of our thoughts in a most efficient manner, be it in showing through gestures, writing with a pen or computer, composing on a musical instrument, or changing a blank canvas into a painted landscape.
It is through the use of the hand and the act of disciplined “touching someone” that the physician communicates directly and professionally with the patient, affecting changes that might not be accomplished simply through the spoken word. In this sense then, the physician who uses his or her hands judiciously in the diagnostic and therapeutic process acts within the context of holistic (“whole-istic”) care and caring and, when fortunate, even some curing. Indeed,
“wearemoreconnectedthanwehavebeenledtobelieve.”
Below, common disorders of the upper limb are presented as encountered in clinical practice. The goal is not to be exhaustive in all aspects for all disorders known, but rather to present a coherent overview that allows integration into one’s management of those disorders when they are encountered in musculoskeletal and manual medicine practice.
The Shoulder
Common Shoulder Disorders
The following common shoulder disorders are described in this section:
• Disorders associated with humeroscapular periarthropathy complex:
– Common rotator cuff tendinopathy (tendinosis).
– Rotator cuff tear.
– Calcifying tendinitis.
– Adhesive capsulitis.
• Glenohumeral arthritis.
• Arthrosis of the acromioclavicular joint.
• SLAP lesions.
• Shoulder (glenohumeral) instability.
Common Rotator Cuff Tendinopathy (“Tendinosis”)
Synonyms and Related Terms | • Common or uncomplicated humeroscapular periarthropathy. • Rotator cuff impingement. • Rotator cuff injury. • Rotator cuff tendonitis/tendinosis. • Shoulder impingement (internal) syndrome. • Shoulder pain. • Swimmer’s shoulder. |
Key Points | • Degenerative changes of rotator cuff with tearing, usually due to overuse. • Frequently due to or associated with impingement syndrome, in particular with a curved acromion, and resulting from a vicious cycle of use-irritation–impingement–tear–re-use… • Progressive course may be demonstrated in patients as early as 30–40 years of age. • Pain typically upon movement or against resistance; possible night pain. • Painful arc—between 70° and 120° of abduction and forward flexion. Clinical Pearls • Remember that not all full-thickness tears are painful. • Up to one-third of patients with rotator cuff tears may have no pain. • Consider the subacromial bursa as source of pain due to the significantly higher number of nerve endings in the bursa. • Consider the cervical spine as a source of referred pain (spondylosis, disk herniation, spinal stenosis, muscle imbalances). • Patients may report night pain. • Utilize the Neer and Hawkins/Jobe tests. • Utilize additional manual medicine examination techniques in the parascapular region and look for compensatory body changes elsewhere. • Lidocaine injection to the subacromial bursa may give some relief (confirms impingement). • Treat the entire patient (vocational and avocational goals). |
Prevalence | • Peak age: 40–45 years. |
Pathology/Etiology | • Degenerative tendon changes resulting from overuse or trauma • Thickened tendon narrows the otherwise free passage at the anterior acromion and coracoacromial ligament. • May involve any portion of the tendon as partial or complete tears. • Tendinotic changes (“tendinosis”) typically in absence of signs of inflammatory reaction. • Thus the preferred term is “tendinosis” rather than “tendonitis.” • Consider subacromial bursa involvement, especially in light of it having significantly more free nerve endings (10–20 times more) compared to the cuff tendon (Vangsness et al., 1995). |