Chapter 4
Seating Systems as Enablers of Function
On completing this chapter, you will be able to do the following:
1. Identify the potential outcomes of seating for postural control, tissue integrity, and comfort
2. Describe a comprehensive seating assessment
3. Describe key biomechanical principles related to sitting and seating technologies
4. Describe the principles of seating for postural control
5. Describe the factors that contribute to the development of pressure ulcers
6. Describe the different characteristics of seating materials
7. Discuss the different classifications of materials used to construct seats
The first part of this chapter describes the needs served by seating systems, evaluation of individuals for seating, and biomechanical principles related to seating. The remainder of the chapter provides in-depth information on each of the three categories of seating needs (seating for postural control, tissue integrity, and comfort), including related principles and the technologies used for intervention. Seating components are typically used with some type of mobility base. For purposes of this text, however, these two systems are separated. Mobility is viewed as a specific-purpose extrinsic enabler (see Chapter 12).
Overview of needs served by seating
Three distinct areas of seating intervention have emerged, each serving a particular consumer need. These three categories of seating intervention are (1) seating for postural control, (2) seating for pressure redistribution, and (3) seating for comfort.18
The third category of seating addresses the need to improve an individual’s level of physical comfort through postural accommodation. Persons in this category include the elderly, individuals with limited endurance for walking (e.g., people with cardiac or pulmonary conditions), and individuals with amputations or arthritis. They may or may not use a wheelchair on a regular basis and typically have normal or near-normal sensation; however, any prolonged sitting causes discomfort from which they are unable to obtain relief. Therefore, they have unique needs and are not completely served by either category previously described. Specialized seating can help to alleviate this chronic discomfort and maximize function. Box 4-1 shows some of the potential outcomes of seating intervention for these populations.
Evaluation for seating
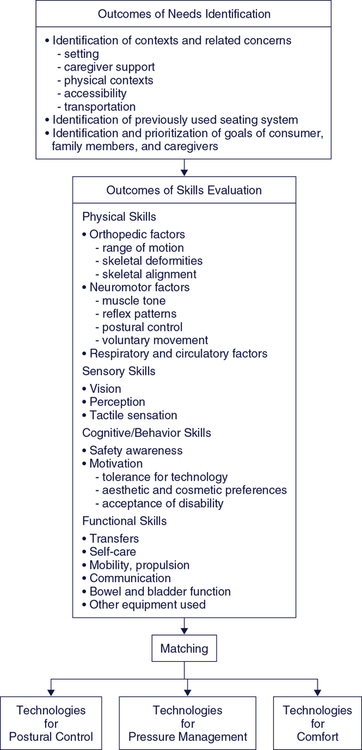
The process of assessing individuals for the purpose of recommending seating technologies requires a systematic method that includes consideration of many factors. The discussion of the design of an assistive technology system in Chapter 2 gave a general framework to guide assessment. The purpose of this section is to describe the factors that are considered when evaluating a client for seating technology. Figure 4-1 depicts a framework showing the process of this evaluation. The rehabilitation assistant’s role in this process is to provide information about the client’s daily activities, physical and cognitive function, and emotional state, particularly noting any changes that might affect the client’s seating needs.
Overview of Assessment Process
The first element of the HAAT model requires the team to understand the activities in which the client wants or needs to participate. Figure 4-1 lists the desired outcomes of the identification of needs. An ATP is usually responsible for completion of the assessment to determine seating needs and the most appropriate technology recommendation. However, others provide important information to support this information. Any assessment with the goal of identifying seating needs and recommended technology starts with discussion of the occupations the user wants and needs to complete while using the seating system. A general measure such as the Canadian Occupational Performance Measure28 provides a systematic means of discussing key occupations in the areas of self-care, productivity, and leisure. There are some measures that are specific to seating and wheeled mobility, including the Functioning Everyday in a Wheelchair measure37 and the Wheelchair Outcome Measure,34,38 that consider function in self-care, productivity, and leisure specifically from the view of an individual who uses seating and mobility devices.
Human Factors
Physical Skills or Mat Assessment
The physical evaluation includes assessment of orthopedic factors, postural control, and respiratory and circulatory factors (see Figure 4-1). It is recommended that evaluation of physical skills take place with the person both in a sitting position and supine on a flat surface such as a mat.
Musculoskeletal Factors
Orthopedic evaluation involves measurement of joint range of motion and assessment of skeletal deformities and skeletal alignment to determine optimal angles for sitting. Obtaining information regarding limitations in range of motion and deformities is necessary to determine whether the goal of the seating system will be to prevent deformities, correct deformities, or accommodate deformities.55
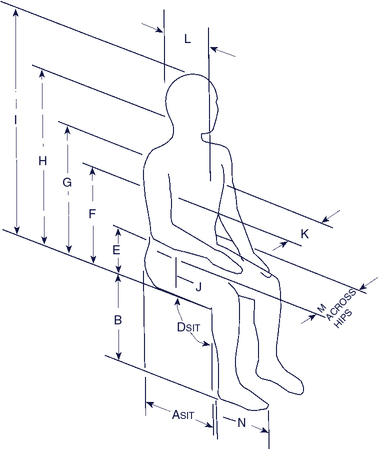
Starting with the consumer supine on the mat, mobility of the lumbar spine and pelvis are assessed, followed by range of motion measurements of the hips, knees, ankles, upper extremities, and neck. Joint angle and body measurements as shown in Figure 4-2 are made at this time. Alignment of the individual’s head, shoulders, and trunk with the pelvis is determined next. Range of motion and skeletal alignment should also be assessed with the individual in a sitting position to determine how the body parts are affected by gravity. Bergen, Presperin, and Tallman (1990) describe in detail a process for measuring joint angles and assessing skeletal alignment.
Postural Control
The client’s sitting ability is described by the amount of support required to maintain a seated position. Hands-free sitters are those who do not need to use their hands to support themselves to maintain sitting, whereas hands-dependent sitters do need to use their hands. These individuals could not perform a seated activity using the hands without some type of external support. A dependent sitter does not have sufficient motor control to support herself in sitting at all. A dependent sitter (or propped sitter) requires more support from a seating system in order to maintain the sitting position.54Box 4-2 defines these levels of postural control.
The amount of external control required to assist an individual to maintain a seated position is an important determination. Kangas (2006)24 recommends that only the minimal amount of external support needed by the client to remain in an upright position be used. This strategy enables the client to use the postural control they have and also gives them freedom of movement that they wouldn’t have when held more tightly with straps. Support may vary with the activity. Less support may be needed when the individual is engaged in a sedentary activity, such as watching television. Alternatively, more support is needed when the individual is using his hands for an activity and the focus of attention is on the activity. The individual should not need to divert attention to the maintenance of posture when engaged in an activity.
Psychosocial Factors
The meaning that technology holds for the individual is an important factor to explore with the user, although it is more significant for the mobility component of a seating and mobility system (see Chapter 12). Many clients prefer technology that does not draw attention to a disability. This preference will be a factor in the selection of a seating system. Aesthetics, or the appearance of the device, is an important factor in acceptance or rejection of the technology.36,4 Behavioral problems, such as an agitated person who throws himself against the back of the chair, can also present a safety problem that needs to be addressed. Working together with the consumer and the caregiver to address these concerns is essential.
Environmental Considerations
Physical Context
Institutional Context
Funding implications are a key institutional consideration. General considerations with respect to funding were described in Chapter 3. The ATP has the responsibility for providing the necessary documentation to secure funding but may rely on the rehabilitation assistant to provide important information about the client’s function to include in the documentation.
Another type of legislation has unique implications for seating products: the use of restraints. The Centers for Medicare and Medicaid Services define a restraint as “any manual method or physical or mechanical device, material or equipment attached or adjacent to the resident’s body that the individual cannot remove easily which restricts freedom of movement or normal access to one’s body.”9 Certain legal jurisdictions have legislation that regulates the use of restraints with individuals residing in institutional settings. The intent of this legislation is to limit inappropriate use of restraints, such as tying an individual into a chair simply to prevent him or her from moving around. This legislation has implications for the use of straps, pelvic belts, and sub–anterior-superior iliac spine (ASIS) bars, trays, and tilt systems (as part of the wheelchair set up) that are used in seating systems for positioning and safety reasons. The legislation typically regulates how restraints are used in institutional settings, requiring most institutions to have a plan and a documented process when restraints are used. Box 4-3 provides information on what to look for in an institution’s guidelines and care plan concerning restraint use.1,44 The rehabilitation assistant should be familiar with the restraint use policies of the institution, how these policies affect their practice, and what is required of them when interacting with a client whose seating system includes elements listed above that are considered to be restraints.
Restraints are frequently used to prevent falls. However, there is little evidence to suggest their use actually does result in any significant reduction in the incidence of falls.53 The rehabilitation assistant should monitor the client for any adverse outcomes to the use of restraints. These outcomes include increased agitation if the client becomes upset by the restriction of movement, redness, skin abrasion or pressure ulcer formation, or undue limitation of functional activities if the client’s movement is overly restrained by seating components.
Matching Device Characteristics to a Consumer’s Needs and Skills
The final component of the evaluation process involves the matching of the client and the technology. Box 4-4 lists a number of questions that are important in the determination of whether the recommended technology is appropriate. Because the rehabilitation assistant engages with the client for several hours a day, over several days, she is in an excellent position to provide information that contributes to the evaluation of the technology as it is used by the client. The rehabilitation assistant can observe the client over time to determine if he is able to maintain a functional position that is comfortable and minimizes the risk of pressure ulcer development. She can observe the client if various daily activities and note whether the seating technology enables their performance in these activities. Interaction with the client over the long term can provide information on whether the technology is sufficiently durable and flexible to meet the client’s changing needs. Finally, interactions with caregivers provide important information about their ability to cope with caregiving demands, including their ability to use and maintain the seating technology.
Biomechanical principles
It is important for the rehabilitation assistant to understand some of the aspects of body position and movement when they position a client in their seating system and interact with that client during the day. Biomechanics is the study of body position and movement. This section presents the major concepts of biomechanics that are fundamental to an understanding of seating and positioning systems for persons with disabilities. There are additional aspects of biomechanics that are pertinent to this area. A lengthier discussion of relevant biomechanical principles can be found in Cook and Polgar (2008).13
Kinematics: Study of Motion
There are two fundamental types of displacement: linear and rotational. When all parts of a body move in the same direction, at the same time, and for the same distance, the movement is linear.30 For example, a person generates translational movement when walking. Displacements caused by external positioning components can also be translational. If the direction, distance, and time of the movement occur simultaneously, but the movement is through an angle instead of in a straight line, the movement is called rotational. Rotational movements occur around an axis called the fulcrum. The majority of body movements are rotational, such as hip or elbow flexion and shoulder flexion or extension. Some positioning components cause rotational displacements (e.g., reclining the back of a wheelchair causes rotation at the pelvis and hip).
Kinetics: Forces
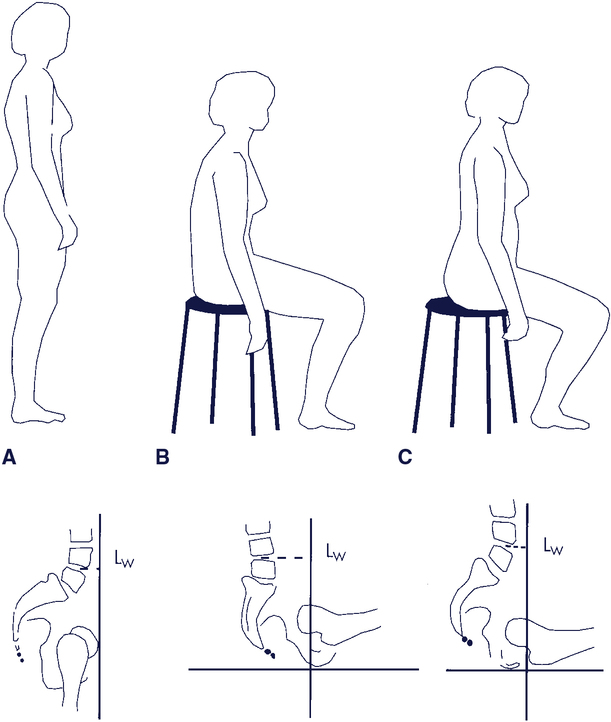
Force is a major element in both biomechanics and seating for individuals with disabilities. Force is anything that acts on a body to change its rate of acceleration or alter its momentum.30 It is described by both magnitude and direction.49 Forces always occur in equal and opposite action-reaction pairs between bodies. Forces can be applied to the body internally or externally. Internal forces are generated inside the body, such as muscle contractions that cause movement of the joints. Externally applied forces (such as the shearing of skin against the wheelchair cushion during transfers) come from outside the body and act on it in some way. One example is the forces applied by a support surface and components of a seating system such as lateral supports. The force resulting from the acceleration of gravity is another external and ever-present force that acts on the body and influences its posture and movement.49 This force on the body acts along a line called the gravitational line, and its effect is localized around a point in the body called the center of gravity. The center of gravity changes as posture changes from standing to sitting and in different sitting positions. Figure 4-3 shows the change in the position of the center of gravity with different positions.
The four properties of force ultimately determine its result. These properties are magnitude, direction, line of application, and point of application. Magnitude is the amount or size of the force measured in newtons, pounds, or kilograms. Forces are applied in some direction, either pushing or pulling, and are applied along a particular line of application. The force acts at a particular point on the body, called the point of application.30
Newton’s Laws of Motion
The English scientist Sir Isaac Newton formulated three laws relating to forces on bodies at rest and in motion. Newton’s first law states that a body at rest tends to remain at rest and that a body in motion in a straight line tends to remain in motion, unless external forces act to change either of these states. In other words, a body likes to continue what it is doing, whether moving or resting. This law defines inertia. Newton’s second law defines force. Force is equal to mass (in kilograms) multiplied by the acceleration of the object (force = mass × acceleration). This means that the greater the force, the greater the acceleration; or, conversely, the greater the mass for the same force, the smaller the acceleration. Newton’s third law states that if one body exerts a force on another, there is an equal and opposite force, called a reaction, exerted on the first body by the second.30 This law is applied to seating systems with the assumption that every force exerted by the human body while sitting in a wheelchair or seating system is balanced by an opposite force exerted by the sitting surface on the person.49 The force generated by the body is equal in magnitude and opposite in direction to the force generated by the seating system, a state often referred to as equilibrium. When a body is at rest and all internal and external forces are balanced, the body is then in a state of static equilibrium. When forces are balanced around a body during movement, resulting in a constant velocity, it is described as a state of dynamic equilibrium. Both types of equilibrium are important in seating and positioning systems.
Friction
Frictional forces exist between two bodies in contact moving in opposite directions.49 These forces result in resistance to movement between the two bodies. Two types of friction are defined: static friction and dynamic friction. Static friction is that force that must be overcome to start a body in motion. Static friction is proportional in magnitude to the perpendicular (compression) force holding the two bodies together. Static friction is independent of the area of contact between the two bodies. Once motion is initiated, the resistive force is generally smaller than when at rest, and it takes less force to keep the bodies moving relative to each other than to start movement. Friction during movement is called dynamic friction. Both of these frictional forces are affected by surface conditions such as moisture, heat, texture, and lubricants, and both are important considerations in the recommendation, design, and on-going evaluation of seating surfaces.
Sitting Posture and Center of Pressure
Two constructs are important to consider when discussing postural control: center of gravity and center of pressure. The location of the center of gravity is fairly well defined in the standing position. Its location is described as passing through the mastoid processes of the jaw, a point just in front of the shoulder, a point just behind the center of the hip joints, a point just in front of the center of the knee joints, and approximately 5 to 6 cm in front of the ankle joints (Figure 4-3). In this posture the pelvis is in a neutral position and there is a natural lordosis of the lumbar spine.59 The location of the center of gravity in sitting is more difficult to determine, but it is usually considered to be lower, with the buttocks and thighs forming the base of support. The individual must maintain the center of gravity over the base of support to maintain an upright posture in either sitting or standing. Seating interventions for postural control assist the client to keep the center of gravity within the limits of the base of support.
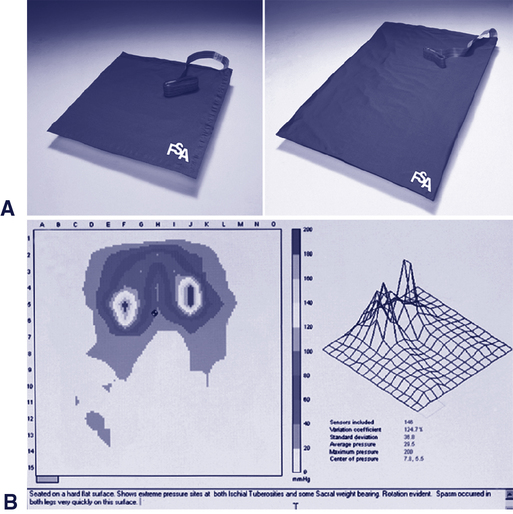
Typically, the center of gravity is defined by its position in the frontal, lateral, and coronal planes. However, in the clinic we are only able to capture the location of the center of pressure location in the frontal and lateral planes. This location can be identified and monitored in the clinic by using a pressure mapping system (see Figure 4-16). These systems use various technologies to monitor the pressure between the individual and a support surface (i.e., between the client’s buttocks and thighs and the seat cushion). They are most commonly used to show pressure distribution when pressure redistribution cushions are evaluated, so their function will be described in greater detail in that section.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree